You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In the 1960s, Brånemark introduced the concept of osseointegration by demonstrating how a commercially pure titanium fixture was able to achieve bony anchorage through direct bone-to-implant contact.1 During the next 50 years, with advances in research, technology, and biomaterials, implant dentistry progressed to become a highly predictable treatment option for the replacement of missing teeth. Due, in part, to patients' increased demand for esthetics, Albrektsson's criteria for osseointegration have proven insufficient for the evaluation of implant treatment success.2-7 In order to account for the importance of patient satisfaction, Smith and Zarb extended Albrektsson's criteria to include adequate esthetic appearance as an additional requirement for success.8
For an implant restoration to be considered truly esthetic, it must resemble a natural tooth.9-11 Therefore, an understanding of the factors that comprise the natural esthetic zone is essential, and they should be evaluated prior to implant treatment planning.7,9,12 Implant treatment should begin with a prosthetic analysis to determine the ideal position, shape, and contours of the final restoration. This allows the clinician to evaluate the need for further interventions, such as orthodontic treatment or augmentation procedures, prior to implant placement.
The gingival scallop and interdental papilla are important determinants of an esthetic outcome.7,10,11 Because the reconstruction of deficient interdental papilla and gingival tissue can pose a challenge to clinicians, they are considered significant factors related to esthetic treatment risk.12,13 The esthetics of these structures are determined not only by the position of the implant but also by the shape and contour of the implant supported crown.7,11,12 For example, considering that the distance between the contact point and the alveolar crest is a determinant for papilla fill, the crown shape is ultimately responsible for the presence or absence of a papilla because it dictates the location of the contact point.7,11,12,14 Furthermore, the implant crown should provide a congruent position of the anatomical gingival zenith along with an appropriate emergence profile through the peri-implant mucosa, which is dependent upon the size and shape of the selected implant.4,15 In addition to helping preserve the gingival contours and improve interdisciplinary communication, implant-retained provisional restorations in the esthetic zone may be used to modify the pink esthetics following extraction and implant placement.16,17
In order to achieve an outcome with optimal esthetics and function, there is a general consensus that, regardless of the timing of implant placement, implants placed in the esthetic zone should abide by certain guidelines for 3-dimensional positioning, including the following10,16,18:
- Regarding the apicocoronal positioning of the implant, implants should be placed 3 mm to 4 mm apical to the expected position of the gingival margin.15
- Buccopalatally, the presence of a minimum of 2 mm of bone buccal to the implant is recommended in order to prevent loss of facial tissue as a result of bone remodeling, but 4 mm is preferred.19 Ideally, the implant should be placed 1-mm palatal to the point of emergence of the adjacent teeth.15
- Mesiodistally, the implant shoulder should be placed in a position that respects a 1.5-mm distance from adjacent teeth and a 3-mm distance from any adjacent implants.20,21
Abiding by these guidelines can help clinicians prevent periodontal and esthetic complications.10,16,18 However, within these guidelines, it is assumed that the implant will be centered mesiodistally within the available restorative space. Consequently, the emergence profile and gingival contour are dictated by the size and shape of the implant, implant abutment, and implant supported crown, rather than the mesiodistal position of the implant.
Whereas many of the previous studies addressing the relationship between implant placement and hard- and soft-tissue esthetics have focused on the buccolingual position of implants, the aim of this article is to provide evidence to support the mesiodistal placement of anterior implants with respect to the location of the gingival zenith.
The most apical portion of the gingival margin is referred to as the gingival zenith.22 For maxillary canines the location of the gingival zenith in reference to the tooth axis tends to be located coincidental with the vertical buccal midline; for lateral incisors, it deviates 0.4-mm distal to the midline; and for central incisors, it deviates 1-mm distal to the midline.23 Replacement of a central incisor with an implant centered mesiodistally would thus result in a 1-mm discrepancy in the gingival contour on the distal aspect of the incisor and under-contouring of the gingival margin on its mesial aspect.
