You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Part 1 of this article (Compendium, March 2024) described the history of post and core usage in dentistry, including the various systems and materials utilized for this purpose. It also provided empirical data regarding fiber-reinforced post systems. This second part of the discussion presents a novel concept for developing a precise, predictable post and core complex using the injectable resin method and a newly developed fiber-optic post system.
Developing a Monoblock System Using the Injectable Resin Technique
A system is defined as any set of components working together for the overall objective of the whole.1 The components of a direct fiber-reinforced composite resin post system are the root dentin surface, intraradicular post, core buildup, luting cement, and final restoration. Four interfaces are among these surfaces. A monoblock adhesive system allows for an uninterrupted bonding at all interfaces, resulting in increased resistance to fatigue and fracture, enhanced retention, and reduced microleakage and bacterial infiltration. An adhesive integration of these five components provides structural integrity for intraradicular rehabilitation.1-3 This combined adhesive assembly forms a mechanically homogenous functional unit (monoblock) with improved biomechanical performance that reduces stress at the interface and improves the force distribution while minimizing the potential for fracture.4-9 In vitro studies have demonstrated that the presence of resin-based cement and a fiber post provides a monoblock system that can significantly improve the fracture resistance of structurally weakened roots.10-12
A new concept for developing a monoblock system involves the use of a fiber-reinforced post system and the injection resin technique. A study by Stylianou et al reported that a particular fiber-optic post system had consistent light transmittance throughout the entire length of the post and a significantly greater light-transmitting ability, even with a light-polymerized resin cement. According to their research, the improved polymerization of the resin cement around the fiber-optic posts is related to the posts' different optical properties and composition, as well as the density and orientation of their fibers.13 The clinical case presented in this article provides a clinical illustration of the use of a light-cured flowable resin composite instead of a dual-cured composite resin cement with this fiber-optic post system. This technologically advanced fiber post system reportedly delivers substantial light to the apex, increasing resin flowable polymerization.1 This occurs because of the fiber-optic glass fibers that force all light rays in the acceptance angle to be totally internally reflected and transmitted to the end of the post.
Developing a Ferrule Effect
The concept of "ferrule" or "ferrule effect" is considered the most essential element for the reinforcement of an endodontically treated tooth.14,15 The term originates from the Latin roots "ferrum" meaning iron and "viriola" meaning bracelet. Thus, the ferrule is an encompassing band or ring of cast metal that embraces the coronal surface of the tooth.9,11,12,14-28
A modified interpretation is that parallel walls of dentin extending coronally from the crown margin provide a ferrule preparation design, which after being surrounded by a crown provides a protective mechanism against fracture by reducing stresses within the tooth; this is called the "ferrule effect."20,22 The ferrule design has also been described as incorporating a crown with a 360-degree collar that encompasses the perimeter of the prepared parallel dentin walls and extends cervically to the prepared tooth margin. This design improves the mechanical resistance of the treated tooth by distributing forces on the remaining tooth structure.24,29-31 Preserving tooth structure during preparation is paramount in preventing stress concentrations at the cementoenamel junction of the endodontically restored tooth and providing resistance to tooth fracture. Because maximum preservation of coronal and radicular tooth structure is imperative for optimizing biomechanical behavior of the restored tooth and the long-term survival of endodontically treated crowned teeth,20,32-34 the completed crown preparation should have a ferrule design that encapsulates the endodontically restored tooth complex (Figure 1). The objective of the ferrule is to enhance the structural integrity of the endodontically treated tooth by counteracting stresses such as functional lever forces, the wedging effect of tapered post systems, and lateral forces generated during post placement.9,14,24,35-38 Design parameters to consider for the effectiveness of the ferrule include: number of walls; ferrule width, height, and configuration; design of the cervical collar; type of tooth; the tooth's location in the oral cavity (ie, maxilla/mandible, anterior/posterior); occlusal forces; remaining wall parallelism; post design and material; core material and type; thickness of cement; and type of restoration.9,12,14,19,20,22,24,29-31,39-52
