You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
It has become a familiar scenario. A woman becomes ill on an international flight. Her condition deteriorates rapidly and, on arrival, she is rushed to the hospital with a high fever from which she may or may not recover. The incident may be briefly mentioned on a local newscast, but then the disease recurs in other places around the world. Soon the mystery ailment is given a name that, although not terribly informative, at least provides a convenient label. Reaction from officials is mixed, and public health measures, increasingly draconian, are instituted in an attempt to limit the spread of this unknown illness. In time, the disease is brought under some degree of control, and things essentially return to normal.
While seasonal influenza occurs every year, in 2003 severe acute respiratory syndrome, or SARS, was the culprit.1 Thanks to quick action by the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and other public health agencies, the medical community already knew a great deal about SARS.2,3 It is caused by a coronavirus similar to those that cause some cases of the common cold. When the authors (MJ) wrote about this in 2003, the likely outcome of the SARS problem appeared serious but perhaps not catastrophic.1 As it turned out, this optimistic forecast proved to be roughly correct, at least in the United States. Despite much suffering and death among those infected, life went on mostly as usual.
In early 2020, a new and different threat arose. Its symptoms and mode of transmission (primarily airborne) are the same as SARS. Both SARS and the new disease, COVID-19, are caused by coronaviruses and share similar characteristics, especially their severity and high mortality rates (1% to more than 10% depending on how reported) and an apparently greater likelihood of transmission. Seasonal influenza is caused by numerous and changing groups of viruses and, for most people, is much less serious.
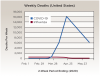
Figure 1 illustrates weekly (not cumulative) mortality rates attributed to COVID-19 and flu in the spring of 2020, based on a CDC review of death certificates.4It shows the dramatically higher rate of COVID-19 deaths, as well as an encouraging decline in both curves after widespread public health measures were adopted. At this writing, an alarming uptick of COVID-19 is occurring in some regions, which is probably the combined result of business reopenings and a general "lockdown fatigue." Table 1 compares selected aspects of seasonal influenza, SARS, and COVID-19.1-6
Hierarchy of Evidence
Clinicians have been trained to base decisions on best evidence. There is much evidence swirling around COVID-19, however not all of it is good or actionable. Figure 2 illustrates the hierarchy of evidence that underlies responsible decision-making in medicine and dentistry.7 At the top of the hierarchy is the randomized controlled clinical trial (RCCT), which yields the strongest evidence that an effective way has been found to control and treat this or any disease. Strong, appropriate evidence is needed before any new test, vaccine, or antiviral drug could be accepted. Climbing the pyramid is normally a multi-year, multi-million-dollar process, with extensive oversight (in the United States) by the Food and Drug Administration (FDA). But given the extraordinary circumstances in the current climate, there simply may not be time to follow the normal path. As illustrated on the right side of Figure 2, case reports assume a heightened evidentiary role as work continues on studies that are more definitive.
Not included in the well-ordered pyramid of clinical evidence is a plethora of essentially worthless information, including what is known as "junk science," that is not based on evidence and may have more to do with ignorance or self-serving interests.8 Much of this unreliable information is driven by rumor, tradition, hype, politics, or even fraud or sabotage, and it may have acquired its "proof" by intimidation or endorsement. Sometimes a "natural" solution is equated with being "good." Most of this dubious information is easy enough to see through; however, "junk science" can be more difficult to navigate. This consists of publications or presentations that appear to be scientific but are so flawed as to lack any claim to credibility. Ulterior motives, such as product promotion, career advancement, grievance, prejudice, or ideology, are usually evident or easily discoverable. Junk science can be laughable and/or infuriating, but it could also be deadly.
With regard to real evidence, in a time of worldwide emergency, shortcuts are inevitable. Drugs, devices, and test kits are almost certain to be fielded without the normal evidential backing, as has been seen in the current pandemic. But mechanisms exist to keep such "emergency uses" rational and safe. In the United States the responsibility falls to the FDA and CDC, which must issue some form of limited emergency approvals on the basis of whatever evidence does exist, however imperfect.
