You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The art and science of dental materials are constantly evolving to create more efficient methods of producing stronger and more esthetic restorations. Digital technology plays a large role in this evolution, as most full-service laboratories offer digitally manufactured restorations. Furthermore, a continually increasing amount of caseloads consists of CAM-milled restorations. Several new restorative materials options have been introduced that allow the dental technician to be more time efficient in fabricating beautiful, natural-appearing restorations.
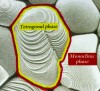
Zirconia is one of the only restorative materials that must be fabricated in the laboratory (or in the dental office) by means of digital technology. Zirconium dioxide was introduced in dentistry in the early 2000s as a substructure for single crowns and fixed partial dentures, which subsequently were layered with a veneering porcelain. Commonly referred to as zirconia, zirconium dioxide1 is now used for a full-contour monolithic single crown and multiple-unit monolithic fixed partial dentures (Figure 1). Initially, partially sintered zirconia blocks were milled and stained, and then the sintering process was completed, using a special oven for 9 to 12 hours. For individual posterior single units, for which esthetics is not as critical, a stained monolithic zirconia restoration has been acceptable.
In the anterior, zirconia was first used as a substructure fully veneered with a likely compatible porcelain. Problems began to surface such as delamination of the veneering porcelains. Chipping and bulk fractures of the veneering porcelain without exposure of the zirconia core were occurring2,3 (Figure 2). Causative factors for these failures included a disparity between the coefficients of thermal expansion between the veneering porcelain and the zirconia substructure, low fracture strength of the porcelains, framework design flaws, and sliding contact fatigue.4-6 The bond strength between a feldspathic veneering porcelain can also be affected by the sintering of the feldspathic porcelain itself and the surface treatment of the zirconia substructure.7 For single and multiple anterior units (fixed partial dentures), several fabrication modifications have changed the framework design. The lingual aspect, for example, can be left exposed and milled to full contour while the facial aspect is milled leaving space for veneering porcelains. Other modifications to the fabrication methods have eliminated, for example, the hand-layering of the veneering porcelain and replaced it with a heat-pressed method similar to the press-to-metal technique.3,8 In theory, this approach would seem to have an increase in fracture resistance with a reduction in air voids and with fewer firing cycles.3 Stawarczyk et al9 (referring to this as overpressing) found the fracture loads of PressX Zr Dentine Press Pellets (Ivoclar Vivadent, ivoclarvivadent.us), GC Initial LF (GC America, gcamerica.com), and VITA PM9 (VITA North America, vitanorthamerica.com) were not statistically significant between overpressed and layered porcelain systems. Only IPS e.max® ZirPress (Ivoclar Vivadent) was found to have a significantly higher fracture load than that of the layering porcelains used: ZIROX® (Wieland Dental Systems, wieland-dental.de), GC Initial ZR (GC America), VITA VM9 (VITA North America), or IPS e.max Ceram (Ivoclar Vivadent).
Another modification to the fabrication of a veneered zirconia bridge restoration is the CAD-on restoration technique in which the veneering portion of the restoration is milled and then secured to the fully sintered zirconia framework. For example, a feldspathic material (VITABLOCS® TriLuxe Forte, VITA North America) can be milled and then cemented to the framework with a resin cement, or a lithium disilicate (IPS e.max CAD, Ivoclar Vivadent) can be milled and then attached to the fully sintered zirconia framework using glass-fusion ceramics10 before the CAD material is crystalized or sintered. Few studies are available on the efficacy of this technique. Comparing the two milled materials at the same thickness, Hill et al11 found the lithium disilicate version to have higher strength than the feldspathic material. In another study, Watzke et al12 had the same results. Aboushelib et al13 reported that the higher tensile strength of press-on veneer material (lithium disilicate) and the superior quality of the interface can prevent porcelain chipping. Schmitter et al14 assessed the ultimate load to failure of CAD/CAM (lithium disilicate) overpressed zirconia restorations and found when compared with hand-layered veneer-to-zirconia restorations after artificial aging, 87.5% of the latter version failed during chewing simulation, whereas the former version reached ultimate loads to failure of about 1600 N.