Studies indicate that at least 1 mm to 2 mm of remaining tooth structure coronal to the preparation finish line is required to establish an adequate ferrule.24,48,53 Other studies propose that a ferrule height of 2 mm of vertical sound tooth structure offers the most favorable resistance to tooth fracture and the most optimal stress distributions,54 thus decreasing the weakening effect of a post system.45 Numerous studies have indicated that a uniform ferrule provides a significantly greater resistance to fracture than a non-uniform ferrule.45,46,55 A partial ferrule, however, has been suggested to be a better alternative than no ferrule, although a circumferential coronal structure extending 1.5 mm to 2 mm from the margin of the crown has an improved prognosis.20 One study concluded that the clinical success of endodontically treated premolars was improved when a ferrule of at least 2 mm was present.56 Also, in vitro and clinical studies have demonstrated that allowing 2 mm of coronal tissue to remain around the entire circumference of the endodontically treated tooth will provide resistance such that the design of the post and material are irrelevant.24,57-61
Dislodgment and tooth fracture are causes of post and core restoration failure. A finite element analysis of ferrule design confirmed that a ferrule increases the mechanical resistance of a post/core/crown restorative complex by reducing the potential for displacement.31 A restoration without a ferrule is susceptible to failure from debonding and subsequently by root fracture through the lever action motion of the unstable debonded post.31 Core stability and post retention are important aspects in preventing these failures in the restoration of endodontically treated teeth. The stability of the crown is influenced by the preparation design. This collar effect provides an anti-rotational feature to aid in the stability of the crown. The ideal treatment should replace lost tooth structure while providing adequate retention and support to the core, allowing retention of the restoration while transferring occlusal forces during function and parafunction to prevent root fracture. Root fractures are prevalent in endodontically treated teeth without an adequate ferrule effect.16,62 A direct correlation has been reported between the amount of existing sound coronal tooth structure and the capacity of the tooth to resist occlusal forces.63-66
The authors' general guideline is to have a 1-mm to 2-mm preparation on sound tooth structure. Procedures that provide a shoulder on tooth structure and an axial preparation on the core buildup likely will have an insufficient ferrule design and will compromise the ferrule effect.21 It has been suggested, therefore, that although the ferrule is recommended and desirable, it should not be provided at the detriment of the remaining tooth and/or root structure.16 In cases where there is insufficient sound coronal tooth structure for the ferrule design, this dimension needs to be obtained through periodontal crown lengthening and/or forced tooth eruption procedures to achieve optimal clinical results. If these treatment options are not feasible after informing the patient, alternatives to consider include a post and core with a crown, an extraction with an implant-supported crown, or a fixed (conventional or adhesive bridge) or removable prosthesis.21
Preservation or Replacement of the Natural Tooth?
A frequent dilemma often juxtaposed is the concern over preserving or replacing a compromised natural tooth.67,68 Dental implants provide an appropriate alternative for replacing teeth that cannot be treated with a predictable and favorable prognosis.69 Today, however, many compromised teeth are extracted and replaced with an implant with limited consideration for the vast reconstructive options that are available to restore and maintain them.70 This extraction-oriented reconstructive mentality may be founded on the misconception that endodontically treated teeth are considered inferior to implants with regard to long-term stability and retention.71,72 This misconception is the catalyst for the confusion regarding success or survival outcomes of implants and endodontics.71 Nevertheless, contemporary dentistry should follow an evidence-based approach.71,73
Studies have demonstrated that endodontic and implant therapies have provided similar long-term results.68 One meta-analysis indicated there was no significant difference in success rates between restored single implants (95%) and endodontically treated teeth (94%) over 6 years.74 Another study reported positive outcomes of 74% for implants and 84% for endodontically treated teeth; however, in this study the rate of complications and required interventions was significantly higher in the implant group, and patients required a longer period of time to adjust to the implant restoration.75 Another review evidenced that the failure rate of implants is higher than that of natural teeth in clinically well-maintained patients.73 Furthermore, restorations on implants have shown to have a lower life expectancy over 5 to 10 years than the implants themselves.76 Other long-term studies report high success rates with modern endodontic microsurgery.77-80 Thus, numerous studies and publications have reviewed and debated the question of whether preservation by nonsurgical and surgical endodontic methods or an extraction and replacement with an implant is more beneficial in the long-term.72,81-93
