You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Hypertension affects more than 1 billion people worldwide and is a leading cause of morbidity and mortality.1,2 As per the blood pressure (BP) thresholds by the American College of Cardiology/American Heart Association (AHA) 2017 guidelines, between 2013 and 2016, 46% of the US adult population, or approximately 116.4 million adults, had hypertension, which is defined as blood pressure ≥130/80 mm Hg. The prevalence was seen to increase with age. Prevalence was 26.1% among people aged 20 to 44 years, 59.2% among those aged 45 to 64 years, and 78.2% among those aged ≥65 years. A higher percentage of males had hypertension in the age group up to 64 years, whereas more females were seen to develop hypertension in the population ≥65 years of age.1 Those who are normotensive at age 55 to 65 and survive to age 80 to 85 have a 90% lifetime risk of developing hypertension during the remaining years of life.3,4
Hypertension is a significant risk factor for cerebrovascular disease and stroke.1 In 2015, an estimated 7.8 million deaths globally could be attributed to systolic blood pressure (SBP) >140 mm Hg.1 The number of deaths between 1990 and 2015 did not increase in high-income countries but increased in middle- and low-income countries.1 Hypertension is usually asymptomatic until complications occur.5Hence, it is not surprising that 35% of US adults with hypertension are unaware that they have it.1 Typically, many patients avoid seeking medical or dental care until they are in pain or until serious symptoms arise. Thus, dentists are in a unique position to identify undiagnosed hypertensive patients, refer them to a physician for appropriate medical care, and educate them regarding lifestyle modifications and the risks associated with uncontrolled high blood pressure. Unfortunately, approximately 50% of patients do not comply with taking their medications as directed.6
Guidelines and Classification
The risk for cardiovascular disease (CVD) doubles for each rise of 20/10 mm Hg in systolic/diastolic blood pressure.3,7 From blood pressure levels as low as 115/75 mm Hg upward, the risk of death from both ischemic heart disease and stroke increases, with the increase being progressive and linear.3 Because of this continuous association between high blood pressure and increased cardiovascular risk, categorization of blood pressure levels is useful for clinical and public health decision making.8
Guidelines have evolved considerably since the publication of the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines in 2003.3 The JNC 7 (overseen by the National Heart, Lung, and Blood Institute) classified blood pressure in four stages: normal (<120/<80 mm Hg), prehypertension (120-139/80-89 mm Hg), stage 1 hypertension (140-159/90-99 mm Hg), and stage 2 hypertension (≥160/≥100 mm Hg). Recommendation was made to initiate antihypertensive drug therapy at stage 1 hypertension. In case of diabetic patients or patients with chronic kidney disease, it was recommended to start therapy at BP level of 130/80 mm Hg.3
The 2017 guidelines by American College of Cardiology/American Heart Association (ACC/AHA) in association with nine other professional societies are considered a successor to the JNC 7 guidelines.9
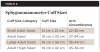
Hypertension in the new guidelines is defined as systolic blood pressure of 130 mm Hg or higher and diastolic blood pressure of 80 mm Hg or higher in adults. These guidelines classify blood pressure into four categories. CVD risk increases as blood pressure increases from normal (<120/<80 mm Hg) to elevated (120-129/<80 mm Hg) to hypertension stage 1 (130-139/80-89 mm Hg) to hypertension stage 2 (≥140/≥90 mm Hg).7,10 (A comparison of blood pressure categories under the 2003 JNC 7 guidelines versus the 2017 ACC/AHA guidelines is provided in Table 1.3,7) The relative risk from CVD increases twofold in people with stage 1 hypertension as compared with those who are normotensive.4 An SBP goal of <120 mm Hg results in fewer CVD events and improved survival rate than an SBP goal of <140 mm Hg among patients with SBP ≥140 mm Hg and who are at a high risk for CVD but do not have a history of stroke or diabetes.1,11 Patients with stage 1 and stage 2 hypertension are recommended to consult a healthcare provider for further treatment.7
Physiology of Blood Pressure Regulation
