You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
There is often controversy regarding the best course of treatment when evaluating the clinical options for either root canal therapy (and maintenance of the natural tooth) or extraction and tooth replacement with a dental implant. Although predictable, implant placement can be challenging in the esthetic zone where numerous criteria must be evaluated by the restorative team. The science of endosseous root-form implants has advanced considerably with the development of new implant designs, surface characteristics, materials, and methods. High success rates have helped make dental implants a viable and accepted option for tooth replacement, and the debate is intensifying.
Clinicians have a growing number of options in the commercial marketplace for both treatment modalities. Clinical recommendations vary depending on their source (empirical, literature-based, manufacturers' information, etc). In addition, techniques using these various options and systems are constantly being developed and both choices continue to provide improved clinical success. This article discusses the current considerations in treatment planning for retention of the natural tooth through endodontic therapy (including orthograde first-time treatment, retreatment, and endodontic surgery) versus extraction and placement of the dental implant. As a secondary goal, the article describes several specific cases in which the best option is either an implant or retention of the natural tooth. Additionally, the article addresses these same questions with regard to the specific clinical diagnosis of resorption in all of its various forms.
The complexity and controversy regarding endodontic versus implant treatment planning was recently addressed by Hannahan and Eleazer, who reported a success rate of 99.3% after following 143 root canal-treated teeth for 22 months; this percentage was higher than the implant group, in which 129 were followed for 36 months with a success rate of 98.4%. The success of endodontically treated teeth and implants was essentially the same, but implants required more postoperative treatments for maintenance. The study also concluded that the data showed implants required significantly more follow-up treatment or surgical intervention after the procedure as compared to endodontically treated teeth (12.4% versus 1.3%).1 The clinically accepted protocol for retention of a nonvital tooth has been to perform root canal therapy followed by conventional crown-and-bridge procedures. Before the advent of modern implant therapy, removal of the tooth with subsequent implant placement was considered high risk and not the standard of care.
Tooth retention and implant therapy can be competing options in developing a definitive treatment plan. The use of risk assessment throughout the treatment-planning process is essential due to the definitive changes that occur because of tooth removal. The development of a predictably successful long-term restorative/prosthetic treatment plan requires careful evaluation of the various factors that influence the prognosis of the teeth involved. Risk assessment consists of identifying all clinical factors, both local and systemic, that can affect the biologic and mechanical functions of that tooth. Table 1 lists the major factors that should be considered in determining the periodontal prognosis of teeth.
In assessing long-term periodontal stability, bear in mind that periodontal disease is characterized by attachment loss resulting in various osseous defects that reduce the overall periodontal support. Bone-grafting procedures with guided tissue regeneration (GTR) have shown success in many types of periodontal defects. The success of regeneration depends on the architecture and location of the defect, tooth mobility, and other factors, some of which are listed in Table 1. The degree of furcation determines the success rate with most GTR procedures. If the tooth does not require a terminal bridge abutment, then retention with periodontal therapy and/or endodontic therapy, if indicated, may be a reasonable choice versus extraction and implant therapy. Tooth mobility is critical to the assessment process. The prognosis for a tooth with compromised periodontal support and the mobility that results can adversely affect the retention, especially if the tooth is to be used as an abutment. Splinting of mobile or otherwise compromised teeth to implants by a fixed prosthesis is not recommended unless there are extenuating circumstances.
Retention Versus Extraction
Retention of the natural tooth versus extraction/implant therapy requires consideration of additional factors. The definitive treatment depends on the long-term predictability of the final outcome. Risk factor assessment, in addition to local considerations, includes the effects of systemic illness. Tobacco use and poorly controlled diabetes mellitus are concerns because both increase the risk for periodontal disease in addition to affecting implant healing. The patient's genetic susceptibility to periodontal disease can also be a critical factor. Patients can be evaluated by a simple diagnostic test for the presence of a pro-inflammatory genotype that is associated with the production of interleukin-1ß, an inflammatory mediator. These patients are more susceptible to further disease progression, unlike a patient without this genotype. This factor can impact tooth retention and should be considered in the risk assessment process.
In addressing the options of endodontic treatment versus implants, the clinician should obtain a thorough, informed patient consent that includes alternative treatment options, risks and benefits of each, and the risks of choosing no treatment (the clinician's best interest financially should be excluded).2 The patient's input in every aspect of the treatment-planning process is essential. When options and parameters are explained, most patients strongly prefer a particular treatment based on their needs, especially if the prognosis is equally weighted for both endodontics versus implants.
