You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
Dental caries is the most common chronic disease in childhood and represents a significant public health concern.1 Early childhood caries (ECC) is defined as affecting the dentition of children <72 months old.2 Disparities in ECC are evident, and rates are associated with the social determinants of health (ie, family income, immigrant status, areas of social deprivation, etc.).1-3
The period from preconception to approximately age 3 is a critical window for caries prevention efforts.4 Children can acquire caries-related bacteria from their primary caregivers during the first 3 years of life, and it becomes more difficult to change the oral environment and prevent dental disease without significant professional interventions after this window of infectivity closes. Thus, the very early childhood period is a critical time for early identification of risk factors and early intervention to help change the trajectory of a child’s oral health.
Many professional associations involved in pediatric care advocate early oral health visits as a public health strategy to promote population oral health and to reduce the prevalence of ECC. The Canadian and American Academies of Pediatric Dentistry and Pediatrics recommend that children establish a dental home by age 1.5-7 The American Academy of Pediatric Dentistry defines a dental home as “the ongoing relationship between the dentist and the patient, inclusive of all aspects of oral healthcare delivered in a comprehensive, continuously accessible, coordi-nated, and family-centered way. Establishment of a dental home begins no later than 12 months of age and includes referral to dental specialists when appropriate.”8 Research conducted in the United States has demonstrated that providing dentists with training in the management of very young children and in family-centered dental care can increase dentists’ confidence and their willingness to provide services.9,10 However, little research has been conducted regarding early oral health visits in Canada and this study aims to explore this translation of research to practice gap.
The Baby Oral Health Program (bOHP) was developed in North Carolina and has been implemented in other states in the United States. Its mission is “to educate dental healthcare providers on the principles of infant and toddler oral health in order to equip them with the necessary tools to be comfortable and competent at providing preventive oral health services for young children.”11,12
The purpose of this study was to conduct a pilot evaluation of the bOHP program in a Canadian community setting. The specific objectives were to examine the impact of this intervention on dental providers’ practice knowledge, values, confidence, and practice behaviors regarding providing oral healthcare to young children (<3 years), and to assess the feasibility and satisfaction of the bOHP among dental providers in a community setting. This study employed a mixed methodology prospective quasi-experimental design with a 1-, 3-, and 6-month follow-up. This paper focuses on findings between the pre- and post-test. Findings for the follow-up assessments (3 and 6 months) are presented for descriptive purposes only.
METHODS AND MATERIALS
Sample
A master list of dental practices in a southwestern community in Ontario (n=61) and their corresponding contact information was obtained from the Royal College of Dentist Surgeons of Ontario (RCDSO). All registered practices received, via postal mail, an invitation to attend the intervention workshop titled “Family-Centered Dental Care: Treating Infants & Toddlers in Your Practice.” Follow-up telephone calls were made 1 week after the invitations were mailed out, and a second invitation was either hand-delivered, faxed, or e-mailed to the offices that indicated they had not received the original mailed invitation.
Control participants were recruited by comparing the master list of dental practices originally obtained from the RCDSO with the attendance list from the workshop to identify those dental practices that did not participate in the intervention. A convenience sample of those remaining dental practices were sent a letter via postal mail, followed by a telephone call 1 week later explaining the study and inviting them to participate. Researchers randomly sampled practices until the sample size was approximate to the intervention group. All dental professionals participating in patient care (ie, dentists, dental hygienists, dental assistants, etc.) were invited to attend the workshop and all participants (intervention and control groups) received a $15 gift card as a token of appreciation for their participation in the study.
Intervention
The intervention consisted of a 1-day workshop (4.5 hours) and a take-home personal bOHP kit. The kit consisted of a binder containing information and tools (ie, DVD, flip chart, clinical and supplemental forms) intended to serve as an educational resource when discussing oral health with parents/caregivers of young children. The presenter of the workshop was a faculty member from the Department of Pediatric Dentistry at the University of North Carolina–Chapel Hill who is also the director of bOHP. Topics covered included:
• Background on policies and guidelines of early childhood oral health
• Principles of pediatric preventive care for infants and toddlers including strategies for caregiver interviewing, anticipatory guidance, and clinical examination
• Child development in the delivery of preventive oral health services to infants and toddlers
• The promotion of practice through a family centered approach
Participants were eligible to receive continuing education credits (CE) for attending the workshop. In addition, at the 1 month post-intervention, each participant completed the follow-up survey and then received a booster session which consisted of a visit from a dental program member who reviewed the health information presented at the workshop and discussed any questions or issues that may have arisen in regard to each practice’s progress in implementing the bOHP.
