You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
It has been reported that the highest frequency of oral trauma occurs in children between the ages of 8 and 10 years.1 At this age permanent teeth have erupted, but the roots have not matured; also, children still have most of their skeletal and facial growth yet to come. After loss of a tooth the ridge atrophies rather than develops. In addition, an ankylosed tooth leads to arrested development of the associated alveolar ridge.
To achieve the optimal prosthetic outcome, an intact alveolar ridge in the anterior esthetic zone is crucial. Bone grafting or augmentation procedures to correct a ridge defect, however, can be complicated and the outcomes unpredictable. Depending on the age at which an injury occurs, a trauma site may need to be managed for 10 years or more before a child's facial growth is complete. Incorporating the body's naturally occurring growth processes during that time may help mitigate the formation of a large ridge defect.
This article presents two treatment options to preserve the developing alveolar ridge. In one, fractured roots that were not ankylosed were retained; in the other, decoronation of an ankylosed tooth was performed.
Case 1: Not Ankylosed
A healthy 8-year-old boy was referred for evaluation and treatment of his maxillary right and left central incisors (teeth Nos. 8 and 9). His dental history revealed that 10 days earlier these two teeth had been severely luxated and both crowns fractured. Emergency treatment that day included placement of a splint and performance of a pulpotomy on tooth No. 9.
The patient's endodontic examination revealed a flexible splint from teeth Nos. 7 through 10 (Figure 1). Tooth No. 8 had a 3 mm x 3 mm class II fracture of the mesioincisal portion of the crown. Tooth No. 9 had a class IV fracture of the crown running labiopalatally from the remaining 2 mm of the crown to bone level on the palatal. A pulpotomy had been performed on the exposed pulp. Both teeth exhibited class III mobility. Teeth Nos. 7 through 10 did not respond to cold testing. None of the teeth were tender to palpation, and only tooth No. 9 had a slight positive response to percussion. Periodontal probings of tooth No. 8 were 4 mm to 5 mm on both the labial and palatal aspects. There was a narrow 12 mm probing on the straight palatal of No. 9; the remaining probing depths were 4 mm to 5 mm.2 A periapical radiograph showed both teeth Nos. 8 and 9 to have incompletely formed roots with wide-open foramina (Figure 2).
One month later, the splint was removed. Both teeth Nos. 8 and 9 exhibited mobility of one-half to one. There was no response to cold from teeth Nos. 8 through 10; No. 7 gave a positive response. Probings on both teeth Nos. 8 and 9 were 3 mm to 4 mm, and the straight palatal of No. 9 now probed 6 mm.
At 4 months, teeth Nos. 8 and 9 had slight mobility and neither tooth sounded ankylosed on percussion. Teeth Nos. 7 and 10 responded to cold; Nos. 8 and 9 did not respond. Both teeth probed 3 mm to 4 mm. A 7 mm x 6 mm periapical lesion had formed on tooth No. 9. There was no radiographic evidence of lengthening of the root or narrowing of the canal in No. 8. The patient's parents were informed that tooth No. 8 would likely need treatment. They opted to defer treatment until symptoms or signs arose. Apexification with calcium hydroxide (Ca(OH)2) on tooth No. 9 began 2 weeks later. Ca(OH)2 was replaced three times over the next year, during which time the lesion resolved. Tooth No. 9 was obturated with gutta-percha at about age 9.5. Shortly before obturation of No. 9, a sinus tract formed over tooth No. 8 and the referring dentist started apexification treatment with Ca(OH)2.
Two months after completion of the endodontic treatment of tooth No. 9, the patient presented with a chisel fracture about 2 mm apical to the cementoenamel junction (CEJ). The crown of tooth No. 9 was removed that day and Ca(OH)2 was replaced in tooth No. 8. Clinical photographs and radiographs were taken 3 months after removal of the coronal segment of No. 9 (Figure 3 and Figure 4). The missing crown of No. 9 was replaced with a temporary partial denture.
