You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
As described previously by the authors, the concept of 10 keys for successful esthetic-zone single immediate implants is an evidenced-based approach to treatment plan and immediately replace a hopeless tooth with a dental implant in the maxillary anterior sextant.1 The 10 keys comprise two treatment-planning, five surgical, and three prosthetic keys. The goal is to minimize soft- and hard-tissue complications to attain an optimal long-term esthetic implant restoration.
As has been discussed in the literature, immediate implant placement in the esthetic zone requires the clinician to be knowledgeable and experienced in a variety of areas. These include esthetic diagnosis, minimally invasive extraction techniques, oral plastic surgical procedures (eg, hard- and soft-tissue grafting, "gummy smile" correction/crown lengthening), and accurate 3-dimensional (3D) implant placement/restoratively driven planning and placement based on cone-beam computed tomography (CBCT) analysis.1-4 Tissue-contour management requires prosthetic knowledge of provisionalization techniques to sculpt peri-implant tissue for developing submergence contour from the implant shoulder to the mucosal zenith to adequately support the tissue. Final impression techniques must capture and transfer this submergence contour, or "transitional zone," to be duplicated in the final crown.1 Under these guidelines the surgical and restorative treatment in the esthetic zone is considered a "complex SAC" procedure, according to the straightforward (S), advanced (A), complex (C) (SAC) classification system.5
In a 2009 systematic review, Chen et al suggested potential risk of facial gingival recession of up to 30% of all cases.4 They identified pre-existing defects of the facial bone, thin facial bone, thin soft-tissue biotype, and facial malposition of the implantas potential risk factors for gingival recession following immediate single-tooth implant placement. Recent systematic reviews by Levine et al2 and Chen et al4 and consensus statements by Morton et al6 were written to organize the diagnosis, planning, and treatment of single-tooth implants in the esthetic zone, along with the treatment of complications around them. Their conclusions suggested a team protocol, if strictly followed, would provide high predictability in preventing esthetic complications related to single-tooth implants. Several guidelines were proposed to ensure high success rates.6 Ten keys were developed to aid the team in treatment planning for a successful esthetic restoration.1
10 Keys for Success
These 10 keys for successful esthetic-zone single immediate implants are defined as follows1:
1. Esthetic risk assessment. This assessment is reviewed with each patient and restorative team member to determine the specific esthetic risk criteria for immediate placement in the esthetic zone.
2. Tomographic plan: CBCT and restorative-driven treatment plan. This is doneto assess for adequate buccal bony wall thickness and to determine the sagittal root position of the tooth, alveolar form, and planned implant position.
3. Minimally traumatic tooth extraction, without flap reflection (if possible), with evaluation of buccal plate status. If the buccal plate is intact, the clinician may proceed with the procedure. If the buccal plate is not intact, the risk of postoperative recession is significantly increased. Either ridge preservation or delayed implant placement might then be recommended.
4. 3D implant placement in good available bone both apically and palatally along the palatal wall. This helps assure a, preferably, screw-retained position for the provisional and final restorations. Ideally, an anatomically correct surgical guide template should be used.
5. Use of a narrower (3.3 mm to 4.3 mm) implant versus a wider-diameter (4.5 mm or greater) implant. This ensures at least a 2-mm to 3-mm buccal gap adjacent to the intact buccal socket wall. This can be preplanned with a careful CBCT analysis and an understanding of the restorative-driven plan.
6. Bone grafting of the buccal gap with a low-substitution small-particle mineralized bone material. Deproteinated bovine bone mineral (DBBM) or freeze-dried bone allograft (FDBA) may be used.
7. Facial gingival grafting using a palatal subepithelial connective tissue graft (SCTG) placed in a buccal envelope under the buccal marginal tissue and facial to the intact buccal plate. This is done to augment the existing gingiva such that it is thick enough for biotype conversion. (The authors note that the dual-zone grafting technique7 also can be used to achieve similar soft-tissue thickness but prefer the present technique, which they have been performing for more than 25 years with cross-sectional CT/CBCT follow-up.)