Polychromatic Full-Contour Zirconia
Despite improvements in materials science and processing techniques, porcelain-to-zirconia restorations remain susceptible to chipping and delamination. Lazari et al15 reported that incomplete bonding between the veneering porcelain and zirconia framework can affect the biomechanical behavior of the ceramic veneer, increasing chipping or fractures.
In recent years, the growing trend has been toward monolithic full-contour zirconia restorations, eliminating the veneering. Full-contour zirconia single units were first placed in the posterior regions mostly because of the inferior esthetic qualities. This poor appearance was due to the large grain size creating a high level of opacity.16,17 In the laboratory, the milled monolithic opaque crown then required a time-consuming manual dip-coloring and drying technique before the lengthy sintering. The introduction of pre-shaded blocks has helped to decrease the time required to produce an esthetic monolithic zirconia restoration. For example, Zirlux® (Zahn Dental, zahndental.com) has 5 pre-shaded milling discs to initiate the fabrication of the restoration. The technician then can use a combination of the 10 stains and 6 modifiers before applying a final glaze.
Taking the pre-shaded concept even further, multi-shaded zirconia milling discs are now available that simulate the color gradients of the natural tooth. KATANA™ polychromatic multi-layered zirconia milling discs (Kuraray America, kuraray.us.com) do not require coloring and drying. The milling discs consist of 4 pre-colored layers that transition from the enamel through the dentin and end in cervical shades. Depending on the shade prescription, the technician can vary the position of the planned restoration relative to the shaded discs. After the material is milled, the sintering process can be completed, resulting in a less time-consuming polychromatic restoration.
Translucent Full-Contour Zirconia
A material is said to be translucent when a portion of light is transmitted and scattered.18 A material’s level of translucency can be determined by the translucency parameter (TP) or the contrast ratio (CR). The TP value is described as the difference in color of a material with a uniform thickness over a black and white background.19 For example, the TP value of human dentin is 6.6 and 11.6 for enamel,20 whereas a material with a value of zero is absolutely opaque.21 A higher TP value translates to a higher translucency.
The CR, meanwhile, is a measured difference of white-light reduction from a specimen placed over a black (Yb) and white (Yw) background.22 The contrast ratio is calculated as CR = Yb/Yw. The lower the CR value, the higher the translucency. Therefore, as the level of translucency of a material becomes greater, the TP value increases and the CR decreases.23
A natural tooth is comprised of high translucent light-transmitting enamel and a lesser translucent, more light-scattering dentin.24 The level of translucency of enamel and dentin depends on the wavelength of the emitted light. A higher wavelength translates to a higher translucency value.25 The goal of ceramic manufacturers is to produce a restorative material that approaches the optics found in nature. The translucency level of dental porcelains is determined by the size, chemical nature, and amount of crystals in the matrix.26 The translucency in zirconia is derived from the level of alumina particles, impurities, and structural defects that cause the light to scatter. When the source of light-scattering particles decreases, the level of translucency increases.27
The thickness of ceramic material also affects the translucency. Wang et al28 reported that as the thickness of the ceramic material increases, the degree of translucency decreases. Therefore, the type of zirconia used for full-contour restorations, having a greater thickness than the veneered porcelain-to-zirconia, must be modified to create the translucency required.
The strength of zirconia increases with the addition of alumina.29 However, because alumina has a different refractive index30 than zirconia, translucency diminishes. A number of manufacturers have introduced new formulations of full-contour zirconia restoratives that have varying degrees of translucency and strength.
