You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Clinicians have tried for years to define teeth with unseparated fractures that experience symptoms such as biting discomfort, thermal sensitivity, and vague pain.1 The diagnostic terminology to define fractured teeth has undergone several revisions over the past 60 years, from "cusp fracture odontalgia" to "cracked tooth syndrome."1,2 More recently, in 2020, the American Association of Endodontists' (AAE) Glossary of Endodontic Termsupdated the definition of fracture in an attempt to bring uniformity to the diagnostic lexicon. It defines a fracture as "a disruption of the enamel and/or dentin and/or cementum that is assumed to be of greater depth than a crack, of unknown depth or extension, visible or not visible clinically or radiographically, and with separated or unseparated segments."3 The Glossary also categorizes fractures as traumatic fractures and root fractures, with each of these types broken down into even more specific subcategories based on location (Table 1).3 The categorical AAE terminology assumes the clinician's ability to accurately visualize the extent of the fracture either by clinical or radiographic means.
Unseparated fractures-ie, those with no visible separation between segments-generally do not fit the Glossary's criteria. The typical mesial to distal fracture line seen on a posterior tooth may be directly visualized on the surface of the tooth, or it may be located beneath restorative material. Generally speaking, because narrow fracture lines cannot be visualized radiographically, the full extent of a fracture cannot be determined unless invasive and potentially destructive exploratory procedures are undertaken, including drilling, exploratory surgery, or extraction.4 As a result, diagnostic accuracy may be diminished, and discussion of management options with patients may be confusing, with resultant negative effects on treatment outcomes. The lack of clarity in accurately determining the extent of fractures may also explain the great variability in how clinicians approach unseparated fractures.5
The purpose of this article is to review and provide an update on unseparated fractures of indeterminate extension in non-endodontically treated teeth. Following a summary of the literature to date on this topic, an evidence-grounded treatment algorithm will be presented.
Epidemiology
The endodontic literature is replete with studies describing fracture epidemiology. The prevalence of fractures is reported to be from 8% to 10% in private endodontic practice and university settings.6,7 Most studies report no significant gender differences in fracture prevalence.8,9 Fractured teeth most commonly occur in individuals aged between 40 and 60 years.7,9,10 There is no consensus on whether restoration types impact susceptibility to tooth fracture, as unseparated fractures can be found in unrestored teeth as well as those treated with both small and large restorations.6-11 Fractures were most frequently found on mandibular molars followed by maxillary molars, with the mandibular second molar being the most commonly fractured tooth.6-8,10,11
Etiology
A variety of forces act on teeth, especially during mastication. Masticatory forces increase occlusal load stress, resulting in cusp flexure and susceptibility to microfractures.8 Beyond function, excessive forces caused by parafunction and trauma contribute to fracture development.10 These forces likely play a role in the development of fractures in unrestored teeth.