Procedure
After collecting written informed consent, participants in the intervention group completed a pre- and post-survey immediately prior and after the workshop, and follow-up surveys at 1, 3 and 6 months post-intervention. Participants in the control group completed the baseline measures consisting of demographic items and outcome measures upon entry into the study and a follow-up survey at 1 month. The overall design of the study can be seen in Figure 1. Research ethics board approval was obtained prior to commencing the study.
Survey Instrument
The survey instrument was adapted from the authors of the bOHP who previously evaluated the intervention among dental students.12 The baseline and follow-up questionnaires were pilot tested by 6 general dentists prior to dissemination and modifications were made based on their feedback. The survey included demographic items and the following baseline measures to measure change and intervention effectiveness: knowledge, values, confidence, and practice behaviors (Table I). An item to assess participants’ stages of change was used to classify participants as currently caring for infants and toddlers in practice (action) or not currently caring for infants and toddlers in practice (pre-contemplation/contemplation).13 Participants also completed two measures assessing the workshop’s usefulness and the extent to which they expected the workshop to influence their practice behaviors. Two open-ended written questions included an item on barriers to providing dental care for infants and toddlers and an item on soliciting general feedback on this topic (pre- and post-survey) and the workshop (post-survey only).
Analyses
Frequencies, chi-square, and independent-samples t-tests were conducted to examine group differences in sociodemographic and other practice characteristics. For the quantitative data, each construct was represented by a mean score calculated by summing the items and then dividing by the total number of items. Change scores were computed for practice behaviors, knowledge, values, and confidence by subtracting baseline values from post-intervention scores. Independent t-tests were then used to examine whether change scores differed between the intervention and control groups. This paper focuses on findings between the pre- and post-test. Findings for the follow-up assessments (3 and 6 months) are presented for descriptive purposes only. All quantitative analyses were conducted using PASW Statistics 18, Release Version 18.0 (©SPSS, Inc., 2009, Chicago, IL).
Qualitative data from the open-response items were independently analyzed by two researchers. Using an inductive and grounded-theory approach, open, axial, and selective coding was employed to discover themes. Two researchers met to compare codes and any discrepancies were discussed. Only minor differences in the label (name) of the codes were found. Illustrative quotations from the responses were documented to provide examples and further context to the themes that emerged.
RESULTS
Participant Demographics
The final sample consisted of 42 dental professionals. The majority were female (n=40, 95%), worked as dental assistants or dental hygienists (n=33, 78%), and reported working in the dental profession for 11 or more years (n=27, 64%). In addition, 33 participants (79%) reported already caring for infants and toddlers in their practice. In regard to the stages of change construct, 21 (87.5%) and 12 (66.7%) participants in the intervention and control groups, respectively, reported being in the action phase. All demographic characteristics are presented by group in Table II.
Group Equivalency Summary
The intervention and control groups were similar in demographic and practice characteristics (Table II), therefore it was deemed unnecessary to use demographic variables as covariates in the subsequent analyses. Mean scores across time for all variables of interest are presented in Table III. Independent t-tests revealed that the intervention group scored significantly higher with respect to confidence and practice behaviors at baseline compared to the control group (P < .05, Table III).
Pre-Post Group Differences
A significant group interaction effect emerged for value and knowdedge (P < .05), with participants in the intervention group demonstrating significantly higher baseline to post-intervention change scores. No group differences were observed with respect to confidence or practice behaviors (P > .05).