8. Immediate contour management of the emergence profile from the implant. This is to preserve the soft-tissue and transition-zone contoursusing an anatomically correct or slightly under-contoured emergence profile with either a screw-retained immediate provisional restoration or a healing abutment that may be customized.
9. Once the team is satisfied with the soft-tissue esthetics developed in the provisional stage, a custom impression coping technique is usedto duplicate the transition zone, which is replicated in the final impression and transferred to the lab model.
10. Final restoration with a screw-retained crown. If direct screw retention is not possible, stock abutments should be avoided because of the difficulty of removing excess cement from deep interproximal margins. An anatomically contoured custom abutment with a titanium implant interface should be fabricated with the final facial cement line no deeper than 1 mm circumferentially. If cemented restorations are needed, radiopaque non-resin cements, using a minimum cement load (ie, copy abutment technique), should be utilized.
Use of a Palatal SCTG
The purpose of this article is tosuggest the routine use of a palatal SCTG placed into a buccal envelope facial to the intact buccal plate based on scientific evidence (as noted in the section below) that strongly supports this approach. Specifically, key No. 7, involving use of a palatal SCTG, is essential when completing immediate single-tooth replacement in the esthetic zone to aid in a long-term successful esthetic outcome. The following case will describe the 10 keys in the treatment of a failed maxillary central incisor with a 5-year follow-up (Figure 1 through Figure 13).
The patient, a healthy 45-year-old nonsmoking woman (American Society of Anesthesiologists [ASA] II), presented with a failed maxillary central incisor due to severe internal-external root resorption (Figure 1). She had a high esthetic risk profile based on 12 presenting esthetic risk factors (key No. 1), including a high lip line, high esthetic expectations, and adjacent teeth that had been restored (Figure 2).Site-specific CBCT (Carestream CS 9300, Carestream Dental, carestream.com) noted a thick intact buccal plate and a class 1 sagittal root position (Figure 3 and Figure 4). Preplanning with a bone-level 4.1-mm diameter x 14-mm long implant (Straumann Bone Level Roxolid® SLActive, Straumann, straumann.com) assured a 3-mm buccal gap upon placement and a screw-retained position (key No. 2). Prior to placement, intact buccal and palatal walls were confirmed. Figure 5 shows palatal wall placement of the implant after minimally traumatic flapless tooth extraction. An anatomically correct surgical guide template was used to assure a screw-retained position and correct vertical depth of approximately 4 mm from the mid-buccal apical extent of the guide template, which correlated to 1 mm apical of the intact buccal plate (key Nos. 3 through 5). The two-unit (8-9x cantilever) fixed provisional was recemented post-surgery. The 3-mm buccal gap was grafted tightly with a low-substitution DBBM (Bio-Oss®, Geistlich Pharma, geistlich-na.com) (key No. 6), and a pouch was created with a Buser membrane instrument (Hu-Friedy, hu-friedy.com) from line angle to line angle as a mini full-thickness flap to the mucogingival border to accept a connective tissue graft (Figure 6). The connective tissue graft, 1-mm thick x 12-mm long x 7-mm wide (Figure 7), was harvested from the palate (key No. 7).
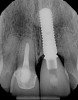
Figure 8 shows the provisionalization of No. 8 at 6 weeks postoperatively and a screw-retained provisional restoration on No. 9 to develop the subgingival transitional zone (key Nos. 8 through 10). The transitional zone will be duplicated using the custom impression coping technique. Figure 9 and Figure 10 depict the completed crowns at 5 years; implant No. 9 was screw-retained (key No. 10). In Figure 10 note the convex contours facial to implant No. 9 that are attributed to the connective tissue grafting as part of the surgical protocol creating biotype conversion from a thick to a thicker biotype. Figure 11 through Figure 13 show 5-year postoperative patient smile, periapical x-ray, and CBCT, respectively.