There is also a heightened responsibility for all clinicians and physicians to report adverse events and side effects for both new and existing COVID-19 drugs and tests. The FDA looks for patterns of problems, including unsuccessful outcomes besides adverse events and side effects. Rare but important deficiencies that may be undetectable in even a massive RCCT will materialize when a new drug is tried in millions of patients. Since it is critical that these flaws be reported, interpreted, and acted upon swiftly, clinicians need to take a careful medical history of patients and report side effects (even those that may not seem to be related to the treatment) to the FDA promptly. For a marketed drug, this is termed "post-market surveillance."9
Practitioners who choose to use a drug beyond its FDA approval have a heightened burden of responsibility to select and apply treatment based on an individual reading of the evidence. This is termed "off-label" use.10
It is important to note that federal agencies, including the National Institutes of Health (NIH), are almost never in a position to carry an idea from basic science through development and testing in clinical trials. To conquer any disease, a partnership among academia, medical centers, industry, and practitioners is critical.11
Muddled Forecasts
The predictions that have come forth regarding COVID-19 have been confusing, inconsistent, and largely inaccurate. In a rush to develop testing for this disease12 some inaccurate tests have resulted in wrong diagnoses and/or estimates of the incidence of COVID-19. Worse still is that uncertainty remains as to who should be treated, be isolated, or return to work. Highly sophisticated models have been developed by very capable analysts, but such models are limited by the data put into them. As the saying goes, "garbage in, garbage out."
This is not to suggest that forecasts be ignored, only that they are inherently limited to current knowledge and small perturbations of the current situation. These forecasts are crucial to decisions about how and when to relax restrictions. Given the current state of the science, however, there is reason to expect this pandemic to be around for a long time and affect a great number of people. But there is always hope.
Immunity Above All
The overarching hope is for immunity, whether acquired from a vaccine or from a mild course of the infection itself. The hope is that nature will render survivors immune, at least for a while, and that an effective vaccine will be developed soon.13 The hope is also for treatments that work, including new approaches to care, in and out of the hospital. Patients often ask about such approaches.
The path to natural immunity starts with infection, which causes (among other things) the body to produce a number of antibodies-the immunoglobulins-in several steps. Of these, IgM typically gives the first stage of immunity; later, IgG usually confers longer-term immunity. IgA, found in secretions such as tears and saliva, is responsible for secretory immunity, whose role in COVID-19 is unknown. Ongoing basic scientific studies aim to determine if and when immunity is conferred by these immunoglobulins, and if so, how long it lasts. At this writing, however, this simply is unknown.
There are two major approaches to vaccines.13 The first is "active" immunity, conferred when a patient receives an active but less potent form of the virus. The patient's own immune system then goes to work rendering the patient immune to the virus. The second approach is "passive" immunity, which is when the patient receives an inactivated form of the virus. Many viruses, such as those that cause influenza, are notorious for mutating, so that an old vaccine is no longer effective; hence the need for new flu vaccines every year. For this reason, a critical element of vaccine development is the identification and targeting of parts of the virus that are conserved, ie, not subject to frequent mutations. Thus far, it seems that COVID-19, fortunately, is not prone to rapid mutations.
A variation of vaccination, known as "convalescent plasma" treatment,14 is being tried as a treatment for some seriously ill patients. Patients who have recovered from a COVID-19 infection can donate a fraction of their blood, which contains the appropriate antibodies, to help another person fight the disease. Again, at this writing, whether or not this works is yet unknown.
Testing: Why and How?
Much emphasis is being placed on development of reliable tests for COVID-19,15-19 meaning low false-positive and still lower false-negative rates. While this objective has yet to be fully achieved, several promising possibilities are emerging from reputable laboratories, including the CDC itself. Testing is critical both for the individual and the population as a whole. Accurate testing may determine when treatment has been successful and it is reasonably safe to return to workplaces.
On a community or population level, testing gives an estimate of the incidence and path of COVID-19 infections, from which models can calculate how many new cases can be expected in a particular geographic area. This information is essential to planning for the supplies, equipment, drugs, gases, and personnel needed to manage the disease.
Testing on the community level provides an indication of when "herd immunity" has been reached, which is the absolute essential condition needed if this virus is to be brought under lasting control. It is generally accepted that 85% to 90% of the population should be immune to COVID-19 so that individuals who are unable or unwilling to take a vaccine are unlikely to become ill.4
Treatments
While a vaccine is the "sine qua non" of long-term success, an immediate need exists for treatments that are effective against COVID-19. Massive research projects are underway in both of these areas, although antiviral drugs seem to receive the most press attention, with promising candidates often touted. The same genetic sequencing technology greatly facilitates both vaccine and antiviral development, but neither is quick, easy, or sure.