Blood pressure is the pressure of circulating blood against the walls of blood vessels. It is determined by how much blood the heart pumps and the resistance offered by the systemic circulation, ie, cardiac output and systemic vascular resistance. Cardiac output is a function of stroke volume and heart rate, and systemic vascular resistance is dependent on vascular structure, tone, and blood volume. Blood pressure is never constant.5 Systolic blood pressure is the pressure at the peak of ventricular contraction. After the contraction of the left ventricle, the total resting resistance in the arterial system is known as the diastolic blood pressure.12 When the blood pressure during a single cardiac cycle is averaged, it is known as mean arterial pressure.13
Blood pressure is regulated by changes in cardiac output and systemic vascular resistance through multiple physiological systems, including the central nervous system, peripheral nervous system, and renin-angiotensin-aldosterone system. Other regulating factors are blood volume; vasoconstrictors like catechol, endothelin, and vasopressin; vasodilators like nitric oxide and prostaglandins; myogenic factors intrinsic to small arteries; and tissue factors like adenosine, potassium ion, hydrogen ion, and histamine. All contribute in regulating the blood pressure.5 Short-time regulation of blood pressure is via baroreflexes, which come into action within seconds, and vasoactive hormones, which are activated in minutes,14 whereas long-term regulation is done through the kidney fluid volume regulation system.14,15
Etiology and Risk Factors for Hypertension
Ninety percent of people with hypertension have primary or essential hypertension where there is no specific underlying cause but abnormalities of one or more of the aforementioned regulatory mechanisms have caused a failure in the regulation of vascular resistance.12 Increased sympathetic neural activity is a contributing factor to primary hypertension. High sodium intake has been shown to contribute to this condition by triggering neuromodulator signals, thereby activating the sympathetic nervous system, which leads to increased renin secretion by the kidneys.15 Other contributing factors include genetic factors,16 obesity and weight gain, increased angiotensin II activity, and mineralocorticoid excess.
Due to age-related alterations in the cardiovascular system, aging is a risk factor for developing hypertension, especially systolic hypertension.1 Before age 50, isolated diastolic hypertension or a combination of diastolic hypertension and elevated systolic blood pressure is common. After age 50, isolated systolic hypertension is common, as only systolic blood pressure rises with increasing age while diastolic blood pressure either plateaus or decreases.12
Diastolic hypertension puts people younger than 50 years old at a higher CVD risk than systolic hypertension does. In people older than 50, systolic hypertension is a more significant risk factor.3,12 The prevalence of hypertension also varies with race. Non-Hispanic black people in the United States have the highest prevalence of hypertension at 57.6%, which is among the highest in the world.1 Additional factors associated with increased blood pressure progression include lack of exercise, alcohol intake, cigarette smoking, anger, symptoms of depression, and stress.1
Hypertension caused by a specific disease or abnormality is known as secondary hypertension. This condition accounts for 10% of the patients with hypertension and may be a cause for abrupt onset of hypertension, presence of hypertension in patients less than 30 years of age, development of diastolic hypertension in those older than 65 years of age, or sudden increase in blood pressure that had been well controlled by antihypertensive medications. The most common cause of secondary hypertension is renal parenchymal disease, followed by renovascular disease and primary aldosteronism. Obstructive sleep apnea is present in 80% of cases of resistant hypertension. Nonsteroidal anti-inflammatory drugs (NSAIDs), sodium-containing antacids, oral contraceptives, cocaine, caffeine, and neuropsychiatric agents are among the drugs that can lead to the development of hypertension. Coarctation of aorta, pheochromocytoma, and hyper- and hypothyroidism are some of the less common causes for development of secondary hypertension.7
Diagnosis of Hypertension
Accurate measurement of blood pressure is the foundation for a correct diagnosis and classification of hypertension. Intra-arterial catheter is the best means of measurement, but it is invasive and impractical. Hence, a sphygmomanometer and bell of a stethoscope are commonly used in an office-based setting.6 Types of sphygmomanometers are mercury, aneroid, or a hybrid, with mercury being considered the most accurate. Over time aneroid devices have become the most widely used along with digital/automatic arm, wrist, or finger devices that do not need a stethoscope.16 The accuracy of these devices should be regularly calibrated against a mercury sphygmomanometer.6,16