Evidence for Routine Use of Key No. 7
Kan et al in their immediate implant placement and provisionalization (IIPP) study of the esthetic zone (no bone grafting of the buccal gap or SCTG) reported significantly greater facial gingival level (FGL) changes in the thin gingival biotype group (-1.5 mm) compared to the thick gingival biotype group (0.56 mm).8 Facial gingival recession is normally a common occurrence after immediate tooth replacement and ranges from -0.5 mm to -0.8 mm.9-11 When bone graft material was placed in the buccal gap and a SCTG was added facial to the buccal bone during IIPP, Kan et al observed no significant difference in the FGL change (mean follow-up of 2.15 years) between thick (eight patients) and thin (12 patients) gingival biotype.12 This may suggest that a thin gingival biotype can be converted to a thicker gingival biotype morphologically and behaviorally. Thus, the term "biotype conversion" was coined.8 In addition, Cook et al found a difference in labial plate thickness when comparing thin and thick biotypes.13
In a 1-year prospective study in non-esthetic sites in humans, Linkevicius et al found the initial gingival thickness at the alveolar crest may influence marginal bone stability around implants.14 If the tissue thickness was ≤2.5 mm, crestal bone loss of up to 1.45 mm occurred within the first year of function despite a supracrestal position of the implant-abutment interface. They also recommended thickening of thin mucosa before implant placement, converting a thin tissue biotype into a thicker one. This is consistent with an animal study by Berglundh et al,15 who reported the correlation of thin tissues with crestal bone loss during biologic width formation if a minimum dimension of the biologic width was not pre-existing.
Linkevicius et al also found that platform switching in a one-stage implant placement approach does not prevent crestal bone loss if, at the time of implant placement, mucosal tissue is thin (≤2 mm).16However, in thick soft tissue (>2 mm), use of a platform-switched implant maintained crestal bone level with minimal remodeling at 1 year.
Puisys et al in a two-stage implant placement approach with a platform switch found similar results.17 Thin tissues (≤2 mm) lost significant crestal bone, whereas thick tissues (>2 mm) or thin tissues augmented with acellular dermal matrix had similar crestal bone maintenance with minimal bone loss at 1 year.
The positive use of a SCTG technique in conjunction with bone grafting the implant-socket gap with IIPP in the esthetic zone and 3D placement has been evaluated in several other case studies.18-23Rungcharassaeng et al studied the facial gingival tissue thickness (FGTT) with IIPP on maxillary anterior teeth with the placement of SCTGs (n = 31) and without SCTGs (n = 24).22 Using spectrophotometric analysis, Jung et al, in a pig jaw model, evaluated gingival discoloration with three different gingival thicknesses (1.5 mm, 2 mm, and 3 mm) over four different restorative materials (titanium, titanium-ceramic, zirconia-ceramic, and zirconia). The results showed 2 mm of gingival thickness was needed to mask the titanium group, and with 3 mm of gingival thickness all four test materials were sufficiently masked.24
In the Rungcharassaeng study, patients who did not receive the SCTG had a FGTT mean measurement of 1.42 mm.22 This seemed inadequate to mask any type of underlying restorative material, as was also noted in the Jung et al study.24 The mean for the SCTG cases was 2.61 mm, which was significantly greater. Rungcharassaeng et al concluded that when performing IIPP in conjunction with a connective tissue graft, sufficient peri-implant tissue thickness to conceal the underlying implant restorative materials is more likely to result, compared to non-grafted sites.22
Cosyn et al evaluated immediate screw-retained restorations in 22 patients who presented with thick gingival biotypes (thin biotype was excluded).11 All implants were placed by experienced surgeons using platform-switched implants, and all buccal gaps were grafted with DBBM. At 3 months, five cases demonstrated alveolar process remodeling with facial gingival recession (≥1 mm) and were grafted with a SCTG using the pouch technique. Additionally, two cases showed advanced mid-facial gingival recession (1.5 mm to 2 mm) and were also grafted with a SCTG. Thus, seven cases (31.8% of cases) were grafted at 3 months because of esthetic complications. SCTG use resulted in a steady improvement of the pink esthetic score (PES) after 3 months. The authors found similar PES post-treatment (PES: 11.86) compared to pre-surgery (PES: 12.15). They concluded that preservation of pink esthetics is possible following immediate tooth replacement. However, to achieve this, a SCTG is necessary in about one-third of the patients (who present with a thick gingival biotype). Similarly, in the study by Chen et al, mid-facial recession of 1 mm to 3 mm was noted in 10 of 30 sites (33%) within the first year.9