3M™ ESPE™ (3mespe.com) changed the distribution and content of aluminum oxide in Lava™ to 0.1 wt%, creating a more translucent version and at the same time maintaining the strength of the product. The new Lava Plus High Translucency Zirconia still has less translucency than glass ceramics but has four times the strength.31
Sagemax Bioceramics Inc. (sagemax-dental.com) introduced its first line of zirconia, NexxZr-White, in 2011. That product has a biaxial flexural strength of 1150 MPa. In 2013, Sagemax launched a pre-shaded version called NexxZr-19 Pre-shaded that has a flexural strength of 1300 MPa and is available in 19 shades. For milling purposes, the position of the restoration can be adjusted in the milling disc depending on the amount of color required throughout the restoration. This year, Sagemax introduced NexxZrT, which has a biaxial flexural strength of 1150 MPa, a 35% 1-CR translucent factor (1 mm), and a 50% light transmission at 0.6 mm thickness. This version has the most translucency in the incisal area.
Zenostar® Full Contour Zirconia (Ivoclar Vivadent) is available in 6 pre-shaded milling discs. The Zenostar Zr Translucent has a 40% light transmission at 0.6 mm, with less than 0.1% aluminum oxide and a flexural strength of 1200 MPa.
BruxZir® (Glidewell Laboratories, glidewelldental.com) is another zirconia restorative that can be utilized as a full-contour material. With an average flexural strength of 1200 MPa, BruxZir milling discs are also available in pre-shaded versions.
Bunek et al32 measured the translucency of 4 unshaded full-contour zirconia ceramics—BruxZir, Lava Plus, NexxZr T, and Zenostar—at thicknesses of 0.5 mm and 1.0 mm. The TP value was calculated using a ColorEye spectrophotometer (X-Rite, xrite.co). With wavelength ranges from 360 nm to 750 nm, BruxZir was the most translucent among the 0.5-mm specimens. In the 1.0-mm specimen samples, BruxZir and NexxZr T were more translucent than the other two. The results showed that all specimens were more translucent in the thinner-version samples, which were similar to the findings of Wang et al.28
Newer Improvements
The esthetic qualities of full-contour zirconia restorations increase with a reduction of the porosity,33 decrease in the grain size,33 and adjustments to the block or disc processing technique34 and sintering parameters.35,3 Klimke et al37 found that a particle size smaller than 40 nm was necessary to achieve a light transmittance of 50% through a specimen with a thickness of 1.0 mm.
Manufacturers of dental ceramics have always focused on strength and esthetics in their development of restorative materials. A move toward monolithic restorations is a viable approach to eliminating the risk for failures. The creation of translucent ceramics with the highest strength continues to be a high priority. Zirconia formulations and processing are constantly changing, including the methods for characterizing the restorations with improved stains and technique.
Currently, fully stabilized cubic zirconia (ZrO2) is drawing interest because of the high refractive index. Although the flexural strength of the cubic form is approximately 700 MPa, which is significantly less than the tetragonal form, this version of zirconia is still stronger than lithium disilicate (400 MPa)38 and similar in translucency.
Recently introduced, cubeX2 Cubic Zirconia (DAL DT Technologies, daltechsystems.com) is a full-contour zirconia milling material utilizing the cubic form of zirconia. The approach that cubeX2 Cubic Zirconia uses to achieve a higher level of translucency is different in terms of formulation. In order to increase the translucency of standard zirconia (30% translucency), 5 mol% yttria has been added to the 3 mol% yttria (standard zirconia formula) in a combination of 53% cubic form to 47% tetragonal form, which makes the material 19% more translucent. The addition of the cubic form allows for more light absorption, achieving a higher level of translucency, whereas the tetragonal form reflects more light, leading to opacity. So by increasing the amount of the cubic form and decreasing the amount of the tetragonal form, the level of translucency increases. According to the manufacturer, this highly translucent cubic/tetragonal combination has a flexural strength of 720 MPa (Type II Class V) and can be used in full contour for single units and 3-unit bridges in all areas of the mouth.