The 2017 ACC/AHA guidelines reinforce key steps for accurate measurement of blood pressure. The patient should be sitting relaxed in a chair with feet on the floor and back supported for at least 5 minutes before blood pressure measurement. The patient should avoid caffeine, exercise, and smoking for at least 30 minutes prior to measurement, and his or her bladder should be emptied. The correctly sized cuff should be selected wherein the bladder of the sphygmomanometer encircles 80% of the patient's arm.7 Falsely elevated values will be recorded if a cuff is excessively small or placed loosely. If the cuff is too large or placed too tightly, low values will be recorded.6 To select the right cuff size, the arm circumference should be measured at midpoint of the upper arm.17 (See Table 2 for cuff sizes.7) Placement of the middle of the cuff on the upper arm should coincide with the level of the right atrium or the midpoint of the sternum. The cuff should be centered over the brachial artery.7 The fit should allow space for about two finger widths.17 Blood pressure should be recorded in both arms. Subsequent readings from the arm that gave the higher reading should be taken after an interval of 1 to 2 minutes. These guidelines recommend using an average of two or more readings obtained on two or more occasions to estimate the individual's blood pressure level.7
It has been estimated that around 20% of patients with elevated blood pressure during a visit to a dental/medical practitioner have "white coat hypertension."18 This is defined as consistently elevated blood pressure only in the presence of a healthcare worker but not elsewhere.6 Offering reassurance to the patient to reduce stress and anxiety and use of pharmacological sedation can help lower the blood pressure. To achieve an accurate diagnosis, self-monitoring at home or ambulatory blood pressure measurement over a 24-hour period is beneficial. These readings are averaged, and often patients are found to have normal blood pressure levels. Sometimes, though, these ambulatory readings may reveal "masked hypertension," which is when the patient has a normal blood pressure in the physician's office but the readings taken over a span of 24 hours reveal that hypertension is present.6 In the 2017 ACC/AHA guidelines, routine out-of-office and self-monitoring of blood pressure is recommended to overcome the known frequent inconsistencies between office and home values. This helps to confirm the diagnosis of hypertension and for titration of antihypertensive medications in combination with telehealth counseling and clinical intervention.7,10
Signs, Symptoms, and Complications of Hypertension
A person with hypertension may remain asymptomatic for years. Nonspecific symptoms like headache or dizziness may appear in the early stages, but usually the only sign is an elevated blood pressure, and the disease often is diagnosed only at a routine office visit or when complications due to persistently elevated blood pressure arise.12,19
Hypertension leads to thickening of internal elastic lamina, hypertrophy of smooth muscle, and deposition of fibrous tissue in larger arteries.19 In smaller arteries, the lumen narrows due to thickening of the vessel wall by deposition of hyaline. This causes atheroma and atherosclerosis in the vasculature, ultimately leading to end organ damage of the brain, retina of the eye, kidneys, and heart.19 On ophthalmoscopic eye examination, early changes of hypertension can be observed as narrowing of retinal arterioles.3 In acute or advanced hypertension, this progresses to papilledema and retinal ischemia, which could manifest as blot-hemorrhages and cotton wool exudates.3,19
Other signs and symptoms that develop in the later stages of uncontrolled hypertension are indicative of end organ damage. These include proteinuria, hematuria, and chronic renal failure due to hypertensive nephropathy. Cerebrovascular accident, dementia, and hypertensive encephalopathy with symptoms of confusion, headache, and convulsions due to brain damage may develop. Myocardial infarction (MI), angina pectoris due to coronary artery disease, and left ventricular hypertrophy leading to congestive heart failure are some of the late-stage cardiac changes that may occur.In the case of secondary hypertension, other signs and symptoms may be present due to underlying cause.12