Today, many teeth are replaced with implants because the procedure is considered simpler, requires a shorter treatment time, and is more lucrative than preserving a natural tooth, and the latter may require more knowledge and advanced training to achieve an optimal interdisciplinary treatment strategy.71,94 Also, this self-limiting direction may be responsible for the narrower views, which exclude other disciplines of dentistry.71 The development of modern techniques and materials with advanced technology in all disciplines of dentistry should allow for the preservation and maintenance of natural teeth. The concept of less invasive to more invasive as time requires should be the philosophy of today's dental profession. Thus, each discipline should complement the other and not compete for the long-term health and benefit of the patient.71 Regardless of the selected treatment-whether preserving natural teeth or replacing them with implants-the patient should be part of the restorative solution.95
The following section presents the aforementioned restorative concepts for developing a fiber-reinforced post and core complex using the injectable resin technique to restore an endodontically compromised tooth while providing a precise, repeatable, and predictable result.
Restorative Procedure
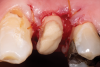
Restorative failure of an existing amalgam restoration on the maxillary left first premolar from recurrent caries is documented here (Figure 2). The periapical radiograph revealed an extensive carious lesion extending into the pulp chamber. After clinical and radiographic evaluation, a treatment plan was discussed with the patient that included endodontic therapy, crown lengthening, and reinforcing the root and supporting the tooth-restorative complex with a fiber-reinforced post and core system.
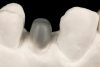
After completion of the endodontic treatment and crown lengthening to develop an ideal ferrule effect (Figure 3 through Figure 5) a diagnostic wax-up was fabricated to an ideal coronal preparation geometric shape, dimension, and height for the anticipated final composite core buildup (Figure 6). A clear polyvinyl siloxane (PVS) impression material was injected into a nonperforated tray, placed over the diagnostic wax-up, and then put into a pressure pot with cold water for 5 minutes. This procedure is aimed at reducing the potential for the formation of voids and bubbles in the impression material (Figure 7 and Figure 8). A small opening was made above the tooth to be restored using a tapered diamond bur (6847) (Figure 9). It is important to clean the internal surfaces with a microbrush to prevent silicone debris from integrating into the flowable material. Prior to the restorative procedure, a diagnostic wax-up was fabricated to the anticipated extracoronal contours for development of the final crown (Figure 10).
After determination of the desired post channel length (one-half to two-thirds the length of the canal), a dental dam was placed using the modified dam technique. The gutta-percha was removed with a series of preshaping instruments (Gates Glidden drills). The channel preparation for a prefabricated fiber-reinforced post (ie, the fiber-optic post system referred to earlier) was performed using a color-coded drill from this post system, establishing the desired intraradicular length and size for the selected post (Figure 11). The prepared channel was rinsed with water and dried with an endodontic paper point.
The preselected fiber-reinforced composite post was placed into the channel space, and the coronal height was measured and marked (Figure 12). The post was cleaned with alcohol, and its surface was silanated with a ceramic primer and air-dried after 60 seconds. The prepared channel was cleaned with a 2% chlorhexidine solution, rinsed, and dried with an endodontic paper point. The prepared endodontic channel was then etched for 15 seconds with 37.5% phosphoric acid semigel. The gel was agitated in the post channel with a paper point (Figure 13), rinsed for 5 seconds, and dried with an endodontic paper point without dehydrating the dentin structure. A universal adhesive was applied with an applicator brush onto the walls and base of the channel and air-dried (Figure 14); any excess adhesive was absorbed with an endodontic paper point using a rapid intermittent movement. The adhesive was lightly air-thinned using a warm air tooth dryer and light-cured for 40 seconds. An injectable flowable universal resin composite was injected into the post channel using an angled tip (Figure 15). It is important to remove the tip slowly while injecting to prevent the incorporation of air bubbles. The aforementioned fiber post was immediately inserted into the post space to the base of the prepared channel, and light-curing was performed from different positions (ie, coronal, facial, and lingual) for 2 minutes (Figure 16).