Restorative factors also impact fracture development. Thermal expansion of restorative materials may play a role in fracture development and propagation, as the coefficients of thermal expansion of gold and amalgam are greater than that of natural teeth.8 An association was found between these non-bonded restorations and fracture development.1 Fracture risk is also related to the depth of the cavity preparation. Compared to teeth with narrow and shallow cavity preparations, teeth with wide and deep preparations have increased fracture potential.12
Diagnosis
The diagnosis of fracture pathology does not differ from the diagnosis of endodontic pathology in that the examination must replicate a patient's chief complaint. A comprehensive endodontic examination is necessary in the workup of fractures, and must include a dental examination, localized periodontal examination, as well as pulp sensitivity and periapical testing. Clinicians should be suspicious of a fracture when patients report thermal sensitivity or chewing discomfort, particularly in teeth without another clear etiology for pulpal pathology such as caries or historically deep restorations.1
Bite sensitivity in the fractured dentition may be difficult to localize, and, historically, these signs have been elucidated with tools such as wooden toothpicks or cotton rolls.1 Plastic bite testers that are now commercially available are commonly used to identify the problem tooth. Although various diagnostic tools are available for bite testing, one study found that while 73% of patients reported experiencing pain from biting, only 56% of the patients gave a positive response to the test.7
Dyes also are used to assist clinicians in identifying fractures and visualizing their complete depth either before or during preparation, usually with the aid of magnification. Methylene blue is one such dye that may be applied to suspected areas for better visualization.13 Transillumination methods, wherein a fiberoptic light in a darkened environment shined on the fracture will not transmit beyond a fracture line, are also used to determine the presence of fractures.13
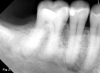
Radiographs are also necessary for fracture diagnosis. While 2-dimensional radiography is the standard of care in endodontics, cone-beam computed tomography (CBCT) represents an effective diagnostic tool. Although CBCT can detect only fractures of relatively large diameter, often 50 µm fracture width, its utility is apparent in the improved detection of periradicular bony changes caused by fractures extending onto root structure as compared to periapical imaging.4,14 Limitations exist beyond inadequate resolution to detect fractures, however, as radiodense restorative materials in teeth can create significant artifacts.4
Prognosis
When considering treatment protocols and recommendations, it is imperative that an analysis of prognosis and the factors that affect outcomes is performed. A body of literature has emerged correlating fracture depth and, thus, treatment prognosis to a variety of factors, including the presence or absence of symptoms, the presence of periodontal or radiographic findings consistent with root involvement, as well as the pulpal or periapical diagnosis of a fractured tooth at the time of treatment.6,7,9,14,15
The prognosis of a fractured tooth depends on the size and location of the fracture. Although multiple fractures may not impact prognosis, the presence of a fracture on a distal marginal ridge might.6,16 Fracture lines can propagate and communicate, resulting in a complete fracture or splitting of the tooth, which can act as a pathway(s) for infection.17 It is mostly assumed that root involvement carries with it a poor prognosis given adjacent periodontal involvement, bone loss, and risk of infection.18,19 Fractures found intraoperatively to extend to and involve the pulpal floor are shown to have a 5-year survival of only 88%, compared to 99% survival found in teeth with shallower fractures.20 Radicular fractures harbor bacteria and debris with associated bony dehiscences, resulting in narrow and deep periodontal pockets or even periradicular bone resorption.21,22 Isolated periodontal pockets greater than 4 mm to 6 mm found adjacent to fracture lines are associated with a poorer prognosis.6,7,9
Signs and symptoms of pulpal involvement are correlated with fracture depth and, therefore, prognosis. Fractured teeth associated with reversible pulpitis show good success following full-coverage restorative care. In one study, 89% of symptomatic fractured teeth had symptoms resolve with crown placement.23 In another, only 21% of fractured teeth that were crowned developed progression to irreversible pulpitis or pulpal necrosis in the 6 months following full-coverage restorative care.24
The effect of preoperative pulpal and periapical diagnoses on outcomes following treatment of fractured teeth has been discussed extensively in the literature. Although a small study of 27 extracted teeth with "fracture necrosis," that is, pulpal necrosis secondary to fractures, had evidence of root fracture involvement, other reports found no significant effects of pulpal status on treatment outcomes.6,16,19 Similarly, periapical status may impact outcomes, as a significantly negative effect was reported in teeth with preoperative asymptomatic apical periodontitis and chronic or acute apical abscess.6
That said, certain treatment protocols have been shown to improve outcomes for fractured teeth. Even in teeth with radicular extensions, one study reported 90.6% success at 2 to 4 years post-root canal treatment, with improvements noted when microscope-assisted intraorifice barriers were placed apical to the fracture, occlusal reduction was performed postoperatively, and full-coverage restorations were placed expeditiously.25 In summary, pretreatment prognostic factors for fractured teeth include the size, extent, and location of fractures, periodontal involvement, and periapical diagnosis, while intratreatment prognostic factors for fractured teeth include microscope-aided intraorifice barriers, occlusal reduction, and expedient crown placement.
