You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
With appropriate therapy and patient compliance with plaque control, periodontal tissues have the ability to recover from disease and even regenerate.1-3 Because periodontal ligament cells act like stem cells, they can form cementum and bone to replace lost tissues of the periodontium.4 Teeth with severe alveolar bone loss are often assigned a hopeless prognosis and recommended for extraction.5 They are rarely given the opportunity to survive. Periodontal disease is diagnosed by clinical attachment loss.6 The patient's history of disease and behavioral, social, and environmental risk factors are often considered during diagnosis and treatment of this condition. Further, control of periodontal disease does not occur until etiologic and risk factors are controlled.7,8 Therefore, patient compliance, appropriate care, and adequate healing time are essential for desired outcomes.8-11
Patients with advanced periodontal disease benefit from a comprehensive periodontal assessment and a rigorous nonsurgical periodontal therapy program.12 As seasoned professionals and specialists are aware, furcation involvements may manifest due to loss of interradicular bone and of the periodontal ligament between the roots of molars. In general, maxillary molars are trifurcated, while the mandibular molars and, at times, the maxillary first premolar are bifurcated. A specialized instrument, the Nabers probe, is used to measure the amount of interradicular bone loss in multi-rooted teeth.13 Typically, the Nabers probe has markings in increments of 3 mm-at 3 mm, 6 mm, 9 mm, and 12 mm (Figure 1).
The technique for furcation probing is site-specific. The buccal furcations of mandibular and maxillary molars may be probed from the buccal aspect, while the lingual furcations of mandibular molars are approached from the lingual. The mesial-lingual furcations of maxillary molars and of the first maxillary premolars are accessed from the mesial-lingual aspect, while the distal-lingual furcations of maxillary molars are accessible from the distal-lingual.13
One of the most common systems used for classification of furcation involvements is Glickman's Furcation Classification system, where Grade I furcation has slight loss of interradicular bone that is undetectable by radiographs but detectable by the Nabers probe. Grade II furcation involvement has loss of bone from one aspect or both aspects of the furcation, with a portion of alveolar bone intact. In this case, the furcation probe can partially enter the furcation area. In Grade III furcation, the interradicular bone is completely absent, but the lingual and/or buccal aspect of the furcation is occluded by the gingiva. In Grade IV furcation, the interradicular bone is completely destroyed and the entire furcation can be seen clinically. In Grade III and IV furcation involvement, the furcation probe can pass through the furcation, and radiolucency between roots can be seen radiographically.14
Appropriate instrument selection for the debridement of deep periodontal pockets is critical for the removal of calculus that is difficult to reach. Ultrasonic instrumentation in pockets greater than 5 mm is best achieved by the left and right curved ultrasonic inserts (Figure 2) due to their adaptability to root anatomy.15
These modified ultrasonic inserts are used together as a pair and are area-specific. The right insert is used on buccal surfaces of the maxillary right or mandibular left and on lingual surfaces of the maxillary left or mandibular right (Figure 3). The left insert is used on the lingual surfaces of the maxillary right or mandibular left and on buccal surfaces of the maxillary left or mandibular right (Figure 4).
For hand instrumentation of deep pockets, curettes with extended shanks are preferable to traditional-length curettes13 due to the 3-mm extension of the terminal shank when compared with traditional curettes, which allows for access to calculus located in periodontal pockets greater than 5 mm (Figure 5).
Case Report
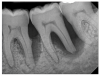
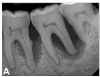
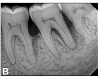
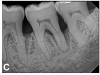
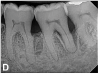
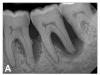
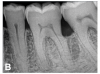
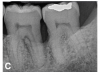
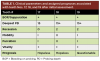
A 63-year-old male patient with a medical history of asthma, hay fever, sinusitis, and arthritis was referred for periodontal therapy in November 2015. He reported taking multivitamins, fish oil, and naproxen sodium occasionally for pain. The patient did not report experiencing any dental discomfort. The clinical findings, radiographic interpretations, diagnosis, and preoperative prognosis for teeth Nos. 17 through 19 are summarized in Figure 6 and Table 1. The patient was informed that teeth Nos. 17 and 18 should be extracted and that tooth No. 19 would need regenerative therapy. A treatment plan was devised for phase I and phase III periodontal therapy, and the patient consented to the proposed treatment verbally and in writing.
Case Management
For initial treatment, the patient was educated about the causes and risk factors of periodontal disease, and oral hygiene instructions were provided. Phase I periodontal therapy was completed for teeth Nos. 17 through 19 using local anesthesia, the lower arch was deplaqued, and personal oral hygiene was assessed. Oral hygiene instructions were given. The patient returned 8 weeks later for periodontal re-evaluation. At that time, supportive periodontal therapy (SPT) was initiated, and teeth with residual subgingival calculus were retreated. For almost 5 years, the patient's periodontal disease was managed using only SPT every 3 months.
Clinical Outcomes
The patient's periodontal disease improved with initial nonsurgical periodontal therapy that involved scaling and root planing. This initial treatment was followed by only SPT every 3 months. Despite treatment, residual deep periodontal probing depths remained, so a decision was made to maximize improvements with nonsurgical therapy and to reassess as needed to determine whether surgical intervention was appropriate. After almost 5 years of SPT and good patient compliance with plaque control and supportive care, the periodontium was stable. Because of the resulting bone formation and improvements in clinical attachment levels (Figure 7 through Figure 13), it was determined that periodontal surgical intervention was not necessary.