When the Cosyn study was followed up to 5 years their results were surprising.25 The sites previously treated with SCTG improved and all remained stable at the 5-year evaluation. However, three additional sites (all maxillary central incisors) that were stable and considered esthetic at 1 year (having received no SCTG) experienced significant facial recession (>1 mm) after 1 year and required a SCTG. At 5 years, of the returning 17 patients of the original 22 that presented at the start of the study, more than 50% (10/17) were treated with SCTGs by the 5-year mark. Thus, mid-facial recession (>1 mm) as noted in the 5-year Cosyn et al study,25 in which the authors used nine of the 10 aforementioned keys (excluding SCTG) as part of their protocol, may be seen in as few as 30% of esthetic-zone cases at 1 year but in as many as 50% by 5 years.
Based on their results, Cosyn et al concluded that though single immediate implants showed high implant survival and limited marginal bone loss in the long term, mid-facial recession, mid-facial contour, and alveolar process deficiency deteriorated after 1 year, and that with an esthetic complication rate of 8 out of 17 in well-selected patients who had been treated by experienced clinicians, type 1 placement (ie, immediate) could not be recommended for daily practice.25Their conclusion is interesting in that there was no suggestion of the routine usage of a SCTG as part of the initial surgical protocol to help prevent the mid-facial recession seen at both 1 year and 5 years in thick-tissue biotype patients. The Cosyn et al protocol used all of the 10 keys mentioned herein except key No. 7 and used a SCTG only after significant mid-facial recession had occurred.
Esthetic Complications Without Use of SCTG
Thus, based on the literature it seems that when clinicians do not use a SCTG in the esthetic zone when treating the thick-tissue biotype patient they get "lucky" approximately 50% to 70% of the time and"unlucky" 30% to 50% of the time. For example, Figure 14 and Figure 15 show an 11-year follow-up of a case treated in 2006. The patient was a 65-year-old healthy nonsmoking woman who had a low esthetic risk profile with a thick periodontal biotype. She had thick intact buccal crest after flapless surgical extraction, immediate 3D implant placement (Straumann Tissue Level Tapered Effect Regular Neck SLActive implant, Straumann), buccal gap bone grafting with a low-substitution DBBM (Bio-Oss), and an immediate screw-retained provisional restoration (Figure 14). Nine of the 10 keys were used, the exception being key No. 7 (SCTG), and it seems "luck" played a part in the result as no mid-buccal recession/esthetic complication was noted.
An example of an "unlucky" outcome is shown in Figure 16, which depicts a 15-year postoperative result of the No. 7 implant in a 44-year-old female patient with a high esthetic risk profile. Again, all 10 keys except key No. 7 (SCTG) were followed. Esthetic complication of >1 mm mid-buccal recession with a facial bony concavity was noted. The treatment included removal of the custom abutment and remaking the crown on a UCLA abutment.
Finally, another example of an "unlucky" esthetic outcomeis illustrated in Figure 17 through Figure 19, which show the 3-year postoperative follow-up of the fully guided (coDiagnostix®, Dental Wings, dentalwings.com) 3D placement of No. 7 and No. 10 implants (Straumann Bone Level Narrow Connection Roxolid® SLActive, Straumann) in a 34-year-old high esthetic risk profile female patient with non-loading of both implant sites. For this patient, eight of the 10 keys were followed, with the exceptions being key Nos. 7 (SCTG) and 8 (immediate contour management). Esthetic complication was noted, especially on implant No. 7, with a facial bony concavity with loss of ridge width and show-through of the titanium custom abutments (ie, "graying" of soft tissues) due to colorimetric changes of the marginal tissues.