Previous studies of bone level implants have associated emergence angles that are greater than 30° with a significant risk for peri-implantitis.24 A high implant emergence angle results in a crown contour with impaired access for hygiene, promoting plaque accumulation and the subsequent initiation and progression of peri-implant disease. In addition to the emergence angle of the prosthesis, the contour of the critical and subcritical zones of the crown will dictate soft-tissue morphology and health.9,10,25
Given the importance of these hard- and soft-tissue relationships, in order to achieve an optimal esthetic and functional outcome in the anterior maxilla, it is proposed that, mesiodistally, implants should be centered in line with the gingival zenith rather than centered within the available restorative space (Figure 1 through Figure 3).
Case Report
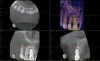
A 56-year-old female patient was referred for the evaluation of tooth No. 8 (Figure 4 and Figure 5). A periapical radiograph indicated that the tooth had undergone apicoectomy and received an excessively long post (Figure 6), and a cone-beam computed tomography (CBCT) scan of the site revealed a lack of buccal plate bone (Figure 7).
Esthetic implant placement was selected as the preferred treatment modality to restore function, preserve the smile, and provide a psychologic benefit. In addition to performing a complete periodontal evaluation, including periodontal probing, localization of the gingival margin, and calculation of the clinical attachment level, it was necessary to quantify the amount of keratinized tissue and gingival thickness for diagnosis and treatment planning. This patient was diagnosed with localized periodontitis (Stage II, Grade B) as well as other conditions affecting the periodontium, including an endodontic-periodontal lesion and gingival recession.26
Initial Augmentation and Implant Planning
Based on the single extraction socket roadmap developed by El Chaar and colleagues, the socket of tooth No. 8 was diagnosed as Grade III and would require initial treatment that included the extraction of failing tooth No. 8 followed by simultaneous guided bone regeneration and soft-tissue augmentation by means of a rotated palatal pedicle flap (Figure 8 through Figure 11).27,28 The principles of and guidelines for both the ridge augmentation and rotated pedicle flap have been described in the literature and will not be focused on in this case report.27-30 The patient was temporized with a bonded Maryland bridge that was adjusted to avoid creating pressure on the tissue during healing (Figure 12).
When the patient returned 4 months after the initial procedure for reevaluation, she underwent supportive periodontal therapy and was provided with detailed oral hygiene instructions (Figure 13). An intraoral scan and a postoperative CBCT scan were taken to evaluate both the horizontal and vertical hard- and soft-tissue gain. Next, implant planning software was used to merge the STL and DICOM data, which facilitated the creation of a digital wax-up (Figure 14).
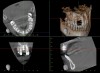
The digital wax up allowed the implant position to be planned based on the ideal prosthetic position of the final restoration (Figure 14). The planned implant position adhered to the aforementioned guidelines for ideal implant placement regarding the buccal, interproximal, and apical bone, and its platform would be located 4-mm apical to the planned restorative margin. In the coronal plane, the implant was centered with the gingival zenith in a position that was located approximately 1-mm distal to the midline of the edentulous space. Following implant planning, a tooth-supported surgical guide was designed and then 3D-printed to facilitate fully guided surgical implant placement.
Implant Surgical Procedure
Preoperatively, the patient was prescribed a 1-week course of antibiotics with instructions to begin taking them on the day of surgery. The patient was also prescribed an antimicrobial rinse with instructions to begin using it on the day after surgery. At the surgical appointment, perioral disinfection was accomplished utilizing a povidone-iodine solution. An antimicrobial soaked gauze was used to wipe intraorally, the teeth were debrided, and full mouth ultrasonic scaling was performed. Finally, profound local anesthesia was achieved by means of buccal and palatal infiltration.