Treatment Algorithm
The evidence presented above can be used to develop a treatment algorithm for teeth with unseparated fractures. This systematic approach allows for a practical progression of both diagnosis and management (Figure 1). The first consideration to be made is whether the tooth is symptomatic or asymptomatic. In the absence of symptoms, a full-coverage restoration may be considered in addition to monitoring for fracture progression or symptom development. Bonded restorations should only be considered as a stopgap means to slow progression of newly developing fractures, and patients should be informed of the risks of failure and fracture progression.26-28
Symptomatic teeth must undergo careful assessment. Beyond pulp sensitivity testing to measure for cold and periapical tests to measure for percussion, palpation, or bite sensitivity, both a limited periodontal examination to detect periodontal pocketing and a detailed radiographic assessment should be performed on any tooth with suspected fracture. CBCT imaging allows for early detection of crestal bone loss adjacent to unseparated fractures. Narrow crestal bone defects suggest root fracture involvement, whereas wider defects may indicate generalized periodontal bone loss of inflammatory origin.
Shallow symptomatic fractures typically present with symptoms consistent with reversible pulpitis, namely non-lingering cold sensitivity, as well as biting sensitivity. Periodontal involvement and radiographic abnormalities, including crestal bone loss or apical pathology, should be absent. Full-coverage restorative care is indicated for these teeth as a reliable means to not only resolve the symptoms associated with these fractures, but also prevent fracture progression to pulpal involvement and eventual necrosis.29-31 Still, certain teeth will remain symptomatic following full-coverage restorative care, suggestive of deeper infractions involving the pulp; therefore, placement of a temporary crown is advisable prior to placement of the definitive crown. A minimum of 2 weeks duration before definitive crown placement will allow for assessment of postoperative symptoms.32 If symptoms fail to resolve with temporary crown placement, the preoperative diagnosis may be changed to symptomatic irreversible pulpitis, warranting endodontic intervention (as described in the next paragraph) prior to crown cementation.
Unseparated fractures may also be identified concurrently with symptoms consistent with symptomatic irreversible pulpitis, which is characterized by heightened and lingering sensations to cold along with biting sensitivity and sometimes spontaneous pain. As long as no defects consistent with root fracture involvement are present, root canal therapy is indicated.33 Fractures can be further assessed using a surgical operating microscope during delivery of endodontic care. Direct visualization of fractures extending to the pulpal floor have a reduced prognosis compared to shallower fractures, and patients should be forewarned of this possibility and informed of actual visualized fracture extension during delivery of care. In some cases, patients may decide to consider endodontic intervention as an "exploratory" procedure in that the determination of fracture depth can dictate the ultimate choice of whether to save a tooth or elect extraction.
If, during root canal therapy, fractures are noted that extend into the canal orifice, intraoperative and microscope-assisted placement of a bonded intraorifice barrier is advised. Numerous materials composed of resin-modified glass-ionomers or composite materials are available for this purpose in dedicated or adapted forms. Additionally, occlusal surfaces should be reduced, taking teeth clear from occlusal interferences following treatment, and full-coverage restorative care should be completed expediently for fracture stabilization.25
When unseparated fractures are accompanied by radiographic crestal bone defects suggestive of root fracture involvement, a thoughtful discussion with the patient should occur regarding the potentially reduced prognosis for long-term maintenance of these teeth. Patients should be counseled that a deep infraction is at risk of enlargement by the same factors that led to initial fracture development, including traumatic biting incidents or parafunction. Risk mitigation involves efforts to minimize these factors, such as the use of occlusal guards when indicated and incorporation of expedient post-endodontic fracture stabilization protocols previously described. If patients do elect to retain the tooth with apparent root fracture involvement, close postoperative monitoring is indicated to prevent progressive bone loss that can accompany failing treatments and limit future implant replacement. Informed consent always requires presentation of treatment alternatives, and cases of unseparated fractures with suspected root involvement warrant thoughtful consideration of the alternative of extraction with or without replacement.
