You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Patients and clinicians are challenged with a multitude of clinical decisions when faced with a failing tooth in the esthetic zone. Should the tooth be extracted and grafted? Should immediate implant therapy be considered? If so, how will temporization be accomplished? These scenarios are compounded by the sense of urgency typically demonstrated by the patients facing this challenge. They want the treatment to be accomplished in the most expedited manner available to help alleviate any further embarrassment due to the loss of an anterior tooth. Thankfully, modern implant dentistry can fulfill these needs.
Immediate implant placement and provisionalization are routinely utilized to help address these issues. Immediate placement involves the instillation of the implant into a fresh extraction socket,1 which has been associated with high implant success rates,2 similar to those attained with conventional placement.3,4 Attaining adequate initial stability above 25 Ncm allows for immediate provisionalization.5 This has been linked with improved esthetics in the anterior region,6 better soft tissue stability,7 and decreased resorption of the facial cortical bone.8 When both immediate placement and immediate provisionalization protocols are utilized, the patient is able to leave the office feeling comfortable and confident having a fixed anterior interim prosthesis.
With the leveraging of dental technology in these areas, the precision and productivity of immediate placement and loading also has increased.9 Guided implant surgery with Simplant (Dentsply Sirona Implants, dentsplyimplants.com), allows for very precise, prosthetically driven implant planning.10 The clinician is able to visualize the cementoenamel junction and the incisal edge of the proposed tooth and plan the final implant relative to these areas to help ensure soft tissue stability and an esthetic outcome.11 Technology can be further utilized to design and manufacture a custom abutment and provisional or final restorations.
The protocol for Immediate Smile featuring Atlantis abutments utilizes all of these planning and manufacturing tools to simplify the clinical visit. It begins with the registration of the patient’s pre-operative condition and final restorative plan via digitized casts (or intraoral scans) and merges them with the bony conditions of the patient from their cone-beam computed tomography (CBCT) scan. The implant is planned and the Simplant project file is sent to Dentsply Sirona Implants for patient-specific SAFE Guide and Atlantis abutment design. The final plan for the custom abutment is then exported to any dental laboratory software for the design of the provisional or final restoration. The surgical guide, custom abutment, and restoration are then manufactured and returned to the clinician, allowing for efficient implant placement and provisionalization.
Case Presentation
A 62-year-old woman presented on emergency, reporting having fractured her right central incisor (Figure 1). The area was asymptomatic and demonstrated no problems other than the embarrassment associated with the loss of her front tooth. Diagnostic records were made and an Essix retainer (essix.com) was fabricated to help alleviate her immediate esthetic concerns. Due to the lack of tooth structure incisal to the gingiva, the prognosis of the tooth was very guarded. Various options to restore this area were presented to the patient, leading to her ultimate choice of a dental implant. A diagnostic CBCT scan of the patient was attained and the patient left the office wearing the retainer.
From this emergency/diagnostic visit, all relevant information was gathered to plan her treatment. The diagnostic stone casts were digitized and a digital waxup achieved in the Dental Designer CAD software, (3Shape, 3shape.com) (Figure 2). This single tooth was milled out of wax, fixed to the pre-operative cast, and digitized. The digital files were then exported in an STL file format. They were then uploaded into Simplant planning software. The DICOM file obtained from the CBCT scan of the patient was also uploaded and all three files were merged to accurately express the pre-operative situation, proposed final tooth position, and the anatomical features of the future implant site.
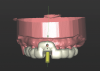
With all of this needed information relative to the pre-operative condition and proposed final tooth position, the treatment moved into the assessment and planning phase. The CBCT revealed an intact buccal plate anterior to the root of tooth No. 8 with adequate bone surrounding the area in all dimensions. Because of the favorable bony contours, an immediately placed implant was decided upon and planned in the software. The CEJ of the proposed final tooth location was identified and an OsseoSpeed EV 4.2 C - 11 mm implant (Dentsply Implants) was planned 3 mm apical and 2 mm lingual to that landmark12 to assure adequate biologic and prosthetic space for the final restoration (Figure 3 through Figure 5). A Simplant SAFE Guide was selected and ordered to convey all of the positional parameters of the final implant position, including depth control and implant timing.
The prosthetic components of the case also were planned at this time. The Simplant file registering all of the positional attributes of the implant was then imported into the Atlantis Abutment software by selecting the Immediate Smile protocol option. This allows a final abutment to be designed from the proposed implant plan. A fully anatomic patient-specific abutment in gold-shaded titanium was selected to achieve optimal soft tissue and prosthetic support.13 The digital file representing the abutment was then exported via an Atlantis Core File and imported into the 3Shape software to design an acrylic resin interim prosthesis. The surgical guide, patient-specific abutment, and interim prosthesis crown were all manufactured and returned prior to the surgical date (Figure 6).