After polymerization and removal of the stopper, the fiber post was cut with a diamond bur to the predetermined length (Figure 17). It should be noted that the clinician should never use a serrated instrument or shears to cut the post to avoid damaging the integrity of the post. The remaining sound tooth structure (ferrule) was etched for 15 seconds with a 37.5% phosphoric acid semigel, rinsed for 5 seconds, and air-dried (Figure 18). With the use of a sable brush, silane was then applied to the coronal portion of the fiber post and existing composite material and air-dried. A universal adhesive was applied to the tooth structure, existing composite material, and fiber post and allowed to dwell for 10 seconds, then air-dried and light-cured (Figure 19).
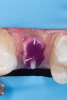
The clear silicone matrix was placed over the posterior segment of the maxillary arch, and an opacious A2-shaded injectable flowable universal resin composite was injected through a small opening above the preparation and fiber post (Figure 20 and Figure 21). The resin composite was cured through the clear resin matrix on the incisal, facial, and lingual aspects for 40 seconds each. Upon removal of the matrix, the excess polymerized composite resin was removed with a #12 scalpel blade, and the incisal sprue was removed using a tapered diamond finishing bur. A round, tapered diamond bur was used to establish the gingival margin (Figure 22) and a needle-shaped finishing bur was used to complete the finishing of the preparation.
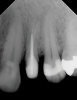
The completed post and core displayed an ideal ferrule dimension (Figure 23 and Figure 24). Radiographic review revealed an optimal integration at the adhesive interfaces (Figure 25). A laboratory-processed composite crown completed the optimal integration between the components of the post-retained system and provided structural integrity for intraradicular rehabilitation (Figure 26).
Conclusion
The dental industry continues to develop improved methods and materials, and clinicians should be encouraged to explore new, innovative products and techniques. This article presented an alternative approach for developing a fiber-reinforced post and core system using the injectable resin technique to restore an endodontically compromised tooth with precision and predictability. As with most procedures, clinical experience and judgment based on scientific evidence must guide final decision-making for application. With the emergence of newer restorative materials that have physical properties and characteristics increasingly similar to natural teeth and the use of adhesive techniques that facilitate the concepts described herein, clinicians can produce tooth-restorative complexes with predictable function and excellent esthetics.
About the Authors
Douglas A. Terry, DDS
Adjunct Professor, Department of Restorative Sciences, University of Alabama at Birmingham, Birmingham, Alabama; Professor Emeritus, Department of Restorative and Esthetic Dentistry, V.S. Dental College and Hospital, Rajiv Gandhi University of Health Sciences, Bengaluru, India; Founder and CEO, Institute of Esthetic and Restorative Dentistry; Private Practice, Houston, Texas
John O. Burgess, DDS, MS
Director of Clinical Research, Clinical Research Professor, School of Dentistry, Louisiana State University, New Orleans, Louisiana; Diplomate, Federal Services Board of General Dentistry
John M. Powers, PhD
Professor Emeritus, UTHealth School of Dentistry, Houston, Texas
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Queries to the author regarding this course may be submitted to mailto:authorqueries@broadcastmed.com.
References
1. Terry DA. Restoring the Intraradicular Space: Esthetic Post Systems. Chicago, IL: Quintessence Publishing; 2021.
2. Sirimai S, Riis DN, Morgano SM. An in vitro study of the fracture resistance and the incidence of vertical root fracture of pulpless teeth restored with six post-and-core systems. J Prosthet Dent. 1999;81(3):262-269.
3. Lui JL. A technique to reinforce weakened roots with post canals. Endod Dent Traumatol. 1987;3(6):310-314.
4. Barjau-Escribano A, Sancho-Bru JL, Forner-Navarro L, et al. Influence of prefabricated post material on restored teeth: fracture strength and stress distribution. Oper Dent. 2006:31(1):47-54.