When a physician evaluates a patient for hypertension, in addition to a thorough medical history, a complete physical examination is performed. Also, laboratory tests are ordered to try to detect conditions that could be causing hypertension or to assess for any resulting organ damage from high blood pressure. Electrocardiogram (ECG) is obtained to evaluate for damage to the heart, including MI and left ventricular hypertrophy, which are common complications of hypertension. Blood tests are taken for measurement of electrolytes, like potassium, to assess for primary aldosteronism and Cushing syndrome, which are causes of secondary hypertension. Blood glucose is measured, as elevated blood sugar is a possible complication of hypertension. Other tests include hematocrit, to assess polycythemia, which can contribute to systemic hypertension; blood urea nitrogen, creatinine levels, and urinalysis, to assess for renal and renovascular disease; and fasting lipid profile, to evaluate risk for a potential cardiovascular event. Additional tests may include ultrasound of the kidney and computed tomography (CT) of the abdomen for further assessment of kidneys and adrenal glands. Depending on the results of these tests, further evaluation may be warranted, and management protocol will be determined.3,20
Treatment
According to the World Health Organization, about 60% of CVD and 50% of ischemic heart disease can be attributed to hypertension, which is also a leading risk factor for death. Yet the prevention and management of hypertension is still a significant challenge.3,21 The goal of treatment is reduction of blood pressure to lower the incidence of coronary artery disease, stroke, and heart failure.In individuals who are at a greater risk for CVD, lowering of blood pressure results in a greater reduction of absolute CVD risk. Hence, the 2017 ACC/AHA guidelines recommended estimating the 10-year atherosclerotic cardiovascular disease (ASCVD) risk by using the ASCVD risk calculator.7 The risk is calculated on the basis of different variables, including the patient's age, sex, race, level of total and HDL cholesterol, systolic blood pressure, antihypertensive medications, history of diabetes, and smoking status reflecting the lifetime exposure to tobacco. To overcome issues of miscalibration, however small it may be, clinical judgment and other risk enhancers are used.22
For patients with hypertension and clinical CVD or who have greater than 10% risk for 10-year ASCVD event, blood pressure level of 130/80 mm Hg is "recommended." For those without the markers for increased CVD risk, target blood pressure level of 130/80 mm Hg is "reasonable."7 A combination of lifestyle modifications and pharmacological therapy is recommended for lowering blood pressure in patients in accordance with their blood pressure levels, CVD risk, and co-morbid conditions.
Lifestyle Modifications
A healthy lifestyle is recommended for maintaining optimal blood pressure or reducing an elevated blood pressure. In patients who are overweight or obese, a 10-lb weight reduction can lower SBP by about 5-10 mm Hg and even prevent hypertension.3,7 Maintaining a normal body index of <25 Kg/m2 is recommended. A dietary approach to stop hypertension (DASH) should be adopted; such a plan emphasizes eating vegetables, fruits, low-fat dairy foods, whole grains, poultry, fish, and nuts, with a reduction of red meat and sugar and decreased consumption of total and saturated fats and cholesterol. Patients with hypertension may see an expected impact of about 11 mm Hg reduction in SBP after adopting a DASH diet.7 Reduction in sodium intake to no more than 1500 mg per day has been found to reduce SBP by 5-6 mm Hg in a hypertensive patient.Potassium supplementation, targeting 3500-5000 mg per day, is also recommended unless contraindicated due to chronic kidney disease. Aerobic activity of 30 to 45 minutes most days of the week in a structured exercise program has been shown to reduce SBP by 4-8 mm Hg in a hypertensive patient and 2-4 mm Hg in a normotensive patient.7
Limiting alcohol intake to no more than 1 ounce or 30 mL of ethanol per day (equivalent to no more than two drinks per day for men and no more than one drink per day for women) is recommended.3,7 Reduction in blood pressure correlates to the amount of reduction in the consumption of alcohol in a dose-dependent manner.23 Reduction in consumption of alcohol has been shown to reduce SBP between 3-4 mm Hg.7,24 For people who drink two or fewer drinks per day, reducing consumption does not have a significant blood pressure reduction. Thus, there seems to be a threshold effect at two drinks per day.23
Pharmacological Therapy