The Ca(OH)2 regimen for No. 8 continued for about a year when the patient, now age 11, presented with a horizontal fracture about 2.5 mm apical to the CEJ. No further endodontic treatment of No. 8 was attempted beyond the four previous Ca(OH)2 treatments. The coronal portion of No. 8 was retained for about 4 years before it was removed at age 15 (Figure 5 through Figure 7). Over that 4-year period, Ca(OH)2 in the canal was expended and not replaced.
After that the patient was seen in the endodontic office periodically to monitor the retained roots and associated alveolar ridge. The root of No. 8 was retained for 8 years after fracturing, and the root of No. 9 was retained for 9 years. During that time there were no clinical signs or symptoms, nor were there radiographic signs of periradicular breakdown. A final endodontic check at age 19 found the coronal surface of the root of No. 9 had been exposed. The vertical level and horizontal width of the alveolar ridge appeared very similar relative to the adjacent teeth as it had been at ages 10 and 15 (Figure 8 and Figure 9). No evidence of periradicular breakdown appeared radiographically (Figure 10). The patient's growth was deemed nearly completed and he was referred to an oral surgeon for evaluation and placement of implants.
At age 20, an oral surgeon placed implants in the Nos. 8 and 9 sites. A full-thickness flap was reflected and the roots were extracted. Both sockets were intact with thin-medium width labial plates (Figure 11). Implants were placed into the sockets, healing abutments were secured, and the flaps were sutured. Four months later the implants were uncovered and restorations were completed. (Author's note: A radiograph of the implants with healing abutments at placement was unavailable for this article.)
Case 2: Ankylosed
A healthy 9-year-old boy was referred for evaluation and treatment of his maxillary central incisors. He had been in a bicycle accident 2 weeks earlier. The right central incisor had been avulsed and the left central incisor had a class II fracture of the mesioincisal edge. Tooth No. 8 had been replanted after 90 minutes, and orthodontic brackets were placed to splint and position the tooth in anticipation of ankylosis.
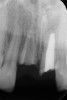
Teeth Nos. 7 through 10 were included in the endodontic examination. Nos. 7 and 10 responded to cold; there was no response to cold or electric pulp test (EPT) from either tooth No. 8 or 9. All the teeth gave a mild positive response to percussion, and none of the teeth were tender to palpation. Both Nos. 8 and 9 probed within normal limits (WNL). Radiographs showed a small apical radiolucency associated with No. 8 and a widened periodontal ligament (PDL) on the mesial and apical aspect of No. 9 (Figure 12). An access was made in No. 8, and the canal was debrided and filled with Ca(OH)2.
One month later, the teeth were reevaluated. Nos. 7 and 10 continued to respond to cold. No. 8 was not mobile and sounded ankylosed when percussed. No. 9 was slightly mobile and did not respond to cold or EPT. A 3 mm x 3 mm apical lesion had formed on No. 9. Ca(OH)2 was replaced in tooth No. 8, and No. 9 was opened, debrided, and filled with Ca(OH)2. Both teeth were filled with gutta-percha 6 months after the initial endodontic examination. At that time, tooth No. 8 showed early evidence of replacement resorption on the mesial of the root; No. 9 was slightly mobile and the PDL appeared intact (Figure 13).
The patient returned 4.5 years later, at age 14, for evaluation of his right central incisor. The tooth was now approximately 2.5 mm in infraocclusion (Figure 14). He was asymptomatic, with neither tooth No. 8 nor No. 9 tender to percussion or palpation. No. 9 had normal mobility and the PDL appeared intact radiographically. The radiograph showed No. 8 to have extensive replacement resorption of the root. Gutta-percha was exposed from the mesial CEJ around the apex and down the distal aspect of the root, leaving a sliver of coronal root about 4 mm in length attached to the distal CEJ (Figure 15).
Decoronation consultations were held with the periodontist, referring dentist, and orthodontist. The surgeon concluded gutta-percha removal could be predictably accomplished at the time of implant placement. A decision was made to replace the orthodontic brackets to realign the adjacent teeth before decoronation and as a method to hold a temporary pontic after completion of the surgery.
Six months later decoronation as described by Malmgren was done on the right central incisor.3 After the crown was removed, a mesiolabiodistal collar of resorbing root remained (Figure 16).