5. Madfa AA, Abdul Kadir MR, Kashani J, et al. Stress distributions in maxillary central incisors restored with various types of post materials and designs. Med Eng Phys. 2014;36(7):962-967.
6. Basaran ET, Gokce Y. Evaluation of the influence of various restoration techniques on fracture resistance of endodontically treated teeth with different cavity wall thicknesses. Niger J Clin Pract. 2019;22(3):328-334.
7. Pegoretti A, Fambri L, Zappini G, Bianchetti M. Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials. 2002;23(13):2667-2682.
8. Daleprane B, Pereira CNB, Bueno AC, et al. Bond strength of fiber posts to the root canal: effects of anatomic root levels and resin cements. J Prosthet Dent. 2016;116(3):416-424.
9. Maroulakos G, Nagy WM, Kontogiorgos ED. Fracture resistance of compromised endodontically treated teeth restored with bonded post and cores: an in vitro study. J Prosthet Dent. 2015;114(3):390-397.
10. Abduljawad M, Samran A, Kadour J, et al. Effect of fiber posts on the fracture resistance of endodontically treated anterior teeth with cervical cavities: an in vitro study. J Prosthet Dent. 2016;116(1):80-84.
11. Mangold JT, Kern M. Influence of glass-fiber posts on the fracture resistance and failure pattern of endodontically treated premolars with varying substance loss: an in vitro study. J Prosthet Dent. 2011;105(6):387-393.
12. Saupe WA, Gluskin AH, Radke RA Jr. A comparative study of fracture resistance between morphologic dowel and cores and a resin-reinforced dowel system in the intraradicular restoration of structurally compromised roots. Quintessence Int. 1996;27(7):483-491.
13. Stylianou A, Burgess JO, Liu PR, et al. Light-transmitting fiber optic posts: an in vitro evaluation. J Prosthet Dent. 2017;117(1):116-123.
14. Stankiewicz NR, Wilson PR. The ferrule effect: a literature review. Int Endod J. 2002;35(7):575-581.
15. Rosen H. Operative procedures on mutilated endodontically treated teeth. J Prosthet Dent. 1961;11(5):973-986.
16. Kishen A. Mechanisms and risk factors for fracture predilection in endodontically treated teeth. Endod Topics. 2006;13(1):57-83.
17. Baba NZ, Goodacre CJ. Restoration of endodontically treated teeth: contemporary concepts and future perspectives. Endod Topics. 2014;31(1):68-83.
18. Goracci C, Ferrari M. Current perspective on post systems: a literature review. Aust Dent J. 2011;56(suppl 1):77-83.
19. Trushkowsky RD. Restoration of endodontically treated teeth: criteria and technique considerations. Quintessence Int. 2014;45(7):557-567.
20. Juloski J, Radovic I, Goracci C, et al. Ferrule effect: a literature review. J Endod. 2012;38(1):11-19.
21. Ricketts DNJ, Tait CME, Higgins AJ. Tooth preparation for post-retained restorations. Br Dent J. 2005;198(8):463-471.
22. Jotkowitz A, Samet N. Rethinking ferrule-a new approach to an old dilemma. Br Dent J. 2010;209(1):25-33.
23. Rosen H, Partida-Rivera M. Iatrogenic fracture of roots reinforced with a cervical collar. Oper Dent. 1986;11(2):46-50.
24. Sorensen JA, Engelman MJ. Ferrule design and fracture resistance of endodontically treated teeth. J Prosthet Dent. 1990;63(5):529-536.
25. The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10-92.
26. Hsu ML, Chen CS, Chen BJ, et al. Effects of post materials and length on the stress distribution of endodontically treated maxillary central incisors: a 3D finite element analysis. J Oral Rehabil. 2009;36(11):821-830.