The patient returned for her surgical visit and consent was obtained. Tooth No. 8 was extracted with the aid of periotomes maintaining the integrity of the buccal plate. The socket was curetted and irrigated with sterile saline and the Simplant SAFE Guide was placed. The assessment of the surgical guide’s intimate fit to the teeth was verified by creating occlusal and proximal windows, allowing for visual inspection to assure the guide was seated (Figure 7). The OsseoSpeed EV guided surgical kit (Dentsply Sirona Implants) was used with full depth and location drilling control. The implant was placed through the guide to its proper depth (Figure 7). An insertion torque of 35 Ncm was achieved and verified by the surgical motor, allowing for adequate initial stability for immediate loading. The timing of the implant was attained by assuring the large notch on the implant driver lined up perfectly with the channel index line on the surgical guide (Figure 8 through Figure 10). Due to the immediate nature of the implant placement, a facial gap was evident between the implant and the alveolar process. A xenograft material (Bio-Oss, Geistlich Biomaterials, geistlich-na.com) was placed to fill this gap according to established protocols.14 The Atlantis custom abutment was then placed in its proper position and the seating was verified with digital radiography. The abutment was torqued to 25 Ncm, as per the manufacturer’s specifications (Figure 11). The interim prosthesis was then placed onto the abutment and slight adjustments were made. A final custom stain and glaze was placed on the interim prosthesis crown using Lite Art coloring pastes (Shofu Dental Corporation, shofu.com). The provisional was cemented with TempBond NE (Kerr, kerrdental.com) and was relieved of any excursive contacts. The patient was given post-operative instructions and left in extremely high spirits (Figure 12).
Conclusion
In today’s fast-paced world, where patients and clinicians are demanding very efficient and practical treatments, being able to leverage the technology available with the Immediate Smile featuring Atlantis abutments protocol is a must. It allows us to examine the current state of the proposed implant site, visualize the future restorative ideal, plan the implants accordingly, and execute very precise guided surgery. The ability to then use this plan to design and manufacture the final patient-specific Atlantis abutment and a milled interim prosthesis pre-operatively simplifies the clinical and laboratory processes associated with the final step of immediate provisionalization. All of this leads to more efficient productive treatment for all parties involved.
Mark Ludlow, DMD, MS, is an Assistant Professor and Division Director of Implant Prosthodontics, at the Medical University of South Carolina’s James B. Edwards College of Dental Medicine in Charleston, South Carolina.
Manufacturer Contact Information
Dentsply Sirona Implants
dentsplyimplants.com
800-531-3481
References
1. Hammerle CH, Chen ST, Wilson TG Jr. Consensus statements and recommended clinical procedures regarding the placement of implants in extraction sockets. Int J Oral Maxillofac Implants. 2004;19(suppl):26-28.
2. Lang NP, Pun L, Lau KY, Wong MC. A systematic review on survival and success rates of implants placed immediately into fresh extraction sockets after at least 1 year. Clin Oral Impl Res. 2012;23:39-66.
3. Benic G, Mir-Mari J, Hammerle C. Loading protocols for single-implant crowns: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 2014;29(suppl):222-238.
4. Cosyn J, Hooghe N, De Bruyn H. A systematic review on the frequency of advanced recession following single immediate implant treatment. J Clin Periodontol. 2012;39:582-589.
5. Gallucci G, Benic G, Eckert S, et al. Consensus Statements and Clinical Recommendations for Implant Loading Protocols. Int J Oral Maxillofac Implants. 2014;29(suppl);287-290.
6. Buser D, Wittneben J, Bornstein MM. Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year results of a prospective study with early implant placement postextraction. J Periodontol. 2011;82:342-349.
7. Chu C, Salama M, Garber D, et al. Flapless postextraction socket implant placement in the esthetic zone: part 2. The effect of bone grafting and/or provisional restoration on peri-implant soft tissue height and thickness-a retrospective study. Int J Perio Rest Dent. 2015;35:803-809.
8. Tarnow D, Chu C, Salama M, et al. Flapless postextraction socket implant placement in the esthetic zone: part 1. The effect of bone grafting and/or provisional restoration on facial-palatal ridge dimensional change-a retrospective cohort study. Int J Perio Rest Dent. 2014;34:323-331.
9. Arisan V, Karabud CZ, Ozdemir T. Implant surgery using bone- and mucosa-supported stereolithographic guides in totally edentulous jaws: Surgical and post-operative outcomes of computer-aided vs. standard techniques. Clin Oral Impl Res. 2010;21:980-988.
10. Vercruyssen M, Cox C, Coucke W, Naert I, Jacobs R, Quirynen M. A randomized clinical trial comparing guided implant surgery (bone- or mucosa- supported) with mental navigation or the use of a pilot-drill template. J Clin Periodontol. 2014;41:717-723.
11. Cooper L. Objective criteria: guiding and evaluating dental implant esthetics. J Esthet Restor Dent. 2008;20(3):195-205.
12. Rojas-Vizcaya F. Biologic aspects as a rule for single implant placement. The 3A-2B rule: a clinical report. J Prosthodontics. 2013;22:575-580.
13. Lops D, Bressan E, Parpaiola A, Sbricoli L, Cecchinato D, Romeo E. Soft tissues stability of cad-cam and stock abutments in anterior regions: 2-year prospective multicentric cohort study. Clin Oral Impl Res. 2015;26:1436-1442.
14. Araujo MG, Linder E, Lindhe J. Bio-Oss Collagen in the buccal gap at immediate implants: a 6-month study in the dog. Clin Oral Impl Res. 2010;10:1-8.