A few words on anti-malarial drugs are worth noting. One such drug, chloroquine, has been promoted to treat COVID-19. Some studies have given it credit, while others have shown this use of the drug to be both unsafe and ineffective, and its recent history offers an object lesson on how even seemingly reliable reports must be used with care. In this case, the rush to publish led prestigious journals to rapidly review and present studies online, ahead of print.20-25 Subsequently, flaws in the clinical trial design and the authors' refusal to present data resulted in the journals retracting the papers.21,23 Certainly, clinicians must rely on a thorough peer review process to screen out such flaws.
Multiple Responsibilities
Given the seriousness of the threat of this disease, the first priority of individuals in general is the protection of themselves, their families, their colleagues, and, frankly, everyone else. As everyone knows all too well by now, this means wearing protective masks and gloves, practicing "social distancing," and voluntary isolation. For many people, this has meant working, learning, or treating from home.
For those, such as clinicians, who must work with actual people and things (as opposed to "virtually"), isolation is not always an option, and protective measures must go further. Because they must come into close contact with many individuals every day, some of who may be patently ill patients, the risks for clinicians are obviously high. The recommendations made to dentists back in 2003 remain just as valid today: enforce universal infection control and standard precautions (wear protective glasses, gloves, gowns, and masks, and practice sterilization); take a careful health history, and use it; refer quickly and appropriately, erring on the side of caution; and stay out of harm's way.1 A further recommendation, testing, should be added to these if and when reliable tests are available, to rule out this very specific pathogen.
Of course, it is not always possible for clinicians to stay out of harm's way. Like nurses, police, firefighters, and the other "heroes" working gallantly throughout this pandemic, the job of clinicians often requires going into harm's way. Following the aforementioned recommendations and using the best equipment and techniques available can help clinicians do their job safely and successfully.
Hope Going Forward
The battle against COVID-19 appears to be far from over as evidence emerges of infections and deaths increasing precisely where and when public health measures, which admittedly are onerous, are relaxed. When society at large finally does emerge from self-isolation, it will be to a changed world. Familiar shops, restaurants, services, and especially people may not be there anymore. New ways of doing business will become familiar and entrenched. Some of these changes will be permanent, some will be transitory. People will have to adapt, and perhaps it will provide opportunities to improve.
Realistic hope of moving forward depends on having facts from sources that can be trusted. Thus far, amidst a virtually infinite supply of reporting and commentary, few peer-reviewed reports have been published on testing and treatment of COVID-19. Much of the knowledge that has been gained has come from press releases issued by WHO, NIH, and CDC-excellent sources, but scant data at this point. In any case, it is critical that trusted practitioners, such as hygienists, dentists, nurses, and physicians, stay thoroughly abreast of the best current information and share it with their patients in understandable language.
Not all of the news is bad. History is full of instances where alert clinicians have pointed the way to breakthroughs by sharing observations in as few as one interesting patient with their colleagues. Presently, there is a great need for thoughtful case reports to be published and shared. Although these may not carry the statistical and methodological weight of an RCCT, they warrant a respected place in the spectrum of "best evidence" at this juncture. A pattern of positive outcomes will likely be a harbinger of effective therapies to come.
Some research results offer realistic hope for effective antiviral drug treatments. Early studies in animals and humans suggest positive effects with one called remdesivir,24,25 and others will undoubtedly follow. Because COVID-19 is known to be a viral illness, it is prudent for clinicians to keep abreast of the literature to be able to recommend or use antiviral drugs in practice.
For dental clinicians, this crisis presents the opportunity to learn from it and to replace a host of bad, old habits. For the dental/medical community it may be an opportunity to reform creaky institutions and processes. Medical and dental professionals have learned a great deal about the power of cooperation, the unexpected importance of all sorts of occupations, and the value of stable, evidence-based leadership at all levels.
We have also learned just how vulnerable we are to natural factors beyond our control. And although it is impossible to be prepared for everything, it is obvious to most that our institutions were woefully unprepared for this pandemic and shamefully slow to respond. Science and technology were exceptions. Innovations like the Internet, rapid genetic sequencing, and rational drug design, just to name a few, contribute to our conviction that a victory over COVID-19 may not be too far away.
About the Authors
Marjorie Jeffcoat, DMD
Professor and Dean Emeritus, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
Thomas Sollecito, DMD
Professor, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania; Fellow of Dental Surgery, Royal College of Surgeons, Edinburgh
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
4. Centers for Disease Control and Prevention. Daily Updates of Totals by Week and State. Provisional Death Counts for Coronavirus Disease 2019 (COVID-19). Updated June 10, 2020. https://www.cdc.gov/nchs/nvss/vsrr/COVID19/. Accessed June 10, 2020.