Teeth presenting with signs and symptoms consistent with pulp necrosis or periapical infection should be managed similarly to cases without infection. That said, because the literature suggests a connection between pulpal and periapical infection to root fracture involvement and a reduced prognosis much more directly, the conversation about potential reductions in prognosis should occur even if crestal bone defects are not present preoperatively.6,19 Patients should be informed of the risks of pursuing root canal therapy and full-coverage restorative care, including recurrent symptoms or infection and eventual tooth loss, as well as the benefits of maintaining a tooth and postponing extraction for as long as possible. Conversations must incorporate the patient's individual risk profile, including possible effects their health history might have (eg, bisphosphonate use, medical complexity) and their ability to have an extracted tooth replaced.
The extent of any crestal bone defects can impact recommendations. Teeth with extensive crestal bone defects whose further enlargement would complicate future implant replacement, for example, might be better suited to extraction. When discussing such issues with patients, the conversation should be detailed and accompanied by visual aids such as radiographs and/or illustrations, and include a thorough review of risks and benefits in both the short and long term. A case of fracture necrosis and periapical infection is presented in Figure 2 and Figure 3. Figure 1, to reiterate, summarizes the proposed treatment algorithm for unseparated fractures.
Conclusion
Unseparated fractures represent one of the most complex areas of dental diagnostics, and diagnosis is currently limited to indirect visualization of these fractures. Evidence-based conduits must be incorporated to best determine the extension of such fractures in order to provide patients with the best care possible. Ultimately, management of a patient with unseparated fractures should be approached in a systematic manner. Symptoms, preoperative diagnostics, and CBCT imaging are all elements that can aid in the clinician's understanding of fracture depth and should be precursors to appropriate management.
About the Authors
Jacquelyn Chou, DMD, Certificate in Endodontics
Private Practice limited to Endodontics, Boston, Massachusetts
Brooke Blicher, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Clinical Instructor, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston, Massachusetts; Instructor in Surgery, Dartmouth Medical School, Hanover, New Hampshire; Co-founder, Pulp Nonfiction Endodontics; Private Practice limited to Endodontics, White River Junction, Vermont
Rebekah Lucier Pryles, DMD, Certificate in Endodontics
Assistant Clinical Professor, Department of Endodontics, Tufts University School of Dental Medicine, Boston, Massachusetts; Clinical Instructor, Department of Restorative Dentistry and Biomaterials Science, Harvard School of Dental Medicine, Boston, Massachusetts; Co-founder, Pulp Nonfiction Endodontics; Private Practice limited to Endodontics, White River Junction, Vermont
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Cameron CE. Cracked-tooth syndrome. J Am Dent Assoc. 1964;68
(97):405-411.
2. Gibbs JW. Cuspal fracture odontalgia. Dent Digest. 1954;60:158-160.
3. American Association of Endodontists. Glossary of Endodontic Terms. 10th ed. Chicago, IL: American Association of Endodontists; 2020. https://www.aae.org/specialty/clinical-resources/glossary-endodontic-terms/. Accessed July 26, 2022.
4. Patel S, Brady E, Wilson R, et al. The detection of vertical root fractures in root filled teeth with periapical radiographs and CBCT scans. Int Endod J. 2013;46(12):1140-1152.
5. Alkhalifah S, Alkandari H, Sharma PN, Moule AJ. Treatment of cracked teeth. J Endod. 2017;43(9):1579-1586.
6. Krell KV, Caplan DJ. 12-month success of cracked teeth treated with orthograde root canal treatment. J Endod. 2018;44(4):543-548.
7. Kang SH, Kim BS, Kim Y. Cracked teeth: distribution, characteristics, and survival after root canal treatment. J Endod. 2016;42(4):557-562.
8. Seo DG, Yi YA, Shin SJ, Park JW. Analysis of factors associated with cracked teeth. J Endod. 2012;38(3):288-292.
9. Kim SY, Kim SH, Cho SB, et al. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod. 2013;39(4):449-452.
10. Hilton TJ, Funkhouser E, Ferracane JL, et al. Correlation between symptoms and external characteristics of cracked teeth: findings from the National Dental Practice-Based Research Network. J Am Dent Assoc. 2017;148(4):246-256.e1.