The patient was recalled 1 year later. Although orthodontic hardware hindered a thorough clinical evaluation of the surgical site, it looked generally unremarkable. Palpation of the mid-labial alveolar ridge over tooth No. 8, however, revealed a fingertip-sized convexity similar to an exostosis, which was interpreted as the resorbing root of No. 8 being replaced by bone. The recall radiograph, when compared to the immediate postsurgical radiograph, showed 2 mm to 3 mm of bone coronal to the remaining collar of resorbing root structure (Figure 17).
The patient was recalled 1 year later at age 16.5. Endodontic tests for No. 9 were WNL as was the radiographic appearance of the root and periradicular bone. The vertical level of the soft tissue in the decoronation site was slightly apical when compared to the level of the adjacent papilla and the labial tissue level of the adjacent teeth (Figure 18). The horizontal width of the most coronal portion of the soft tissue in the site was slightly narrower than the ridge of the adjacent teeth. The mid-root labial convexity remained (Figure 19). A radiograph of No. 8 showed the slivers of root had continued to resorb and the additional coronal bone was still intact at the previous level (Figure 20). A recall at age 18 showed the soft tissue and radiographic appearance of the decoronation site to be essentially unchanged. Smaller slivers of resorbing root still remained.
At age 19, the remnants of the root had been replaced by bone and the soft-tissue dimensions remained stable. The mid-labial convexity of the replacement bone remained intact. An implant evaluation was scheduled.
One concern arising from the implant examination was that the coronal width of the ridge might be too narrow for the positioning of an implant that would support an esthetic implant crown without an additional bone graft procedure. A CBCT scan was taken, which showed an ample coronal ridge as well as a relatively large fenestration in the apical third of the alveolus.
At age 21, it was determined that growth was substantially com--pleted (Figure 21). At the implant surgery, a mid-crestal incision was made with adjacent sulcular incisions. The labial flap was reflected revealing a very wide ridge at the coronal aspect. The mid-labial fenestration was evident along with exposed gutta-percha. A test drill was made and a radiograph was taken, which showed that the gutta-percha was removed during the site preparation. The fixture was placed and a 2 mm healing abutment secured (Figure 22). The bone was quite dense. The labial fenestration was grafted with particulate bone and primary closure was accomplished with 6-0 nylon sutures.
The patient healed well, and in 4 months the implant was uncovered with a simple punch uncovering technique. One month later, the restorative dentist placed a custom provisional restoration to begin molding the soft tissue. There was a small black space between the central incisors, partly due to the triangular shape of tooth No. 9 and slight papilla shrinkage on the mesial of No. 9. A small gingival composite was placed on the mesial of No. 9 to mimic the contour of the provisional crown. The tissue was molded for 4 months, and the final restoration was placed (Figure 23).
Discussion
The first case illustrates several aspects involved in the long-term clinical management of two injured, but not ankylosed, central incisors with immature root formation. The roots of both teeth subsequently fractured near the CEJ. The treatment goal was to sustain the development of the alveolar ridge until childhood growth was completed and implants could be placed.
According to clinical observations supported by investigational studies, retained teeth and roots preserve the associated alveolar ridge.4-7 These studies focused on alveolar ridge preservation in adult patients. With the advent of implants, ridge preservation became more significant as superior functional and esthetic prosthetic outcomes were becoming possible after tooth extraction. In children, however, this option was not available until growth was completed so as to avoid both potential esthetic issues due to continuing facial growth and infraocclusion of the implant in relation to adjacent natural teeth.
Between the restorative challenges posed by the treatment of fractured immature and mature permanent teeth, along with being unfamiliar with survival rates and lacking a strategic treatment plan, the instinctive response of clinicians may often be to remove these teeth. Yet, in contrast to removal of a fractured tooth, multiple studies have found the prognosis for fractured roots to be good. One study found 77% of fractured roots undergo repair.8 Non-repair caused by pulpal necrosis occurred in 13 cases, nine of which were successfully treated with endodontic treatment. Four teeth were removed. In a follow-up study of seven teeth with incomplete root formation, all the teeth retained pulp vitality and had repair of the fracture and nearly normal root development with closure of the apical foramen.9 Two of the teeth were re-fractured and healed spontaneously.