Barriers
Barriers identified from the intervention and control groups at baseline were combined. Four main overarching themes emerged:
1. Child developmental/behavioral barriers (“child is too young,” “behavioral management,” “child cooperation,” and “nervous/fear”)
2. Parent/caregiver barriers (“parent interruption/interference,” “parents are nervous,” “must have parent/caregiver cooperation,” and “lack of knowledge of parents when the first visit should be”)
3. Access to care barriers (“cost,” “transportation,” and “waiting list for pediatric dentists”)
4. Environmental barriers (“open concept office environments,” “gloves/masks/protective eye-wear,” and “sounds and smells”)
Workshop Satisfaction
Items addressing workshop satisfaction were very positive as the mean scores for perceived workshop usefulness (M=9.47; SD=0.90) and perceived influence on practice (M=8.21; SD=1.87) were high. Open responses regarding workshop satisfaction were also positive among intervention participants as indicated in the following examples: “The information provided in this course was very educational and helpful,” “I feel much more comfortable in infant toddler care since this workshop,” and “This was a very good course! It’s great to be able to help small children to care for their teeth.”
Other comments from participants reflected the positive impact of the workshop at the individual level, but highlighted the concern that support and buy-in at the practice level is needed: “I found this very informative; unfortunately the rest of my large office was unable to attend. I will gladly share my information and enthusiasm with them,” “I really enjoyed the seminar, unfortunately I am a single participant from a large practice,” and “Enjoyed the program but don’t think it can influence my doctors.” Interestingly, other additional comments that participants provided conveyed a notion that early preventive care is not the responsibility of the dental practice and placed the responsibility on parents and had a sense of pessimism: “Treating infants could very well lead to a life long fear of dentistry; diagnosing problem areas, then referral to a pediatric specialist with sedation would be best,” and “The only reason this age group would need dental treatment is because of poor caregiver knowledge. Children only eat and drink what they are given. Caregivers need to be responsible for oral care and nutrition. Educate them!”
DISCUSSION
The present findings indicate that the bOHP program had an impact on intervention participants’ knowledge and value of oral healthcare among young children (<3 years), and that the impact appeared to be sustained for at least 6 months. In addition, workshop satisfaction was very positive as reflected in the perceived workshop usefulness and the perceived influence on practice scores.
However, data suggest that the bOHP intervention alone did not impact participants’ confidence or practice behavior in treating young children. This may have been because the recruitment attracted professionals who already had an interest in this topic, or that the items used to measure these constructs were not sufficiently sensitive to detect increases that may have resulted from the intervention. Furthermore, the focus of the workshop was more knowledge-based versus skill building-based. Although the workshop had a hands-on component where participants were able to practice oral healthcare on young children volunteers, many participants were involved in this brief practice as observers only.
Some contradictory results regarding caring for young children emerged. The majority of intervention (87.5%) and control (66.7%) participants reported that they were in the action phase. However, these results were in direct contradiction to participants’ responses to the two items used in the current practice behaviors scale to assess their frequency of caring for 0- to 2-year-olds. Specifically, 100% of control group participants and 76.2% of participants in the intervention group reported that they “rarely” or “never” provided preventive and restorative treatment to 0- to 2-year-olds. This later measure (providing preventive and restorative treatment to 0- to 2-year-olds) was more consistent with what the researchers expected to find, since during formative research within the local health unit prior to planning the bOHP intervention, the following issues were documented:
• Community dentists were uncomfortable in treating children <3 years
• Parents attending well-baby clinics reported that dental offices have told them that their child is “too young” to be seen until the child is at least 3 years old
• A total of 23% of school entrants had experienced dental caries prior to starting school at age 4
The apparent contradiction may be due to several factors, including social desirability or a weakness in questionnaire design. For example, participants may have thought they were practicing the desired behavior and then later realized how infrequently they were doing so, or how their own definition of “caring for toddlers” differed from “best practice.”