Along with lifestyle modifications aimed at improving health, drug therapy is recommended in patients with stage 2 hypertension. It is also recommended in patients with stage 1 hypertension and either a 10-year risk for heart disease and stroke of at least 10% or existing clinical CVD, diabetes mellitus, or chronic kidney disease. 7,8 Any commonly used antihypertensive drug regimen would reduce the risk for a total major cardiovascular event. The risk reduction for such an event would be greater for a greater reduction in blood pressure.25
For stage 1 hypertension, one antihypertensive medication is reasonable; for stage 2 hypertension, a combination of two first-line antihypertensive medications of different classes is recommended. The response to initial therapy will determine any subsequent changes, titration, or more intensive therapy.7 Patients with baseline SBP of <140 mm Hg benefit the most from intense lowering of blood pressure. This is in contrast to those with a high baseline SBP, who show greater incidence of adverse events without any clinical benefit.26
Recommended first-line drug therapy includes thiazide diuretics, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers, and calcium channel blockers. Prototypes of these drugs are hydrochlorothiazide, lisinopril, losartan, and amlodipine and diltiazem, respectively. Secondary agents include diuretics, beta blockers, direct renin inhibitors, alpha 1 blockers, and direct vasodilators. The hemodynamic effect of most antihypertensive drugs is reduction of the total peripheral resistance (TPR). Certain drug classes like thiazides initially decrease cardiac output and increase the TPR, but long-term they decrease the TPR thereby reducing the blood pressure. To improve adherence, once-daily dosing is recommended instead of multiple times daily.7
Dental Management
The dentist is an integral member of the patient's healthcare team and may be the first to detect undiagnosed hypertension or find that hypertension is uncontrolled despite pharmacological intervention. The dentist can then refer the patient to his or her physician for appropriate care.27 Routine blood pressure measurement should be part of a dental patient's assessment and health screening. This also provides an opportunity for the dentist to talk about healthy lifestyle and encourage a hypertensive patient to adhere to a medication regimen prescribed by the physician.
If a patient is known to be hypertensive, this should be documented, including how the patient is being treated and which hypertensive medications are prescribed along with their dosages and frequency. Any symptoms associated with hypertension should be assessed, and appropriate referrals made.12
The chief concern while treating a hypertensive patient is an acute increase in blood pressure during the procedure, which can potentially lead to arrythmia, angina, MI, or stroke.28 Before starting any treatment, it must be determined whether the patient can undergo dental procedures safely, giving consideration to the risk associated with the planned procedure, risk associated with the patient's cardiovascular status and functional reserve, and the blood pressure thresholds.
The ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery stratified the risk of stroke, MI, or heart failure with any noncardiac surgical procedure.29 Uncontrolled systemic hypertension, with blood pressure >180/110 mm Hg, is categorized as a "minor cardiovascular risk." Mild angina pectoris, previous MI, prior heart failure, diabetes mellitus, and renal insufficiency are stratified as intermediate risk. Acute or recent MI, unstable or severe angina, unstable coronary syndrome, decompensated heart failure, significant arrythmias, high-grade atrioventricular block, and severe valvular diseases are considered major risk (Table 3).12,29
With regard to type of surgery, head and neck surgery is categorized as intermediate risk with cardiac risk 1% to 5%. Superficial surgical procedures, which include periodontal procedures and minor oral surgery, are low risk, ie, the cardiac risk is less than 1%. The last category is for the risk imposed by functional reserve or capacity. Metabolic equivalents (METs) are used for assessment of a patient's capacity to conduct specific physical activities.12,29 Most daily activities, like eating or doing daily household chores, are equivalent to 1 to 4 METs. Taking a short run or walking up a flight of stairs equates to 4 to 10 METs, while engaging in more strenuous activity like playing sports such as tennis or football equals to >10 METs.6 A patient who cannot meet a 4-MET demand is at an increased cardiac risk.