Another study of 22 root fractures included 10 patients who were under age 11. It found that pulp vitality could not be reliably detected for 1 year after the injury. Five teeth required endodontic treatment on the coronal segment, but none of the teeth became abscessed or formed a sinus tract over a range of 6 to 92 months.10
A success rate of 90% was found in a clinical investigation of fractures at or below the gingival margin in children. The children ranged in age from 8.3 to 15.8 years old. They were followed for 2 years. Because of the high success rate, retaining permanent anterior roots in children was deemed justified.11
In a large retrospective study, the survival rate of 534 root-fractured teeth was 80% in patients aged 7 to 17 years. Fifty-six teeth healed with root development being only one-third to two-thirds formed. The most frequent loss of a tooth occurred in 77 teeth with fractures in the coronal third of the root. Nevertheless, healing occurred in 30% of those 77 teeth, and the study advised to proceed conservatively rather than with immediate removal.12
Most of the teeth extracted in studies were fractured in the coronal third of the root.12-14 After the removal of the coronal segment, the remaining root segment may not be suitable for a restorative foundation. Nevertheless, clinical articles have demonstrated that the retained root segment of a fractured tooth appears to maintain the height and width of the alveolar ridge in the fracture site in a way similar to the adjacent developing ridge.11,15 With this in mind, the remaining root should be evaluated for its use in preserving a developing ridge before being removed.
The ideal outcome for root-fractured teeth would be for the pulp to remain vital and the root to repair to nearly its original state. If, however, a tooth cannot be restored to a functional state, retaining the remaining portion of the root may serve to sustain the development of the alveolar ridge, preventing resorption of the facial plate of the ridge until a child's skeletal growth is complete, thereby preserving a ridge that is as normal as possible for a future implant.
From age 8 to age 19, midfacial skeletal growth occurs. Without a tooth, the alveolar ridge does not fully develop vertically and the ridge loses about one-third of its labial width after the tooth is lost.16,17 In case 1, clinical photographs and radiographs were routinely obtained. When compared, photographs taken at different ages appear very similar in both the facial (Figure 5 and Figure 8) and occlusal views. The levels of the tissue in the edentulous area relative to the incisal edges of the lower anteriors were quite comparable, as were the levels of the papillae on either side of the site. The width of the alveolar ridge in the extraction sites looked much the same from occlusal views (Figure 4, Figure 6, and Figure 9).
Allowing for differences in radiographic angulation, the apices of the retained roots remained in a similar position relative to the apices of the adjacent teeth as did the coronal edges of the root relative to the CEJs of those teeth (Figure 3, Figure 7, and Figure 10). It appears that the retained roots preserved the developing ridge associated with them in a manner similar to the developing ridge next to the injury site during the child's 11 years of growth. The final result was an intact alveolar ridge with an adequate labial plate at the proper level for an implant (Figure 11).
The outcome of case 1 supports the observations and results of multiple investigational studies that routine extraction of fractured teeth is unwarranted. Further, the outcome indicates that the retention of the root of a fractured immature or mature tooth should be considered as an interim treatment in a long-term plan to preserve the anterior alveolar ridge through childhood growth.
The second case demonstrates excellent preservation of the anterior alveolar ridge after decoronation of an ankylosed tooth. However, several decoronation case reports have mixed or unsatisfactory results. Decoronation near the end of adolescent rapid growth in a few cases was performed after a large vertical alveolar ridge defect had already formed.18,19 In other cases, treatment was ongoing and the final state of the alveolar ridge at the time of implant surgery was not documented.20-23
The outcome of this patient's decoronation surgery was extraordinary. Figure 17 shows the deposition of bone 1 year after decoronation. Figure 22 shows the bone formed during replacement resorption of the remaining root. Both the quantity and location of bone after the procedure were exceptional. The coronal level of the replacement bone was proper for an implant fixture as was the horizontal width.