Another new material, Imagine™ (Jensen Dental, jensendental.com) is a Y-TZP (yttria stabilized tetragonal zirconia polycrystalline), a high translucency material that meets the International Standards Organization (ISO) 6872:2008 requirement of a Type II Class V ceramic with a flexural strength of 760 MPa, according to the manufacturer. It can also be used in full contour for single units or 3-unit bridges or as a coping or framework.
Surface Finish
As with all types of full-contour zirconia restorations, the structural integrity is affected by the surface finish.39 Manawi et al40 found that ground, finished, and polished zirconia had a lower flexural strength and fracture toughness than glazed zirconia. After glazing, a smooth topographic surface could not be reached even after finishing and polishing. Clinically, most dental offices do not have the capability to re-glaze zirconia after occlusal adjustments are made. Therefore, it is paramount that the finishing and polishing process be easy for the clinician to provide. To remove diamond bur marks, most manufacturers recommend diamond-impregnated rubber points and discs for finishing surfaces after occlusal adjustments are made chairside. Miyazaki et al41 reported that a diamond paste was essential in reducing the surface roughness and gloss to an adjusted zirconia surface. For the dentist, a disposable brush has now been impregnated with a diamond polishing paste (Zircon-Brite, Dental Ventures of America, dentalventures.com) and can be used for the final step in restoring the zirconia surface. These RA latch-type brushes provide the clinician with the access to apply the diamond polishing paste for 2 to 3 restorations without the concern of cross-contamination (Figure 3).
Standards and Classifications
Often, restorative materials are labeled with an ISO classification type and number. Numerous standards organizations exist throughout the world. In the US, a major one is the American National Standards Institute, which officially represents the US in the ISO.42 A number of technical societies and organizations representing specific fields contribute data. For example, the American Dental Association has developed standards in the US and accepts the worldwide ISO standards.42 In 2008,43 the ISO revised its 1995 standard for dental ceramics (ISO 6872:1995) to ISO 6872:2008, in which Clause 4 specifies 2 ceramic types: Type I ceramic products, which are provided as powders, pastes, and aerosols; and Type II, which includes all other forms of ceramic products such as millable zirconia blocks and discs. This standard further categorizes ceramics by a classification based on flexural strength.44 Class I ceramics are for esthetic coverage of metal or ceramic substructures and single-unit anterior restorations, including veneers, inlays, and onlays, and should have a minimum flexural strength of 50 MPa. Class II ceramics are esthetic ceramics for adhesively cemented restorations used in the anterior and posterior regions and adhesively retained anterior and posterior ceramic substructures with a flexural strength of 100 MPa. Class III ceramics are nonadhesively retained anterior and posterior single units with a flexural strength of 300 MPa. Class IV ceramics are nonadhesively retained single-unit substructures used in the anterior and posterior regions having a flexural strength of 300 MPa. This class also includes 3-unit ceramic substructures not involving molar restorations. Class V ceramics include 3-unit substructures that do involve molar restorations and have a flexural strength of 500 MPa. Finally, Class VI ceramics include 4-or-more-unit substructures with a flexural strength of 800 MPa.44
This clarification of the ISO 6872:2008 standard allows the reader to discern the labeling of restorative materials that is found in the manufacturers’ information packets.
Conclusion
The new milling products available continue to improve the quality and esthetics of restorative materials with greater longevity and diminishing the failure rate. Manufacturers continue to progress in the development of dental restorative materials benefiting not only the clinician and technician but also, most importantly, the patient.
Acknowledgment
The author would like to thank Bryer F. Helvey for his contribution.
References
1. Helvey, GA. Zirconia and computer-aided design/computer-aided manufacturing (CAD/CAM) dentistry. Inside Dentistry. 2008;4(4):72-79.
2. Al-Dohan HM, Yaman P, Dennison JB, et al. Shear strength of core-veneer interface in bi-layered ceramics. J Prosthet Dent. 2004;91(4):349-355.