The majority of participants were also from mature dental practices (65% of all participants reported working in the dental profession for 10 or more years). Fein et al found that after the bOHP intervention, 89% of student participants reported that they were more likely to provide care to young children in the future.12 Thus, the impact of the program on different dental professional sub-populations warrants further study, particularly among dental students and/or recent graduates who are most likely to be receptive to change. Moreover, interventions such as bOHP may need to be tailored for experienced dental professionals as their confidence and motivation for accepting very young patients may differ from recent dental graduates. Although the dental profession has seen a paradigm shift from a surgical to a preventive focus in some practices, a business case highlighting the economic benefit may motivate mature dental providers to provide preventive oral healthcare to very young patients. For instance, in addition to training programs, economic incentives that allow for increased reimbursement for dental offices that treat infant and young children have shown to be effective.14
The literature suggests that continuing education alone is not sufficient for provider practice changes. Sohn et al’s review of interventions for preventing ECC revealed that continuing education was important but a more systems-based approach was necessary for desired changes.15 In the present study, the majority of participants were either dental assistants or dental hygienists, and may not have the authority to change office policies. This theme of “lack of authority to change office policy” also emerged in the qualitative data. Future research should focus on the entire dental team as both the professional and office levels impact individuals’ practice behaviors. Moreover, some participants perceived that early preventive dental care was not part of their role, but a responsibility of the parent/caregiver, suggesting that research should also explore attitudes and subjective norms among dental professionals.
Although practice guidelines indicate a dental home should be established by age 1, few dental offices in this study’s community routinely following these guidelines. A number of theoretical frameworks suggest that the decision to adopt practice guidelines is complex. As applied to the Information-Motivation-Behavior-Skills Model, information related to practice guidelines and the importance of early preventive care, motivation related to individual attitudes and social norms, and behaviors such as objective skills and perceived self-efficacy could be influencing practice behaviors.16 Barriers as outlined in Cabana’s framework could include: lack of familiarity and awareness of guidelines (knowledge), lack of agreement with specific guidelines, lack of outcome expectancy, lack of self-efficacy, lack of motivation (attitudes), and external barriers, patient factors, guideline factors (eg, presence of contradictory guidelines) and environmental factors (eg, time, resources, organizational constraints, reimbursement concerns).17 Future research on the above constructs could be useful in developing additional interventions that facilitate dental providers’ ability and decrease barriers related to providing preventive care to young children.
In addition, one of the goals of this study was to assess the feasibility of implementing the bOHP among dental professionals in the community. While 61 dental practices employing an unknown number of dental professionals received an invitation to participate, only 24 individuals were recruited into the bOHP evaluation, and only three dentists were in attendance. The inability of the current study to recruit dentists is indicative of the real-world challenges associated with reaching this body of professionals and engaging them into these types of programs. In addition, the thorough approach we took to invite dentists (ie, through personalized invitations sent to every dental clinic along with a reminder letter) represents a strength of the present pilot study. Nonetheless, these numbers indicate the need for exploring novel recruitment and retention strategies and for raising awareness among the dental community about the benefits of professional development. One possible solution would be to promote and get buy-in for interventions with existing professional bodies such as the RCDSO or the College of Dental Hygienists of Ontario to increase future participation and the credibility of future community events. The importance of strategies to increase attendance at trainings has also been highlighted in a recent Cochrane Review that confers the benefits of continuing health education. Specifically, the review, which included 81 trials involving more than 11,000 health professionals, found that attending educational meetings or workshops was associated with improved professional practice as well as improved healthcare outcomes for patients.18
Moreover, although the majority of the participants were dental hygienists/dental assistants, these provider groups are important as they provide critical oral health education and care to patients. From a life course perspective, dental hygienists provide a continuum of care, as they typically see the same patients year after year. Thus, they are witness to major life changes and events, such as the birth of children. As such, they have the potential to play a major role in educating patients about oral health issues, including raising awareness among the general population about the importance of infant oral healthcare. Thus, focusing on educating hygienists and assistants may represent an important starting point for efforts aimed at promoting infant oral healthcare.