Because clinicians cannot reliably predict which thick-tissue biotype cases will have significant mid-facial recession over time, the authors recommend that the routine use of a SCTG (key No. 7) be considered in all tissue biotypes for "biotype conversion" to gain a tissue thickness of at least 2 mm to 3 mm. This is corroborated with a recent randomized controlled trial by Zuiderveld et al in which SCTG was the only predictable variable in mid-buccal tissue stability regardless of tissue type.26Beyond soft-tissue augmentation, diligently following all the remaining 10 keys in total will help prevent esthetic mid-facial recession complications.
Conclusions
The 10 keys for esthetic-zone success for single immediate implants are meant to provide guidance for experienced clinicians and aid them in the treatment planning and execution of these cases. By following these steps closely, clinicians can reduce the chances of an unesthetic result.
Treatment in the esthetic zone is a complex SAC procedure for both the surgical phase (key Nos. 3 through 7) and prosthetic phase (key Nos. 8 through 10); therefore, it is important to consider the team approach when treatment planning in the esthetic zone. Even under ideal conditions (ie, thick periodontal biotype, experienced surgeon, intact buccal plate with bone grafting of the buccal gap, immediate 3D implant placement, and immediate contour management), there is a 30% risk at 1 year and a 50% risk at 5 years of significant facial gingival recession of >1 mm when a SCTG is not included in the initial surgical protocol. This concept of "periodontal biotype conversion" using a SCTG is a crucial consideration that may improve the chances of obtaining a long-term esthetic result.
About the Authors
Robert A. Levine, DDS
Clinical Professor, Periodontology and Implantology, Kornberg School of Dentistry, TempleUniversity, Philadelphia, Pennsylvania; Diplomate, American Board of Periodontology; Private Practice in dental implants and periodontics, Philadelphia, Pennsylvania
Jeffrey Ganeles, DMD
Adjunct Associate Professor, Nova Southeastern University College of Dental Medicine, Ft. Lauderdale, Florida; Diplomate, American Board of Periodontology; Private Practice in dental implants and periodontics, Boca Raton, Florida
Joseph Kan, DDS, MS
Professor, Loma Linda University School of Dentistry, Loma Linda, California; Private Practice in prosthodontics and implant dentistry, Covina, California
Phil L. Fava, DMD
Diplomate, American Board of Periodontology; Private Practice in dental implants and periodontics, Philadelphia, Pennsylvania
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Levine RA, Ganeles, J, Gonzaga L, et al. 10 keys for successful esthetic-zone single immediate implants. Compend Contin Educ Dent. 2017;38 (4):248-260.
2. Levine RA, Huynh-Ba G, Cochran DL. Soft tissue augmentation procedures for mucogingival defects in esthetic sites. Int J Oral Maxillofac Implants. 2014;29 suppl:155-185.
3. Morton D, Ganeles J, eds. ITI Treatment Guide Vol. 2. Loading Protocols in Implant Dentistry - Partially Dentate Patients. Berlin: Quintessence Publishing; 2007.
4. Chen S, Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla-a systematic review. Int J Oral Maxillofac Implants. 2014;29 suppl:186-215.
5. Dawson A, Chen S. The SAC Classification in Implant Dentistry. Berlin: Quintessence Publishing; 2009.
6. Morton D, Chen ST, Martin WC, et al. Consensus statements and recommended clinical procedures regarding optimizing esthetic outcomes in implant dentistry. Int J Oral Maxillofac Implants. 2014;29 suppl:216-220.
7. Chu SJ, Salama MA, Salama H, et al. The dual-zone therapeutic concept of managing immediate implant placement and provisional restoration in anterior extraction sockets. Compend Contin Educ Dent. 2012;33(7):524-534.