When dentists are treating patients with upper level stage 2 hypertension, the blood pressure cuff should be left on for periodic intraoperative blood pressure monitoring, and the appointment should be terminated if the blood pressure rises above 180/110 mm Hg. Elective care should not be performed with blood pressure above 180/110 mm Hg. If there are no associated symptoms, referral to be seen by a physician within a week is highly recommended. If symptoms are present, like headache, nausea, chest pain, or shortness of breath, immediate evaluation by a physician is mandated.12,18,28 If urgent dental care is needed due to the presence of swelling/infection, benefits over possible risk should be weighed; in consultation with a physician, procedures may be performed with ECG, BP monitoring, and an intravenous line.12
A concern among dentists is that epinephrine in local anesthetic solutions can contribute to an adverse cardiovascular response. A systematic review has established that epinephrine in local anesthetic has minimal effect.3,30 Moreover, no significant changes occur in blood pressure and pulse rate of hypertensive patients undergoing dental extraction under local anesthetic with epinephrine.31 Several studies have concluded that total dose of epinephrine of about 0.036 mg to 0.054 mg, which is equivalent to two to three cartridges of lidocaine with 1:100,000 epinephrine, brings about slight if any cardiovascular changes.6,28,30 Greater quantities of epinephrine come at a higher risk but are well tolerated. All of these scenarios assume there is no intravascular injection of local anesthesia.
Epinephrine is released by the adrenal medulla and stimulates alpha and beta receptors on various tissues.18 It causes vasoconstriction through alpha-1 adrenergic receptors on the vasculature of the skin and mucous membrane and acts on beta-2 adrenergic receptors on the vasculature in skeletal muscles to cause vasodilation. In response to stress or pain, a patient can release 40 times his or her baseline levels, which is much greater than the amount of epinephrine in two to three dental cartridges.6,32 Patients with blood pressure >180/110 mm Hg are to be deferred, but in case of urgent dental care, the use of epinephrine should be discussed with a physician.12
Epinephrine in local anesthetic should be used cautiously in patients on nonselective beta blockers like propranolol and nadolol. The interaction can lead to unopposed alpha vasoconstriction by epinephrine, which can lead to hypertensive crisis as well as bradycardia. Therefore, epinephrine administration should be limited to no more than two cartridges of 1:100,000 solution.33 After administration of one to two cartridges of 1:100,000 epinephrine concentration, blood pressure and heart rate should be rechecked if the patient is on a tricyclic antidepressant like imipramine, amitriptyline, or doxepin. These medications can potentiate the effect of epinephrine and cause an increase in systolic blood pressure and dysrhythmia, although this risk of interaction decreases with prolonged use of the antidepressant.34,35
Epinephrine should be used with precaution when patients are on COMT (catechol-o-methyl-transferase) inhibitors like tolcapone and entacapone, which are prescribed in the management of Parkinson's disease, as the combination can cause tachycardia. Thus, after administration of a cartridge of 1:100,000 epinephrine, blood pressure and pulse should be monitored.36 Another recommendation regarding epinephrine is to avoid the use of impregnated gingival retraction cord in patients with poorly controlled hypertension.6,12
In a long procedure involving multiple quadrants, injections should be given one quadrant at a time, and blood pressure should be monitored intraoperatively.6 If general anaesthesia is to be administered to a patient using antihypertensive medications, there is a risk for the patient to develop hypotension. Hence, blood pressure should be closely monitored.3