27. Stankiewicz N, Wilson P. The ferrule effect. Dent Update. 2008;35(4):222-228.
28. Hempton TJ, Dominici JT. Contemporary crown-lengthening therapy: a review. J Am Dent Assoc. 2010;141(6):647-655.
29. Barkhordar RA, Radke R, Abbasi J. Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent. 1989;61(6):676-678.
30. Tjan AH, Whang SB. Resistance to root fracture of dowel channels with various thickness of buccal dentin walls. J Prosthet Dent. 1985;53(4):496-500.
31. Ichim I, Kuzmanovic DV, Love RM. A finite element analysis of ferrule design on restoration resistance and distribution of stress within a root. Int Endod J. 2006;39(6):443-452.
32. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature - Part 1. Composition and micro- and macrostructure alterations. Quintessence Int. 2007;38(9):733-743.
33. Dietschi D, Duc O, Krejci I, Sadan A. Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int. 2008;39(2):117-129.
34. Fokkinga WA, Kreulen CM, Vallittu PK, Creuger NHJ. A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int J Prosthodont. 2004;17(4):476-482.
35. Standlee JP, Caputo AA, Collard EW, Pollack MH. Analysis of stress distribution by endodontic posts. Oral Surg Oral Med Oral Pathol. 1972;33(6):952-960.
36. Caputo AA, Standlee JP. Biomechanics in Clinical Dentistry. Chicago, IL: Quintessence Publishing; 1987:187-203.
37. Standlee JP, Caputo AA. Interaction of endodontic posts with tooth structure. In: Kurer PF, ed. The Kurer Anchor System. Chicago, IL: Quintessence Publishing; 1984:160-164.
38. Ausiello P, Ciaramella S, Martorelli M, et al. Mechanical behavior of endodontically restored canine teeth: effects of ferrule, post material and shape. Dent Mater. 2017;33(12):1466-1472.
39. Savychuk A, Manda M, Galanis C, et al. Stress generation in mandibular anterior teeth restored with different of post-and-core at various levels of ferrule. J Prosthet Dent. 2018;119(6):965-974.
40. Asmussen E, Peutzfeldt A, Sahafi A. Finite element analysis of stresses in endodontically treated, dowel-restored teeth. J Prosthet Dent. 2005;94(4):321-329.
41. Sterzenbach G, Franke A, Naumann M. Rigid versus flexible dentine-like endodontic posts-clinical testing of a biomechanical concept: seven-year results of a randomized controlled clinical pilot trial on endodontically treated abutment teeth with severe hard tissue loss. J Endod. 2012;38(12):1557-1563.
42. Zicari F, Van Meerbeek B, Scotti R, Naert I. Effect of ferrule and post placement on fracture resistance of endodontically treated teeth after fatigue loading. J Dent. 2013;41(3):207-215.
43. Bitter K, Noetzel J, Stamm O, et al. Randomized clinical trial comparing the effects of post placement on failure rate of post-endodontic restorations: preliminary results of a mean period of 32 month. J Endod. 2009;35(11):1477-1482.
44. Bitter K, Neumann K, Kielbassa AM. Effects of pretreatment and thermocycling on bond strength of resin core materials to various fiber-reinforced composite posts. J Adhes Dent. 2008;10(6):481-489.
45. Tan PL, Aquilino SA, Gratton DG, et al. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent. 2005;93(4):331-336.
46. Ng CC, Dumbrigue HB, Al-Bayat MI, et al. Influence of remaining coronal tooth structure location on the fracture resistance of restored endodontically treated anterior teeth. J Prosthet Dent. 2006;95(4):290-296.
47. Goto Y, Swift EJ Jr. Ferrules for endodontically treated teeth. J Esthet Restor Dent. 2009;21(5):292-293.
48. Libman WJ, Nicholls JI. Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont. 1995;8(2):155-161.
49. Isidor F, Brondum K, Ravnholt G. The influence of post length and crown ferrule length on the resistance to cyclic loading of bovine teeth with prefabricated titanium posts. Int J Prosthodont. 1999;12(1):78-82.
50. Gegauff AG. Effect of crown lengthening and ferrule placement on static load failure of cemented cast post-cores and crowns. J Prosthet Dent. 2000;84(2):169-179.