11. Cameron CE. The cracked tooth syndrome: additional findings. J Am Dent Assoc. 1976;93(5):971-975.
12. Goel VK, Khera SC, Gurusami S, Chen RC. Effect of cavity depth on stresses in a restored tooth. J Prosthet Dent. 1992;67(2):174-183.
13. Wright HM Jr, Loushine RJ, Weller RN, et al. Identification of resected root-end dentinal cracks: a comparative study of transillumination and dyes. J Endod. 2004;30(10):712-715.
14. Wang P, Yan XB, Lui DG, et al. Detection of dental root fractures by using cone-beam computed tomography. Dentomaxillofac Radiol. 2011;40(5):290-298.
15. Berman LH, Hargreaves KM. Cohen's Pathways of the Pulp. 12th ed. St. Louis, MO: Mosby Elsevier; 2020.
16. Olivieri JG, Elmsmari F, Miró Q, et al. Outcome and survival of endodontically treated cracked posterior permanent teeth: a systematic review and meta-analysis. J Endod. 2020;46(4):455-463.
17. Gutmann JL, Rakusin H. Endodontic and restorative management of incompletely fractured molar teeth. Int Endod J. 1994;27(6):343-348.
18. Hayashi M, Kinomoto Y, Takeshige F, Ebisu S. Prognosis of intentional replantation of vertically fractured roots reconstructed with dentin-bonded resin. J Endod. 2004;30(3):145-148.
19. Berman LH, Kuttler S. Fracture necrosis: diagnosis, prognosis assessment, and treatment recommendations. J Endod. 2010;36(3):442-446.
20. Sim IG, Lim TS, Krishnaswamy G, Chen NN. Decision making for retention of endodontically treated posterior cracked teeth: a 5-year follow-up study. J Endod. 2016;42(2):225-229.
21. Lustig JP, Tamse A, Fuss Z. Pattern of bone resorption in vertically fractured, endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90(2):224-227.
22. Walton RE. Vertical root fracture: factors related to identification. J Am Dent Assoc. 2017;148(2):100-105.
23. Guthrie RC, DiFiore PM. Treating the cracked tooth with a full crown. J Am Dent Assoc. 1991;122(9):71-73.
24. Krell KV, Rivera EM. A six year evaluation of cracked teeth diagnosed with reversible pulpitis: treatment and prognosis. J Endod. 2007;33(12):1405-1407.
25. Davis MC, Shariff SS. Success and survival of endodontically treated cracked teeth with radicular extensions: a 2- to 4-year prospective cohort. J Endod. 2019;45(7):848-855.
26. Opdam NJ, Roeters JJ, Loomans BA, Bronkhorst EM. Seven-year clinical evaluation of painful cracked teeth restored with a direct composite restoration. J Endod. 2008;34(7):808-811.
27. Fissore B, Nicholls JI, Yuodelis RA. Load fatigue of teeth restored by a dentin bonding agent and a posterior composite resin. J Prosthet Dent. 1991;65(1):80-85.
28. Kakka A, Gavriil D, Whitworth J. Treatment of cracked teeth: a comprehensive narrative review. Clin Exp Dent Res. 2022. doi: 10.1002/cre2.617.
29. Snyder DE. The cracked-tooth syndrome and fractured posterior cusp. Oral Surg Oral Med Oral Pathol. 1976;41(6):698-704.
30. Silvestri AR Jr, Singh I. Treatment rationale of fractured posterior teeth. J Am Dent Assoc. 1978;97(5):806-810.
31. Turp JC, Gobetti JP. The cracked tooth syndrome: an elusive diagnosis. J Am Dent Assoc. 1996;127(10):1502-1507.
32. Davis R, Overton JD. Efficacy of bonded and nonbonded amalgam in the treatment of teeth with incomplete fractures. J Am Dent Assoc. 2000;131(4):469-478.
33. Rosen H. Operative procedures on mutilated endodontically treated teeth. J Prosthet Dent. 1961;11(5):973-986.