Other recommendations for dental management of hypertensive patients include stress/anxiety reduction by establishing a good rapport with the patient, scheduling short morning appointments, and administering nitrous oxide and/or premedication with sedative/anxiolytic agents taken 1 hour before the appointment.12 Rapid changes in chair positioning should be avoided due to the possibility of orthostatic hypotension, which is a side effect of certain antihypertensive medications.12 Various side effects may be seen in the oral cavity that are related to intake of antihypertensive medications; for example, ACE inhibitors, thiazides, and loop diuretics can cause xerostomia and dental caries, especially root caries.18 Changing the class of medications, if possible, usually resolves these adverse effects. Use of pilocarpine is indicated along with frequently sipping water and sucking on sugarless candy. Calcium channel blockers, particularly dihydropyridines like amlodipine and nifedipine, can induce gingival overgrowth.18 Several studies indicate a genetic predisposition. Because plaque is a significant risk factor, good oral hygiene should be maintained and professional cleaning is advised. Gingival surgery, including gingivectomy and laser-assisted excision, is effective in treating drug-induced gingival overgrowth, although recurrence is common.37 Lichenoid reactions like lichen planus have been seen due to medications like furosemide, methyldopa, captopril, and beta blockers. Taste alteration can also be a side effect of medications.37
Conclusion
In summary, nearly half of the US adult population has hypertension, especially with the change in guidelines in 2017, which removed the category of prehypertension and classified blood pressure over 130/80 mm Hg as stage 1 hypertension. When patients visit a dental office, the dentist is given a unique opportunity to identify this problem, educate the patients, and refer them if they are unaware of it or non-compliant. Dental care can be provided for a patient whose blood pressure is below 180/110 mm Hg, but the dentist must assess whether there are any co-morbid conditions that may place the patient at an even higher CVD risk. Although dental treatment can be done in patients with stage 1 or stage 2 hypertension, they should still be referred to a physician for evaluation and to bring the blood pressure under control, as SBP >115 mm Hg is responsible for 62% of cerebrovascular disease and 49% of ischemic heart disease, and is the number one attributable risk factor for death throughout the world.3
Dentists can provide treatment safely by utilizing anxiety-reduction protocols and monitoring blood pressure throughout the procedure when the patient is on the higher end of stage 2 hypertension or if the procedure is long. The patient should be evaluated and managed with regard to side effects of various antihypertensive medications. Two to three cartridges of local anesthetic with lidocaine can be safely given to a patient with hypertension.
About the Authors
Brahmleen Kaur, DMD
Clinical Instructor, Department of Oral and Maxillofacial Surgery, Rutgers School of Dental Medicine, Newark, New Jersey
Vincent B. Ziccardi, DDS, MD
Professor, Chair, and Residency Director, Department of Oral and Maxillofacial Surgery, Rutgers School of Dental Medicine, Newark, New Jersey; Fellow,
American College of Surgeons
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Benjamin EJ, Muntner P, Alonso A, et al, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2019 update: a report from the American Heart Association [published correction appears in Circulation. 2020;141(2):e33]. Circulation. 2019;139(10):e56-e528.
2. Ezzati M, Lopez AD, Rodgers A, et al, Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347-1360.
3. Chobanian AV, Bakris GL, Black HR, et al, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572.
4. Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: the Framingham Heart Study. JAMA. 2002;287(8):1003-1010.
5. Klabunde RE. Cardiovascular Physiology Concepts. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins/Wolters Kluwer; 2012.
6. Bavitz JB. Dental management of patients with hypertension. Dent Clin North Am. 2006;50(4):547-562.
7. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269-1324.
8. Detailed Summary From the 2017 Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Dallas, TX: American Heart Association; 2017. http://professional.heart.org/idc/groups/ahamah-public/@wcm/@sop/@smd/documents/downloadable/ucm_497446.pdf. Accessed August 4, 2020.
9. American College of Cardiology. New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension. American College of Cardiology website. November 13, 2017. https://www.acc.org/latest-in-cardiology/articles/2017/11/08/11/47/mon-5pm-bp-guideline-aha-2017. Accessed August 4, 2020.
10. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017;318(21):2132-2134.