Determining the most appropriate time to decoronate an ankylosed tooth has been discussed in the literature.24-26 Decoronation should take place near the start of adolescent rapid growth when a tooth is approximately one-eighth to one-fourth of the crown height of an adjacent homologous tooth or about 2 mm to 3 mm in infraocclusion. Decoronation at that level of infraocclusion should mitigate the development of a severe alveolar ridge defect.
Predicting the labiopalatal width and vertical height of the ridge that will form relative to the ridge of the adjacent teeth after decoronation is more difficult. Malmgren et al's original article describing decoronation surgery found the alveolar bone moved coronally 0.2 mm to 1 mm in eight patients, remained the same in three patients, and moved apically 0.2 mm to 1.3 mm in three patients.3 Patients treated before age 13 showed no further infrapositioning of the ridge. A later report noted that in unpublished data of 103 decoronated ankylosed incisors bone level increased in patients treated before or during pubertal growth27; the amount of increase, however, was not reported.
In 2006, Malmgren et al presented a hypothetical biological explanation for the maintenance of crestal bone labiopalatal width and the continued development of the vertical height of crestal bone after decoronation of ankylosed teeth.28 The article proposed that the development of the vertical height is related to skeletal jaw growth and tooth eruption. In the present case 2, a comparison of the root apices of teeth Nos. 7 and 8 at ages 9.5 and 14.5 years shows the amount of coronal ridge growth/eruption of No. 7 that occurred relative to ankylosed No. 8 beforedecoronation(Figure 13 and Figure 16). One year after decoronation, the apices of teeth Nos. 7 and 9 did not appear to have moved coronally relative to their location before surgery (Figure 16 and Figure 17).
The median age for rapid growth in boys is between 12.5 and 15 years.29 Hypothetically, by decoronating tooth No. 8 at age 14.5, most of the potential coronal movement of adjacent teeth that leads to bone deposition during rapid adolescent growth would have already occurred. Yet, an ample amount of coronal bone was deposited. Despite this bone deposition, lack of coronal movement was demonstrated by the absence of change in the location of the apices of the adjacent teeth relative to the decoronated tooth after surgery. While the outcome for this patient was exceptional, predictability of such outcomes is unknown at this time.
Conclusion
This article highlighted two long-term cases with the same goal of preserving the anterior alveolar ridge in a child after trauma. Two different approaches were needed and taken to incorporate naturally occurring growth processes. The treatment plans were dependent upon whether or not the teeth were ankylosed; both treatments resulted in excellent outcomes.
Additional case series and reports of decoronation treatment near the start of adolescent rapid facial growth, when an ankylosed tooth is 2 mm to 3 mm in infraocclusion, accompanied by photographs and limited field-of-view CBCT radiographs to document the state of the alveolar ridge when an implant is placed, might help clinicians better predict expected horizontal width and vertical level of ridge preservation.
Acknowledgment
The authors thank Gerald W. Harrington, DDS, MSD, Professor Emeritus, Department of Endodontics, School of Dentistry, University of Washington, for his help in preparing this article.
About the Authors
David R. Steiner, DDS, MSD
Affiliate Professor, Graduate Endodontics Program, Department of Endodontics, School of Dentistry, University of Washington, Seattle, Washington
David P. Mathews, DDS
Affiliate Professor, Graduate Periodontics Program, Department of Periodontics, School of Dentistry, University of Washington, Seattle, Washington
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Andreasen JO, Andreasen FM, eds. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 3rd ed. Copenhagen, Denmark: Munksgaard, Mosby; 1994.
2. Harrington GW. The perio-endo question: differential diagnosis. Dent Clin North Am. 1979;23(4):673-690.
3. Malmgren B, Cvek M, Lundberg M, Frykholm A. Surgical treatment of ankylosed and infrapositioned reimplanted incisors in adolescents. Scand J Dent Res. 1984;92(5):391-399.
4. Lam RV. Contour changes of the alveolar processes following extractions. J Prosthet Dent. 1960;10(1):25-32.
5. Helsham RW. Some observations on the subject of roots of teeth retained in the jaws as a result of incomplete exodontia. Aust Dent J. 1960;5(2):70-77.