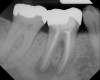
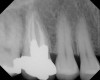
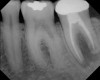
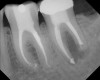
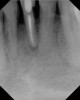
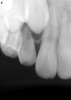
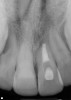
As mentioned, all risk factors associated with both root canal and implant therapy must be carefully considered. Comprehensive clinical and radiographic assessments are necessary to evaluate the patient's risk factors associated with his or her particular case (Figure 1, Figure 2 and Figure 3). The primary risk factors for implants can include smoking, bone quality, and systemic health. For endodontic therapy the primary risk factors are related to the anatomic root complexity, failed root canal treatment with significant technical defects manifested as iatrogenic events, less-than-optimal periodontal status of the tooth (due to a subsequent risk of vertical fracture), and a clinician's lack of experience with regard to the case's complexity. A strong correlation exists between failed root canal treatment and a lack of coronal seal after treatment. This is highly relevant in treatment planning. Often, endodontically treated teeth fail not because they were treated inappropriately and need extraction, but rather, because they have been left unsealed and assaulted by bacteria after the endodontic therapy, causing subsequent long-term clinical failure (Figure 4 and Figure 5).
Generally, treatment options for either modality should be based on case complexity, patient factors, tooth factors, periodontal status, systemic health, the intended functional and strategic value of the tooth, the patient's esthetic desires and financial considerations, in addition to numerous other factors (Table 2). All of these factors can significantly complicate treatment planning and impact the case's outcome.
A comprehensive discussion of the impact of each of the risk factors to endodontic therapy and implants listed in Table 2 is not feasible. However, it should be mentioned that as the number of risk factors increases, the indications for referral rise and the case may require, at a minimum, a multidisciplinary treatment-planning approach and involve specialists for either consultation or to perform limited aspects of the treatment. The authors suggest that the general practitioner, while making treatment-planning decisions, obtain consultations when either an implant and retreatment or endodontic surgery may both be appropriate. Doing so can allow for extraction of teeth that are nonrestorable and enable the practitioner to avoid further attempts to save teeth that may be vertically fractured already or are at high risk of vertical fracture. Some endodontic retreatment case types will have much better outcomes than others. In these cases, providing patients an evaluation of the feasibility of both endodontic treatment and implants can help them receive the most cost-effective and efficient treatment.
Microscopic Endodontic Retreatment
The past 15 years have seen a number of significant advancements that have accelerated the subspecialty of endodontic microsurgical retreatment. While some failed root canals are certainly beyond treatment, teeth that previously needed removal or endodontic surgery can now be retreated predictably. The advent of the surgical operating microscope, ultrasonic, ultrasonic tips, rotary nickel titanium files for both canal shaping and removal of obturation materials, as well as using reciprocation for removing ledges, along with a host of other advances, have made revision of past failed root canal treatment not only possible but also predictable. Referral is essential for the clinician to help decide if the tooth in question, assuming that it is periodontally sound and restorable, can be retreated. Again, informing the patient of all possible and probable treatment that will be required in addition to retreatment will enable the patient to make an informed decision regarding the long-term advisability of tooth retention or extraction.
The use of cone-beam computed tomography (CBCT) has revolutionized clinical diagnostic abilities. Featuring advantages such as a relatively small size, less radiation exposure, and lower cost, CBCT has gained popularity by improving predictability and the quality of care in implant dentistry. This technology has value in aiding in the diagnosis of root fractures. Recently, a study found dental CBCT exhibited greater accuracy (62.8% versus 54.5%) in helping to diagnose vertical root fractures than conventional radiography. The investigators concluded that use of dental CBCT is effective for the diagnosis of root fractures regardless of the direction.3
CBCT has been available for craniofacial imaging since 1999 in Europe and since 2001 in the United States. The scanner uses a cone-shaped x-ray beam rather than a conventional linear fan beam to provide images of the skull's bony structures. CBCT uses a square 2-dimensional (2-D) array of detectors to capture the cone-shaped beam. Subsequently, reconstruction software is applied on the CBCT volumetric data to produce a stack of 2-D gray-scale level images of the anatomy.