11. SPRINT Research Group, Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103-2116.
12. Little JW, Miller CS, Rhodus NL. Little and Falace's Dental Management of the Medically Compromised Patient. 9th ed. Elsevier Mosby; 2017:38-52.
13. Zheng L, Sun Z, Li J, et al. Pulse pressure and mean arterial pressure in relation to ischemic stroke among patients with uncontrolled hypertension in rural areas of China. Stroke. 2008;39(7):1932-1937.
14. Guyton AC. Blood pressure control-special role of the kidneys and body fluids. Science. 1991;252(5014):181-1816.
15. Bolivar JJ. Essential hypertension: an approach to its etiology and neurogenic pathophysiology. Int J Hypertens. 2013;2013:547809.
16. Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015;
386(9995):801-812.
17. Williams JS, Brown SM, Conlin PR. Videos in clinical medicine. Blood-pressure measurement. N Eng J Med. 2009;360(5):e6.
18. Hogan J, Radhakrishnan J. The assessment and importance of hypertension in the dental setting. Dent Clin North Am. 2012;56(4):731-745.
19. Ralston SH, Penman ID, Strachan MWJ, Hobson RP. Davidson's Principles and Practice of Medicine. 23rd ed. Elsevier Ltd; 2018.
20. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-520.
21. World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life. Geneva, Switzerland: World Health Organization; 2002. https://www.who.int/whr/2002/en/whr02_en.pdf?ua=1. Accessed August 4, 2020.
22. American Heart Association. 2013 Prevention Guidelines Tools CV Risk Calculator. AHA website. https://professional.heart.org/professional/GuidelinesStatements/ASCVDRiskCalculator/UCM_457698_. Accessed August 4, 2020.
23. Roerecke M, Kaczorowski J, Tobe SW, et al. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2(2):e108-e120.
24. Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38(5):1112-1117.
25. Turnbull F, Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet. 2003;362(9395):1527-1535.
26. Sun X, Guo Y, Nie Z, et al. Influence of baseline systolic blood pressure on the relationship between intensive blood pressure control and cardiovascular outcomes in the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Res Cardiol. 2019;108(3):273-281.
27. Miller CS, Glick M, Rhodus NL. 2017 Hypertension guidelines: new opportunities and challenges. J Am Dent Assoc. 2018;149(4):229-231.
28. Herman WW, Konzelman JL Jr, Prisant LM, Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. New national guidelines on hypertension: a summary for dentistry. J Am Dent Assoc. 2004;135(5):576-584.
29. Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery): developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Circulation. 2007;116(17):e418-e499.
30. Bader JD, Bonito AJ, Shugars DA. A systematic review of cardiovascular effects of epinephrine on hypertensive dental patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93(6):647-653.
31. Gungormus M, Buyukkurt MC. The evaluation of the changes in blood pressure and pulse rate of hypertensive patients during tooth extraction. Acta Med Austriaca. 2003;30(5):127-129.
32. Knoll-Köhler E, Frie A, Becker J, Ohlendorf D. Changes in plasma epinephrine concentration after dental infiltration anesthesia with different doses of epinephrine. J Dent Res. 1989;68(6):1098-1101.
33. Hersh EV, Moore PA. Three serious drug interactions that every dentist should know about. Compend Contin Educ Dent. 2015;36(6):408-413.
34. Becker DE. Psychotropic drugs: implications for dental practice. Anesth Prog. 2008;55(3):89-99.
35. Lambrecht JT, Greuter C, Surber C. Antidepressants relevant to oral and maxillofacial surgical practice. Ann Maxillofac Surg. 2013;3(2):160-166.
36. Hersh EV, Moore PA. Adverse drug interactions in dentistry. Periodontol 2000. 2008;46:109-142.
37. Aral CA, Dilber E, Aral K, et al. Management of cyclosporine and nifedipine-induced gingival hyperplasia. J Clin Diagn Res. 2015;9(12):ZD12-ZD15.