6. O'Neal RB, Ground T, Levin MP, del Rio CE. Submergence of roots for alveolar bone preservation. I. Endodontically treated roots. Oral Surg Oral Med Oral Pathol. 1978;45(5):803-810.
7. Casey DM, Lauciello FR. A review of the submerged-root concept. J Prosthet Dent. 1980;43(2):128-132.
8. Zachrisson BU, Jacobsen I. Long-term prognosis of 66 permanent anterior teeth with root fracture. Scand J Dent Res. 1975;83(6):345-354.
9. Jacobsen I. Root fractures in permanent anterior teeth with incomplete root formation. Scand J Dent Res. 1976;84(4):210-217.
10. Yates JA. Root fractures in permanent teeth: a clinical review. Int Endod J. 1992;25(3):150-157.
11. Rodd HD, Davidson LE, Livesey S, Cooke ME. Survival of intentionally retained permanent incisor roots following crown root fractures in children. Dent Traumatol. 2002;18(2):92-97.
12. Cvek M, Tsilingaridis G, Andeasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years. Dent Traumatol. 2008;24(4):379-387.
13. Cvek M, Mejàre I, Andreasen, JO. Healing and prognosis of teeth with intra-alveolar fractures involving the cervical part of the root. Dent Traumatol. 2002;18(2):57-65.
14. Cvek M, Mejàre I, Andreasen JO. Conservative endodontic treatment of teeth fractured in the middle or apical part of the root. Dent Traumatol. 2004;20(5):261-269.
15. Mackie IC, Quayle AA. Implants in children: a case report. Endod Dent Traumatol. 1993;9(3):124-126.
16. Iasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and a collagen membrane compared to extraction alone for implant site development: a clinical and histologic study in humans. J Periodontol. 2003;74(7):990-999.
17. Avila-Ortiz G, Elangovan S, Kramer KW, et al. Effect of alveolar ridge preservation after tooth extraction: a systematic review a and meta-analysis. J Dent Res. 2014;93(10):950-958.
18. Cohenca N, Stabholz A. Decoronation - a conservative method to treat ankylosed teeth for preservation of alveolar ridge prior to permanent prosthetic reconstruction: literature review and case presentation. Dent Traumatol. 2007;23(2):87-94.
19. Schwartz-Arad D, Levin L, Ashkenazi M. Treatment options of untreatable traumatized anterior maxillary teeth for future use of dental implantation. Implant Dent. 2004;13(2):120-128.
20. Diaz JA, Sandoval HP, Pineda PI, Junod PA. Conservative treatment of an ankylosed tooth after delayed replantation: a case report. Dent Traumatol. 2007;23(5):313-317.
21. Filippi A, Pohl Y, von Arx T. Decoronation of an ankylosed tooth for preservation of alveolar bone prior to implant placement. Dent Traumatol. 2001;17(2):93-95.
22. Sapir S, Kalter A, Sapir MR. Decoronation of an ankylosed permanent incisor: alveolar ridge preservation and rehabilitation by an implant supported porcelain crown. Dent Traumatol. 2009;25(3):346-349.
23. Sigurdsson A. Decoronation as an approach to treat ankylosis in growing children. Pediatr Dent. 2009;31(2):123-128.
24. Steiner DR. Timing of extraction of ankylosed teeth to maximize ridge development. J Endod. 1997;23(4):242-245.
25. Malmgren B, Malmgren O. Rate of infraposition of reimplanted ankylosed incisors related to age and growth in children and adolescents. Dent Traumatol. 2002;18(1):28-36.
26. Steiner DR. Avulsed maxillary central incisors: the case for replantation. Am J Orthod Dentofacial Orthop. 2012;142(1):8-16.
27. Malmgren B. Ridge preservation/decoronation. Pediatr Dent. 2013;
35(2):164-169.
28. Malmgren B, Malmgren O, Andreasen JO. Alveolar bone development after decoronation of ankylosed teeth. Endod Topics. 2006;14
(1):35-40.
29. Tanner JM. Growth at Adolescence. 2nd ed. Springfield, IL: Blackwell Scientific Publications Ltd; 1962.