51. Eraslan O, Aykent F, Yucel MT, Akman S. The finite element analysis of the effect of ferrule height on stress distribution at post-and-core-restored all-ceramic anterior crowns. Clin Oral Investig. 2009;13(2):223-227.
52. Kashani J, Abdul Kadir MR, Arabshahi Z. Finite element analysis of different ferrule heights of endodontically treated tooth. In: Osman NA, Abas WA, Wahab AK, Ting HN, eds. 5th Kuala Lumpur International Conference on Biomedical Engineering. IFMBE Proceedings. 2011;35:432-435.
53. Ng CC, al-Bayat MI, Dumbrigue HB, et al. Effect of no ferrule on failure of teeth restored with bonded posts and cores. Gen Dent. 2004;52(2):143-146.
54. Verissimo C, Simamoto Junior PC, Soares CJ, et al. Effect of the crown, post, and remaining coronal dentin on the biomechanical behavior of endodontically treated maxillary central incisors. J Prosthet Dent. 2014;111(3):234-246.
55. Naumann M, Preuss A, Rosentritt M. Effect of incomplete crown ferrules on load capacity of endodontically treated maxillary incisors restored with fiber posts, composite build-ups, and all-ceramic crowns: an in vitro evaluation after chewing simulation. Acta Odontol Scand. 2006;64(1):31-36.
56. Cagidiaco MC, Garcia-Godoy F, Vich A, et al. Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am J Dent. 2008;21(3):179-184.
57. Trope M, Maltz DO, Tronstad L. Resistance to fracture of restored endodontically treated teeth. Endod Dent Traumatol. 1985;1(3):108-111.
58. Ma PS, Nicholls JI, Junge T, Phillips KM. Load fatigue of teeth with different ferrule lengths, restored with fiber posts, composite resin cores, and all-ceramic crown. J Prosthet Dent. 2009;102(4):229-234.
59. Leary JM, Aquilino SA, Svare CW. An evaluation of post length within the elastic limits of dentin. J Prosthet Dent. 1987;57(3):277-281.
60. Musikant BL, Deutsch AS. Endodontic techniques defined by principles. N Y State Dent J. 2004;70(4):18-21.
61. Milot P, Stein RS. Root fracture in endodontically treated teeth related to post selection and crown design. J Prosthet Dent. 1992;68(3):428-435.
62. Sathorn C, Palamara JE, Palamara D, Messer HH. Effect of root canal size and external root surface morphology on fracture susceptibility and pattern: a finite element analysis. J Endod. 2005;31(4):288-292.
63. Martino N, Truong C, Clark AE, et al. Retrospective analysis of survival rates of post-and-cores in a dental school setting. J Prosthet Dent. 2020;123(3):434-441.
64. Vale WA. Cavity preparation. Irish Dent Rev. 1956;2:33-41.
65. Larson TD, Douglas WH, Geistfeld RE. Effect of prepared cavities on the strength of teeth. Oper Dent. 1981;6(1):2-5.
66. Mondelli J, Steagall L, Ishikiriama A, et al. Fracture strength of human teeth with cavity preparations. J Prosthet Dent. 1980;43(4):419-422.
67. Avila G, Galindo-Moreno P, Soehren S, et al. A novel decision-making process for tooth retention or extraction. J Periodontol. 2009;80(3):476-491.
68. Vozza I, Barone A, Quaranta M, et al. A comparison between endodontics and implantology: an 8-year retrospective study. Clin Implant Dent Relat Res. 2013;15(1):29-36.
69. den Hartog L, Huddleston Slater JJR, Vissink A, et al. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J Clin Periodontol. 2008;35(12):1073-1086.
70. Meyenberg K. The ideal restoration of endodontically treated teeth - structural and esthetic considerations: a review of the literature and clinical guidelines for the restorative clinician. Eur J Esthet Dent. 2013;8(2):238-268.
71. Setzer FC, Kim S. Comparison of long-term survival of implants and endodontically treated teeth. J Dent Res. 2014;93(1):19-26.