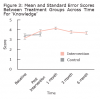
The issue of sustainability is an important consideration for any public health program. Unfortunately, there were a high percentage of participants who were lost to follow-up, thus the long-term impact of the bOHP warrants further study. However, at the 6-month follow-up, the mean scores for value and knowledge did remain higher compared to baseline measures among the intervention group (descriptive data only) (Figure 2 and Figure 3). Moreover, hands-on practical skill training and continuous booster sessions have been found to be critical in sustaining the desired practice behavior among providers and would assist in maintaining the positive impact of the bOHP program.12,15,19
While this is the first study to evaluate the bOHP program among dental professionals in a Canadian community setting, several limitations should be acknowledged. First, the possibility of self-selection bias must be noted given the recruitment methods and the lack of randomization into the intervention and control groups. It is likely that those who chose to attend already had an interest in infant and toddler oral health. Second, more than half of the participants were lost to follow-up. Third, methodological challenges remained, such as a small sample size and the inability to randomly assign participants to the intervention and control groups. However, similar to many other public health community interventions, this quasi-experimental design may be more natural and characteristic of the real-world setting in which interventions are implemented and may possess more external validity, particularly when implementing and evaluating interventions at a local level. Fourth, this study employed a 6-month follow-up to explore whether changes in dental providers’ knowledge, values, confidence, and practice behaviors regarding preventive oral healthcare to young children were sustained. Future research should include longer follow-up periods to provide more meaningful assessments regarding whether these changes have been instituted into practice.
Findings from a national forum on ECC in the United States concluded: “…oral health should be integrated into broader child heath and development systems; dental caries should be addressed through a chronic disease management model; and comprehensive approaches incorporating multiple strategies that involve families, clinicians and child services providers in ECC prevention and reduction efforts should be employed.”20 As professional guidelines and governmental initiatives highlight the importance of early preventive oral healthcare among young children, it is imperative that the local dental workforce is willing and prepared to provide such care. Subsequently, Simpson’s framework for implementing oral health promotion interventions outlines four stages (training, adoption, implementation, and practice) and calls for careful examination of system-level factors (eg, public health, organization) that could be considered when implementing and sustaining such evidence-based interventions.21
CONCLUSION
Notwithstanding the above limitations, results from this community pilot evaluation suggest that the bOHP program may serve as a promising intervention to increase dental professionals’ knowledge and the value of providing oral healthcare to young children and that participants found the workshop useful and applicable. This program may help fill the gap between clinical guidelines and dental practice behaviors; however, evaluating this in the context of varying stages of readiness to change requires further consideration. This may assist in further ensuring a knowledgeable, skilled, and confident dental workforce as a critical component in public health efforts focusing on early detection and decreasing the negative sequelae associated with caries in childhood and across the lifespan.
Summary Points:
• Dental caries is the most common chronic disease in childhood and represents a significant public health concern. In addition, the very early childhood period is a critical time for early identification of risk factors and early intervention to help change the trajectory of a child’s oral health.
• Findings suggest the bOHP is effective in increasing dental professionals’ knowledge and values about the importance of preventive oral health among young children. However, expanding the current program to focus on stages of readiness and including more systems-based approach to enhancing early oral health provider interventions should be considered.
• Ensuring a knowledgeable, skilled, and confident dental workforce is a critical component in public health efforts focusing on early detection and decreasing the negative sequelae associated with caries in childhood and its impact across the lifespan, particularly among the most vulnerable populations.
About the Authors
Cheryl A. Vamos, PhD, MPH, is an assistant professor, associate director, Center for Transdisciplinary Research in Women’s Health (CTR-WH), Department of Community and Family Health, College of Public Health, University of South Florida.
Rocio Quinonez, DMD, MS, MPH, is an associate professor, Department of Pediatric Dentistry, School of Dentistry, University of North Carolina-Chapel Hill.
Anca Gaston, PhD, MS, is a data analyst coordinator, Brant County Health Unit.
Joyce Sinton, BDS, BMSc, DDPH, was previously the Director of Family Health, Brant County Health Unit.
Acknowledgments
The authors would like to acknowledge Tricia Atkinson, dental hygienist, and Jackie Milton, preventative dental assistant, for their assistance with data collection activities.
References
1. A national call to action to promote oral health. US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health, National Institute of Dental and Craniofacial Research. NIH Publication No. 03-5303. 2003.