3. Coelho PG, Silva NR, Bonfante EA, et al. Fatigue testing of two porcelain-zirconia all-ceramic crown systems. Dent Mater. 2009;25(9):1122-1127.
4. Hung C-Y, Huang Y-S. Effect of veneering techniques on ceramic fracture of zirconia restoration. J Prosthodont Imp. 2012;1(2):66-70.
5. Coelho PG, Bonfante EA, Silva NR, et al. Laboratory simulation of Y-TZP all-ceramic crown clinical failures. J Dent Res. 2009;88(4):382-386.
6. Sailer I, Fehér A, Filser F, et al. Prospective clinical study of zirconia posterior fixed partial dentures: 3-year follow-up. Quintessence Int. 2006;37(9):685-693.
7. Ramos CM, Cesar PF, Lia Mondelli RF, et al. Bond strength and Raman analysis of the zirconia-feldspathic porcelain interface. J Prosthet Dent. 2014;112(4):886-894.
8. Helvey GA, Miolen K. Evolution of impression-free techniques for zirconia-based restorations. Inside Dentistry. 2007;3(10):72-76.
9. Stawarczyk B, Ozcan M, Roos M, et al. Load-bearing capacity and failure types of anterior zirconia crowns veneered with overpressing and layering techniques. Dent Mater. 2011;27(10):1045-1053.
10. Daou EE. The zirconia ceramic: strengths and weaknesses. Open Dent J. 2014;8:33-42.
11. Hill TJ, Chlosta K, Tysowsky G. The fracture load of three CAD-CAM veneering systems over zirconia [abstract 3215]. Presented at: IADR/AADR General Session & Exhibition; March 19, 2011; San Diego Convention Center.
12. Watzke R, Peschke A, Roulet JF. 12 months clinical performance of CAD-on-restorations [abstract 544]. Presented at: IADR/AADR General Session & Exhibition; March 17, 2011; San Diego Convention Center.
13. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: zirconia veneering ceramics. Dent Mater. 2006;22(9):857-863.
14. Schmitter M, Mueller D, Rues S. Chipping behaviour of all-ceramic crowns with zirconia framework and CAD/CAM manufactured veneer. J Dent. 2012;40(2):154-162.
15. Lazari PC, Sotto-Maior BS, Rocha EP, et al. Influence of the veneer-framework interface on the mechanical behavior of ceramic veneers: a nonlinear finite element analysis. J Prosthet Dent. 2014;112(4):857-863.
16. Dias MC, Piva E, de Moraes RR, et al. UV-Vis spectrophotometric analysis and light irradiance through hot-pressed and hot-pressed-veneered glass ceramics. Braz Dent J. 2008;19(3):197-203.
17. Tsukuma K, Yamashita I, Kusunose T. Transparent 8 mol% Y2O3–ZrO2 (8Y) ceramics. J Am Ceram Soc. 2008;91(3):813-818.
18. Goodman G. Relation of microstructure to translucency of porcelain bodies. J Am Ceram Soc. 1950;33(2):66-72.
19. Johnston WM, Reisbick MH. Color and translucency changes during and after curing of esthetic restorative materials. Dent Mater. 1997;13(2):89-97.
20. Ryan EA, Tam LE, McComb D. Comparative translucency of esthetic composite resin restorative materials. J Can Dent Assoc. 2010;76:a84.
21. Kurtulmus-Yilmaz S, Ulusoy M. Comparison of the translucency of shaded zirconia all-ceramic systems. J Adv Prosthodont. 2014;6(5):415-422.
22. Shono NN, Al Nahedh HN. Contrast ratio and masking ability of three ceramic veneering materials. Oper Dent. 2012;37(4):406-416.