Prior to the initiation of the surgery, the surgical guide was tried in to confirm proper seating and stability (Figure 15). A flapless approach was not considered because the need for further bone grafting at the time of implant placement had been anticipated through the digital planning. A slightly palatal crestal incision was made, followed by two vertical incisions on the mesial and distal aspects of the edentulous site in order to preserve the papilla and avoid additional esthetic compromise to the anterior sextant. Next, a full-thickness flap was elevated to facilitate removal of the tenting screw and permit visualization of the buccal plate (Figure 16). A standard guided protocol was followed to place the implant, and its final position mirrored that of the digital plan. As predicted, the prosthetically driven implant position resulted in an insufficient buccal plate (Figure 17); therefore, additional guided bone regeneration was performed to reinforce the area and prevent future breakdown (Figure 18 and Figure 19). Making periosteal incisions could have compromised the blood supply to the flap, so instead, it was stretched in order to achieve tension free coronal advancement.31The flap was secured utilizing horizontal mattress sutures with additional supportive interrupted sutures to ensure primary closure (Figure 20). An immediate postoperative periapical radiograph (Figure 21) and CBCT scan (Figure 22) were taken, demonstrating a final implant position centered with the planned location of the gingival zenith.
Temporization and Final Restoration
The patient was postoperatively evaluated at 1-, 2-, 4-, 8-, and 12-week recall appointments. The sutures were removed at the 2-week appointment, and the patient was instructed to rinse twice daily and avoid brushing the anterior maxilla. Prior to provisionalization of the implant, the site was allowed to heal for 6 months, during which time the patient was temporized with another Maryland bridge. At the 6-month recall appointment, full mouth periodontal maintenance was completed, and an implant-retained acrylic provisional restoration was placed (Figure 23 through Figure 25). An acrylic provisional restoration allows for soft-tissue attachment while preventing apical migration of the gingival margin. After a 3-month provisionalization period, the final prosthesis was delivered (Figure 26 through Figure 29), and the patient was scheduled for ongoing 3-month recall appointments for periodontal maintenance.
Conclusion
Traditionally, implant placement was dictated exclusively by bone quantity and quality. Today, however, the criteria for placement of a "successful" implant in the esthetic zone have evolved and encompass a multidisciplinary set of guidelines involving factors related to both hard and soft tissues, prosthetics, and patient expectations. Optimal esthetics and function are generated by a mesiodistal implant position centered on the gingival zenith. In the presented case report, the distal displacement of an implant used to replace a maxillary central incisor allowed for an abutment and prosthesis that more accurately replicated the emergence profile of a natural tooth, which improved the overall esthetics and peri-implant health by creating smoother buccolingual and mesiodistal contours.
About the Authors
Edgard El Chaar, DDS, MS
Director and Clinical Associate Professor
Advanced Education Program in Periodontics
New York University
College of Dentistry
New York, New York
Diplomate
American Board of Periodontology
Private Practice
New York, New York
Gretchen Stern, DDS
Periodontics Resident
New York University
College of Dentistry
New York, New York
Brett Weatherington, DDS
Periodontics Resident
New York University
College of Dentistry
New York, New York
References
1. Brånemark PI, Adell R, Breine U, et al. Intra-osseous anchorage of dental prostheses. I. Experimental studies. Scand J Plast Reconstr Surg. 1969;3(2):81-100.
2. Albrektsson T, Brånemark PI, Hansson HA, et al. Osseointegrated titanium implants. Requirements for enduring a long-lasting direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52(2):155-170.
3. Cosyn J, Thoma DS, Hämmerle CHF, et al. Esthetic assessments in implant dentistry: objective and subjective criteria for clinicians and patients. Periodontol 2000. 2017;73(1):193-202.
4. Buser D, Sennerby L, Bruyn HD. Modern implant dentistry based on osseointegration: 50 years of progress, current trends and open questions. Periodontol 2000. 2017;73(1):7-21.
5. Belser UC, Grütter L, Vailati F, et al. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: a cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J Periodontol. 2009;80(1):140-151.
6. Chappuis V, Araújo MG, Buser D. Clinical relevance of dimensional bone and soft tissue alterations post-extraction in esthetic sites. Periodontol 2000. 2017;73(1):73-83.
7. Kois JC, Kan JY. Predictable peri-implant gingival esthetics: surgical and prosthodontic rationales. Pract Proced Aesthet Dent. 2001;13(9):691-698.
8. Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62(5):567-572.
9. Kois JC. The restorative-periodontal interface: biological parameters. Periodontol 2000. 1996;11:29-38.
10. Chu SJ, Kan JY, Lee EA, et al. Restorative emergence profile for single-tooth implants in healthy periodontal patients: clinical guidelines and decision-making strategies. Int J Periodontics Restorative Dent. 2019;40(1):19-29.
11. Gobbato L, Paniz G, Mazzocco F, et al. Significance of crown shape in the replacement of a central incisor with a single implant-supported crown. Quintessence Int. 2013;44(5):407-413.
12. Kois JC. Predictable single tooth peri-implant esthetics: five diagnostic keys. Compend Contin Educ Dent. 2001;22(3):199-206.
13. Vailati F, Belser UC. Implant-supported fixed prostheses with integrated artificial gingiva for the esthetic zone: the pink power concept. Forum Implantologicum. 2011;7:108-123.
14. Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63(12):995-996.
15. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 Suppl:43-61.
16. Morton D, Chen ST, Martin WC, et al. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29 Suppl:216-220.
17. Noharet R, Van Dooren E. Combination of cone beam computed tomography and CAD-CAM techniques for maintaining natural emergence profile in immediate extraction and/or implant placement and restoration of a central incisor: A dental technique. J Prosthet Dent. 2019;122(3):193-197.
18. Chen S, Buser D. Esthetic complications due to implant malpositions: etiology, prevention, and treatment. In: Froum JT, ed. Dental implant complications etiology, prevention, and treatment. Hoboken, NJ: Wiley-Blackwell; 2010.
19. Spray RJ, Black CG, Morris HF, et al. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
20. Tarnow DP, Cho SC, Wallace SS. The effect of inter-implant distance on the height of inter-implant bone crest. J Periodontol. 2000;71(4):546-549.
21. Esposito M, Ekestubbe A, Grondahl K. Radiological evaluation of marginal bone loss at tooth surfaces facing single Brånemark implants. Clin Oral Implants Res. 1993;4(3):151-157.
22. Rufenacht C. Fundamentals of Esthetics. Chicago, IL: Quintessence Publishing; 1990:124-127.
23. Chu SJ, Tan JH, Stappert CF, et al. Gingival zenith positions and levels of the maxillary anterior dentition. J Esthet Restor Dent. 2009;21(2):113-120.
24. Katafuchi M, Weinstein BF, Leroux BG, et al. Restoration contour is a risk indicator for peri-implantitis: a cross-sectional radiographic analysis. J Clin Periodontol. 2018;45(2):225-232.
25. Steigmann M, Monje A, Chan HL, et al. Emergence profile design based on implant position in the esthetic zone. Int J Periodontics Restorative Dent. 2014;34(4):559-563.
26. Caton JG, Armitage G, Berglundh T, et al. A new classification scheme for periodontal and peri-implant disease and conditions - introduction and key changes form the 1999 classification. J Clin Periodontol. 2018;45 Suppl 20:S1-S8.
27. El Chaar E, Oshman S, Abed PF. Single-rooted extraction sockets: classification and treatment protocol. Compend Contin Educ Dent. 2016;37(8):537-542.
28. El Chaar E, Oshman S, Cicero G, et al. Soft tissue closure of grafted extraction sockets in the anterior maxilla: a modified palatal pedicle connective tissue flap technique. Int J Periodontics Restorative Dent. 2017;37(1):99-107.
29. Liu J, Kerns DG. Mechanisms of guided bone regeneration: a review. Open Dent J. 2014;8:56-65.
30. Khoury F, Happe A. The palatal subepithelial connective tissue flap method for soft tissue management to cover maxillary defects: a clinical report. Int J Oral Maxillofac Implants. 2000;15(3):415-418.
31. El Chaar E, Urtula B, Georgantza A, et al. Treatment of atrophic ridges with titanium mesh: a retrospective study using 100% mineralized allograft and comparing dental stone versus 3D-printed models. Int J Periodontics Restorative Dent. 2019;39(4):491-500.