Conclusion
In the case report presented, treatment with nonsurgical therapy for 5 years effectively halted destruction and led to bone regeneration and improved clinical attachment levels. Although the primary etiology of periodontal disease is well documented, secondary etiologic and contributing factors are numerous.16 After initial therapy in the current case, there was radiographic evidence of a hypercementosis-like lesion on the distal root of tooth No. 19 (Figure 7 through Figure 10). Hypercementosis is a nidus for plaque accumulation leading to disease progression; however, the presence of this lesion did not explain the disease severity observed for tooth No. 18. Chronic periodontitis is the most widespread form of periodontal disease, and nonsurgical periodontal therapy is the most common type of therapy.17 Scaling and root planning is the gold standard for periodontal treatment. When performed meticulously, they result in improvement of clinical parameters through changes related to tissue shrinkage, long junctional epithelium, new attachment, and in rare circumstances, regeneration.18 The use of nonsurgical periodontal therapy for treatment of periodontal disease requires that the timing for re-evaluation is customized for each patient. Because individuals heal at different rates, the overall medical condition, nutritional intake, environmental and social risks factors, local factors, and colonization of pathogenic bacteria of patients should be considered.7,8 Some patients cannot afford, or choose not to pursue, surgical periodontal therapy. For these patients, clinicians should delay surgical decisions until periodontal risk factors are addressed and nonsurgical efforts are exhausted.
Although rare, the radiographic evidence in the current case indicated that nonsurgical therapy effectively halted the destructive effects of severe chronic periodontitis and led to bone regeneration, thereby eliminating the need for surgery. The current case also showed that nonsurgical periodontal therapy may lead to desirable outcomes for patients with severe chronic periodontal disease if the patient is compliant with plaque control, supportive periodontal therapy is provided, etiological and risk factors are eliminated, and the body is given adequate time to heal.11 An additional factor that may have influenced the positive outcome of the current case was the patient's favorable health status.
The outcomes of the current case report illustrated the periodontium's ability to regenerate under favorable physiologic oral environment conditions. Specifically, treatment of the patient using nonsurgical periodontal therapy showed that teeth initially assigned with a hopeless prognosis can be saved. Further, the patient's positive treatment outcome highlights the inability of clinicians to predictably prognosticate for this condition. Because the current knowledge and understanding of periodontal healing in the profession seems to be lacking, clinicians should carefully consider planned extractions of teeth with similar severe periodontal destruction. Results of this case report should be considered as a guide for development of treatment plans that attempt to preserve the natural dentition of patients with severe periodontal disease. Perhaps if more time is allotted for treatment and healing of periodontally involved teeth, more teeth could be saved.
References
1. Lindhe J, Westfelt E, Nyman S, et al. Healing following surgical/non-surgical treatment of periodontal disease: a clinical study. J Clin Periodontol. 1982;9(2):115-128.
2. Lindhe J, Westfelt E, Nyman S, et al. Long-term effect of surgical/non-surgical treatment of periodontal disease. J Clin Periodontol. 1984;11(7):448-458.
3. Greenstein G. Periodontal response to mechanical non-surgical therapy: a review. J Periodontol.1992;63(2):118-130.
4. Maeda H, Tomokiyo A, Fujii S, et al. Promise of periodontal ligament stem cells in regeneration of periodontium. Stem Cell Res Ther. 2011;2(4):33.
5. Al-Shammari KF, Al-Khabbaz AK, Al-Ansari JM, et al. Risk indicators for tooth loss due to periodontal disease. J Periodontol. 2005;76(11):1910-1918.
6. American Academy of Periodontology. Parameter on chronic periodontitis with advanced loss of periodontal support. J Periodontol. 2000;71(5S):856-858.
7. Kinane DF, Radvar M. The effect of smoking on mechanical and antimicrobial periodontal therapy. J Periodontol. 1997;68(5):467-472.
8. Shiloah J, Patters MR. Repopulation of periodontal pockets by microbial pathogens in the absence of supportive therapy. J Periodontol. 1996;67(2):130-139.
9. Rosling B, Nyman S, Lindhe J. The effect of systematic plaque control on bone regeneration in infrabony pockets. J Clin Periodontol. 1976;3(1):38-53.
10. Hwang YJ, Fien MJ, Lee SS, et al. Effect of scaling and root planing on alveolar bone as measured by subtraction radiography. J Periodontol. 2008;79(9):1663-1669.
11. Mousquès T, Listgarten MA, Phillips RW. Effect of scaling and root planing on the composition of the human subgingival microbial flora. J Periodontal Res. 1980;15(2):144-151.
12. Plessas A. Nonsurgical periodontal treatment: review of the evidence. Oral Health Dent Manag. 2014;13(1):71-80.
13. Gehrig JS, Sroda R, Saccuzzo D. Fundamentals of Periodontal Instrumentation and Advanced Root Instrumentation. 8th ed. Jones & Bartlett Learning; 2018.
14. Pilloni A, Rojas MA. Furcation involvement classification: a comprehensive review and a new system proposal. Dent J (Basel).2018;6(3):34.
15. Dragoo, M. R. A clinical evaluation of hand and ultrasonic instruments on subgingival debridement. 1. With unmodified and modified ultrasonic inserts. Int J Periodontics Restorative Dent. 1992;12(4):310-323.
16. Eke PI, Wei L, Thornton‐Evans GO, et al. Risk indicators for periodontitis in US adults: NHANES 2009 to 2012. J Periodontol. 2016;87(10):1174-1185.
17. Greenstein G. Nonsurgical periodontal therapy in 2000: a literature review. J Am Dent Assoc. 2000;131(11):1580-1592.
18. Cobb CM. Non-surgical pocket therapy: mechanical. Ann Periodontol. 1996;1:443-490.