2. Committee on Clinical and Scientific Affairs. Report on early childhood caries. Canadian Dental Association [Internet]. 2010. [cited 2012 March 14] Available from: http://www.jcda.ca/uploads/pdf/ccsa/ECC-Report-FINAL-April-2010_for-jcda-website.pdf.
3. Atkinson T, McIntosh B, Sinton J, et al. Oral health status of Brant County elementary school children, 2002-2008. Brantford, ON: Brant County Health Unit; 2009.
4. Gunay H, Dmoch-Bockhorn K, Gunay Y, Geurtsen W. Effect on caries experience of a long-term preventive program for mothers and children starting during pregnancy. Clin Oral Investig. 1998;2(3):137-142.
5. Hale KJ, American Academy of Pediatrics Section on Pediatric Dentistry. Oral health risk assessment timing and establishment of the dental home. Pediatrics. 2003;111(5 Pt 1):1113-1116.
6. Dental home by age one - recognition and treatment of ECC. Canadian Academy of Pediatric Dentistry [Internet]. [cited 2012 July 5]. Available from: http://www.capd-acdp.org/index.php?option=com_content&view =article&id=4:dental-home-by-age-one-rec-ognition-and-treatment-of-ecc-&catid=2:hot-topics&Itemid=4.
7. CDA position on first visit to the dentist. Canadian Dental Association [Internet]. 2005 [cited 2012 April 15]. Available from: http://www.cda-adc.ca/_files/position_statements/firstVisit.pdf.
8. Council on Clinical Affairs. Definition of dental home. American Academy of Pediatric Dentistry [Internet]. 2010 [cited 2013 January 15]. Available from: http://www.aapd.org/media/Policies_Guidelines/D_DentalHome.pdf.
9. Kobayashi M, Chi D, Coldwell SE, et al. The effectiveness and estimated costs of the Access to Baby and Child Dentistry Program in Washington State. J Am Dent Assoc. 2005;136(9):1257-1263.
10. Weber-Gasparoni K, Kanellis MJ, Qian F. Iowa’s public health-based infant oral health program: a decade of experience. J Dent Educ. 2010;74(4):363-371.
11. Mission statement. Baby Oral Health Program [Internet]. [cited 2012 September 5]. Available from: http://www.bohp.unc.edu/.
12. Fein JE, Quinonez RB, Phillips C. Introducing infant oral health into dental curricula: A clinical intervention. J Dent Educ. 2009;73(10):1171-1177.
13. Prochaska JO, Redding CA, Evers KE. Transtheoretical model and stages of change. In: Glanz K, Rimer BK, Lewis FM, ed. Health Behavior and Health Education: Theory, Research and Practice. San Francisco, CA. Jossey-Bass. 2002;99-120.
14. Kobayashi M, Chi D, Coldwell SE, et al. The effectiveness and estimated costs of the access to baby and child dentistry program in Washington State. J Am Dent Assoc. 2005;136(9):1257-1263.
15. Sohn W, Ismail AI, Tellez M. Efficacy of educational interventions targeting primary care providers’ practice behaviors: An overview of published systematic reviews. J Public Health Dent. 2004;64(3):164-172.
16. Fisher JD, Fishwer WA. The information-motivation-behavioral skills model. In RJ, Crosby RA, Kegler MC, eds. Emerging Theories in Health Promotion Practice and Research: Strategies for Improving Public Health. San Francisco, CA: Jossey-Bass. 2002;40-70.
17. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guide-lines? A framework for improvement. JAMA. 1999;282(15):1458-1465.
18. Forsetlund L, Bjørndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews. 2009, Issue 2. Art. No.: CD003030.
19. Seale NS, Casamassimo PS. Access to dental care for children in the United States: A survey of general practitioners. J Am Dent Assoc. 2003;134(12):1630-1640.
20. Brown A, Lowe E, Zimmerman B, et al. Preventing early childhood caries: lessons from the field. Pedatr Dent. 2006;28(6):553-560.
21. Simpson DD. A framework for implementing sustainable oral health promotion interventions. J Public Health Dent. 2011;71(s1):S84-S94.