8. Kan JY, Rungcharassaeng K, Lozada JL, Zimmerman G. Facial gingival tissue stability following immediate placement and provisionalization of maxillary anterior single implants: a 2- to 8-year follow-up. Int J Oral Maxillofac Implants. 2011;26(1):179-187.
9. Chen ST, Darby IB, Reynolds EC. A prospective clinical study of non-submerged immediate implants: clinical outcomes and esthetic results. Clin Oral Implants Res. 2007;18(5):552-562.
10. De Rouck T, Collys K, Cosyn J. Immediate single-tooth implants in the anterior maxilla: a 1-year case cohort study on hard and soft tissue response. J Clin Periodontol. 2008;35(7):649-657.
11. Cosyn J, De Bruyn H, Cleymaet R. Soft tissue preservation and pink aesthetics around single immediate implant restorations: a 1-year prospective study. Clin Implant Dent Relat Res. 2013;15(6):847-857.
12. Kan JY, Rungcharassaeng K, Morimoto T, Lozada J. Facial gingival stability after connective tissue graft with single immediate tooth replacement in the esthetic zone: consecutive case reports. J Oral Maxillfac Surg. 2009;67(11 suppl):40-48.
13. Cook DR, Mealey BL, Verrett RG, et al. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent. 2011;31(4):345-354.
14. Linkevicius T, Apse P, Grybauskas S, Puisys A. The influence of soft tissue thickness on crestal bone changes around dental implants: a 1-year prospective controlled clinical trial. Int J Oral Maxillofac Implants. 2009;24(4):712-719.
15. Berglundh T, Abrahamsson I, Welander M, et al. Morphogenesis of the peri-implant mucosa: an experimental study in dogs. Clin Oral Implants Res. 2007;18(1):1-8.
16. Linkevicius T, Puisys A, Steigmann M, et al. Influence of vertical soft tissue thickness on crestal bone changes around implants with platform switching: a comparative clinical study. Clin Implant Dent Relat Res. 2015;17(6):1228-1236.
17. Puisys A, Vindasiute E, Linkevciene L, Linkevicius T. The use of acellular dermal matrix membrane for vertical soft tissue augmentation during submerged implant placement: a case series. Clin Oral Implants Res. 2015;26(4):465-470.
18. Yoshino S, Kan JY, Rungcharassaeng K, et al. Effects of connective tissue grafting on the facial gingival level following single immediate implant placement and provisionalization in the esthetic zone: a 1-year randomized controlled prospective study. Int J Oral Maxillofac Implants. 2014;29(2):432-440.
19. Redemagni M, Cremonesi S, Garlini G, Maiorna C. Soft tissue stability with immediate implants and concave abutments. Eur J Esthet Dent. 2009;4(4):328-337.
20. Chung S, Rungcharassaeng K, Kan JY, et al. Immediate single tooth replacement with subepithelial connective tissue graft using platform switching implants: a case series. J Oral Implantol. 2011;37(5):559-569.
21. Tsuda H, Rungcharassaeng K, Kan JY, et al. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011;26(2):427-436.
22. Rungcharassaeng K, Kan JY, Yoshino S, et al. Immediate implant placement and provisionalization with and without a connective tissue graft: an analysis of facial gingival tissue thickness. Int J Periodontics Restorative Dent. 2012;32(6):657-663.
23. Grunder U. Crestal ridge width changes when placing implants at the time of tooth extraction with and without soft tissue augmentation after a healing period of 6 months: report of 24 consecutive cases. Int J Periodontics Restorative Dent. 2011;31(1):9-17.
24. Jung RE, Sailer I, Hämmerle CH, et al. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27(3):251-257.
25. Cosyn J, Eghbali A, Hermans A, et al. A 5-year prospective study on single immediate implants in the aesthetic zone. J Clin Periodontol. 2016;43(8):702-709.
26. Zuiderveld EG, Meijer HJA, den Hartog L, et al. Effect of connective tissue grafting on peri-implant tissue in single immediate implant sites: a RCT. J Clin Periodontol. 2018;45(2):253-264.