23. Yu B, Lee YK. Translucency of varied brand and shade of resin composites. Am J Dent. 2008;21(4):229-232.
24. Nakagawa Y. Analysis of natural tooth color. Shikai Tenbo. 1975;46:527-532.
25. Yu B, Ahn JS, Lee YK. Measurement of translucency of tooth enamel and dentin. Acta Odontol Scand. 2009;67(1):57-64.
26. McLean JW. The Science and Art of Dental Ceramics. Volume 1: The Nature of Dental Ceramics and Their Clinical Use. 1st ed. Chicago, IL: Quintessence Publishing Co; 1979.
27. Fujisaki H, Kawamura K, Imai K. Transparent zirconia powder Zpex suitable to dental materials. Tosoh Res Tech Review. 2012;56:57-61.
28. Wang F, Takahashi H, Iwasaki N. Translucency of dental ceramics with different thicknesses. J Prosthet Dent. 2013;110(1):14-20.
29. de Moraes MCC, Elias CNE, Filho JD, Oliveira LG. Mechanical properties of alumina-zirconia composites for ceramic abutments. Mat Res. 2004;7(4):643-649.
30. Kumar P, Wiedmann MK, Winter CH, Avrutsky I. Optical properties of Al2O3 thin films grown by atomic layer deposition. Appl Opt. 2009;48(28):5407-5412.
31. Wang F, Takahashi H. Translucency and biaxial flexural strength of dental ceramics. J Dent Res. 2012;91(spec iss a):422.
32. Bunek SS, Baumann A, Yapp R, et al. Translucency of CAD/CAM ceramics. The Dental Advisor. 2014;59. http://www.bruxzir.com/downloads/Translucency-of-CAD-CAM-Ceramics.pdf. Accessed March 26, 2015.
33. Zhang HB, Kim BN, Morita K, et al. Effect of sintering temperature on optical properties and microstructure of translucent zirconia prepared by high-pressure spark plasma sintering. Sci Technol Adv Mater.2011;12(5)1-6. doi:10.1088/1468-6996/12/5/055003.
34. Ilie N, Stawarczyk B. Quantification of the amount of blue light passing through monolithic zirconia with respect to thickness and polymerization conditions. J Prosthet Dent. 2015;113(2):114-121.
35. Stawarczyk B, Ozcan M, Hallmann L, et al. The effect of zirconia sintering temperature on flexural strength, grain size, and contrast ratio. Clin Oral Investig. 2013;17(1):269-274.
36. Jiang L, Liao Y, Wan Q, Li W. Effects of sintering temperature and particle size on the translucency of zirconium dioxide dental ceramic. J Mater Sci Mater Med. 2011;22(11):2429-2435.
37. Klimke J, Trunec M, Krell A. Transparent tetragonal yttria-stabilized zirconia ceramics: influence of scattering caused by birefringence. J Am Ceram Soc. 2011;94(6):1850-1858.
38. Helvey GA. Chairside CAD/CAM. Lithium-disilicate restoration for anterior teeth made simple. Inside Dentistry. 2009;5(10):58-67.
39. Aboushelib MN. Long term fatigue behavior of zirconia based dental ceramics. Materials. 2010;3(5):2975-2985.
40. Manawi M, Ozcan M, Madina M, et al. Impact of surface finishes on the flexural strength and fracture toughness of In-Ceram Zirconia. Gen Dent. 2012;60(2):138-142.
41.Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. J Prosthodont Res. 2013;57(4):236-261.
42. Abbey LM, Zimmerman JL, eds. Dental Informatics: Intergrating Technology into the Dental Environment, Springer-Verlag New York, NY, 1992.
43. Fischer J, Stawarczyk B, Hammerle CH. Flexural strength of veneering ceramics for zirconia. J Dent. 2008;36(5):316-321.
44. Vichi A, Sedda M, Del Siena F, et al. Flexural resistance of Cerec CAD/CAM system ceramic blocks. Part 1: chairside materials. Am J Dent. 2013;26(5):255-259.
About the Author
Gregg A. Helvey, DDS, MAGD
Adjunct Associate Professor
Virginia Commonwealth University School of Dentistry
Richmond, Virginia
Private practice
Middleburg, Virginia