5. Centers for Disease Control and Prevention. Coronavirus (COVID-19). https://www.cdc.gov/coronavirus/2019-ncov/. Accessed June 10, 2020.
6. World Health Organization. Coronavirus. https://www.who.int/health-topics/coronavirus. Accessed June 10, 2020.
7. Cochrane Consumer Network. Levels of evidence. https://consumers.cochrane.org/levels-evidence. Accessed June 10, 2020.
8. Jeffcoat M. Junk science: appearances can be deceiving. J Am Dent Assoc. 2003;134(7):802-806.
9. Muñoz M. Introduction to Post-marketing Drug Safety Surveillance: Pharmacovigilance in FDA/CDER. Washington, DC: US Food and Drug Administration; February 23, 2016. https://www.fda.gov/media/96408/download. Accessed June 10, 2020.
10. US Food and Drug Administration. "Off-Label" and Investigational Use Of Marketed Drugs, Biologics, and Medical Devices. Guidance for Institutional Review Boards and Clinical Investigators. January 1998. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/label-and-investigational-use-marketed-drugs-biologics-and-medical-devices. Accessed June 10, 2020.
11. National Institutes of Health. NIH to launch public-private partnership to speed COVID-19 vaccine and treatment options. April 17, 2020. https://www.nih.gov/news-events/news-releases/nih-launch-public-private-partnership-speed-covid-19-vaccine-treatment-options. Accessed June 10, 2020.
13. Centers for Disease Control and Prevention. Understanding How Vaccines Work. Atlanta, GA: Centers for Disease Control and Prevention; July 2018. https://www.cdc.gov/vaccines/hcp/conversations/downloads/vacsafe-understand-color-office.pdf. Accessed June 10, 2020.
14. Mair-Jenkins J, Saavedra-Campos M, Baillie JK, et al; Convalescent Plasma Study Group. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis. J Infect Dis. 2015;211(1):80-90.
15. National Institutes of Health. NIH mobilizes national innovation initiative for COVID-19 diagnostics. April 29, 2020. https://www.nih.gov/news-events/news-releases/nih-mobilizes-national-innovation-initiative-covid-19-diagnostics. Accessed June 10, 2020.
16. Watson J, Whiting PF, Brush JE. Interpreting a covid-19 test result. BMJ. 2020;369:m1808. doi: 10.1136/bmj.m1808.
17. Theel ES, Slev P, Wheeler S, et al. The role of antibody testing for SARS-CoV-2: Is there one? J Clin Microbiol. 2020;JCM.00797-20. doi: 10.1128/JCM.00797-20.
18. Sapkota D, Thapa SB, Hasseus, Jensen JL. Saliva testing for COVID-19? Br Dent J. 2020;228(9):658-659.
19. Riccò M, Ferraro P, Gualerzi G, et al. Point-of-care diagnostic tests for detecting SARS-CoV-2 antibodies: a systematic review and meta-analysis of real-world data. J Clin Med. 2020;9(5):1515. doi: 10.3390/jcm9051515.
20. Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. New Eng J Med. 2020;382(25):2411-2418.
21. Mehra MR, Desai SS, Kuy SR, et al. Retraction: cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med. DOI: 10.1056/NEJMoa2007621. N Engl J Med. 2020;382(26)2582.
22. Mehra MR, Desai SS, Ruschitzka F, Patel AN. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020; doi: 10.1016/S0140-6736(20)31180-6. Published online May 22.
23. Mehra MR, Ruschitzka F, Patel AN. Retraction-hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. Lancet. 2020;395(10240):1820. doi: 10.1016/S0140-6736(20)31324-6.
24. Williamson BN, Feldmann F, Schwarz B, et al. Clinical benefit of Remdesivir in rhesus macaques infected with SARS-CoV-2 [preprint]. New York: Cold Spring Harbor Laboratory; April 22, 2020. https://www.biorxiv.org/content/10.1101/2020.04.15.043166v2. Accessed June 10, 2020.
25. National Institutes of Health. NIH clinical trial shows Remdesivir accelerates recovery from advanced COVID-19. April 29,2020. https://www.nih.gov/news-events/news-releases/nih-clinical-trial-shows-remdesivir-accelerates-recovery-advanced-covid-19. Accessed June 10, 2020.