72. Ruskin JD, Morton D, Karayazgan B, Amir J. Failed root canals: the case for extraction and immediate implant placement. J Oral Maxillofac Surg. 2005;63(6):829-831.
73. Tomasi C, Wennstrom JL, Berglundh T. Longevity of teeth and implants - a systematic review. J Oral Rehabil. 2008;35(suppl 1):23-32.
74. Iqbal MK, Kim S. For teeth requiring endodontic treatment, what are the differences in outcomes of restored endodontically treated teeth compared to implant-supported restorations? Int J Oral Maxillofac Implants. 2007;22(suppl):96-116.
75. Doyle SL, Hodges JS, Pesun IJ, et al. Retrospective cross sectional comparison of initial nonsurgical endodontic treatment and single-tooth implants. J Endod. 2006;32(9):822-827.
76. Pjetursson BE, Tan K, Lang NP, et al. A systematic review of the survival and complication rates of fixed partial denture (FPDs) after an observation period of at least 5 years. Clin Oral Implants Res. 2004;15(6):625-642.
77. Torabinejad M, White SN. Endodontic treatment options after unsuccessful initial root canal treatment: alternatives to single-tooth implants. J Am Dent Assoc. 2016;147(3):214-220.
78. Bogen G, Kuttler S. Mineral trioxide aggregate obturation: a review and case series. J Endod. 2009;35(6):777-790.
79. Rubinstein RA, Kim S. Long-term follow-up of cases consideration healed one year after apical microsurgery. J Endod. 2002;28(5):378-383.
80. Setzer FC, Kohli MR, Shah SB, et al. Outcome of endodontic surgery: a meta-analysis of the literature-Part 2: comparison of endodontic microsurgical techniques with and without the use of higher magnification. J Endod. 2012;38(1):1-10.
81. Iqbal MK, Kim S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod. 2008;34(5):519-529.
82. Lewis S. Treatment planning: teeth versus implants. Int J Periodontics Restorative Dent. 1996;16(4):366-377.
83. Bader HI. Treatment planning for implants versus root canal therapy: a contemporary dilemma. Implant Dent. 2002;11(3):217-223.
84. Cohn SA. Treatment choices for negative outcomes with non-surgical root canal treatment: non-surgical retreatment vs surgical retreatment vs implants. Endod Topics. 2005;11(1):4-24.
85. Felton DA. Implant or root canal therapy: a prosthodontist's view. J Esthet Restor Dent. 2005;17(4):197-199.
86. Trope M. Implant or root canal therapy: an endodontist's view. J Esthet Restor Dent. 2005;17(3):139-140.
87. Dawson AS, Cardaci SC. Endodontics versus implantology: to extirpate or integrate? Aust Endod J. 2006;32(2):57-63.
88. Spangberg LS. To implant, or not to implant: that is the question. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101(6):695-696.
89. Thomas MV, Beagle JR. Evidence-based decision-making: implants versus natural teeth. Dent Clin North Am. 2006;50(3):451-461.
90. Torabinejad M, Goodacre CJ. Endodontic or dental implant therapy: the factors affecting treatment planning. J Am Dent Assoc. 2006;137(7):973-977.
91. White SN, Miklus VG, Potter KS, et al. Endodontics and implants, a catalog of therapeutic contrasts. J Evid Based Dent Pract. 2006;6(1):101-109.
92. Mordohai N, Reshad M, Jivraj S, Chee W. Factors that affect individual tooth prognosis and choices in contemporary treatment planning. Br Dent J. 2007;202(2):63-72.
93. Kao RT. Strategic extraction: a paradigm, shift that is changing our profession. J Periodontol. 2008;79(6):971-977.
94. Ricci G, Ricci A, Ricci C. Save the natural tooth or place an implant? Three periodontal decisional criteria to perform a correct therapy. Int J Periodontics Restorative Dent. 2011;31(1):29-37.
95. Terry DA, Geller W. Esthetic post systems. In: Esthetic and Restorative Dentistry: Material Selection and Technique. 3rd ed. Chicago, IL: Quintessence Publishing; 2018:458-493.