Cost Impact on TREATMENT PLANNING
Specific attention has been given to the cost differences regarding implants versus endodontic therapy,2,4,5 as previous articles and resources have compared treatment expenses. A treatment cost analysis should be considered in all treatment required to retain the tooth in question. Evaluating restorative needs and long-term success in addition to endodontic requirements is essential in determining the tooth's long-range prognosis. Restorative success often depends on the status of the periodontium surrounding the tooth at the time of restoration. Crown lengthening in addition to GTR procedures are often indicated for tooth retention. The total cost of therapy, taking into account all these variables, will influence many patients' treatment decisions at the outset.
The practitioner should complete a comprehensive evaluation and anticipate the scope of treatment, including the aforementioned crown lengthening and other potential procedures, required to retain the tooth and present this to the patient. The patient must fully understand all long-term implications of treatment—financial and clinical. Often, in actual practice, the total cost of treatment may be unknown at the outset because additional procedures might be required that were not anticipated when developing the initial treatment plan. This informational exclusion is preventable if the aforementioned comprehensive examination and consultation is undertaken with the patient. This underscores the importance of obtaining consultations, when needed, with both the clinician placing the implants (periodontist or oral surgeon) and/or the endodontist.
When making a case presentation, the clinician should consider that from a purely pathologic viewpoint Nair and colleagues found that approximately 10% of all periapical lesions require surgery in addition to conventional endodontic therapy.6 Some cases warrant surgery or intervention with endodontic retreatment due to iatrogenic procedural errors (eg, apical transportation, perforation, ledging, and separated instruments) and anatomic considerations (eg, apical ramifications and isthmuses) that influence clinical success. Iatrogenic events in endodontics are entirely avoidable if they are foreseen and alternate actions are taken. When endodontic retreatment could destroy the prosthesis (ie, crown, post, and core), surgical intervention, depending on the specific clinical situation, may be considered a more conservative approach.7
This finding should be tempered with the sobering clinical truth that coronal microleakage is a significant source of endodontic failure. Also, indiscriminant endodontic surgery can lead to long-term failure if the coronal microleakage is not addressed. Specifically, performing apical surgery on a tooth in the presence of coronal microleakage will promote less-than-optimal clinical results postsurgery. In many of these cases, the tooth may need retreatment first, placement of an adequate coronal seal, and, if indicated, apical surgery. In addition, apical surgery, by removing some root end length, can lead to increased risk of vertical root fracture.
Single-Tooth Anterior Trauma
Single-tooth anterior trauma cases are especially challenging. To determine the prognosis of the injured tooth, the clinician needs to assess the degree of damage to the tooth and associated periodontium. The prognosis of retaining the tooth versus removal for subsequent implant placement should be based on pulpal status, remaining tooth structure, damage to the supporting structures, and the long-term risk of resorption depending on the degree of trauma.8,9 Careful clinical and radiographic assessment is crucial in the treatment-planning process to avoid unnecessary treatment on teeth that might be better replaced with implant therapy. Restoration of anterior trauma cases often requires a multidisciplinary approach to maximize the esthetic outcome.
These cases, in which the tooth and periodontium can be severely compromised, are extremely challenging and, because there is often no single ideal solution, involve complex treatment planning. The scope of treatment may include periodontal, endodontic, orthodontic, and prosthodontic intervention to restore form and function. Sufficient quality and quantity of bone are major prerequisites for the placement of dental implants into the alveolar ridge. Loss of bone volume (vertical and horizontal dimension) as classified by Siebert10 can significantly impact the treatment-planning sequence associated with anterior trauma cases. GBR may be necessary prior to implant placement, as may soft-tissue augmentation, based on the severity of the ridge defect. To predictably gain vertical bone height, the clinician may need to consider distraction osteogenesis or orthodontic extrusion. Extensive preoperative planning and treatment coordination are necessary for success; the most common treatment options to consider in these cases are:11
- retention of the tooth (endodontic, periodontal, orthodontic, and restorative therapy) and attempts at restoration.
- removal of the tooth and replacement with a single-tooth implant.
- removal of the tooth with no replacement.
- removal of the tooth and placement of a conventional fixed partial denture (using adjacent abutment teeth).
Incomplete Maxillofacial Growth
Another clinical scenario that complicates treatment planning and requires special care and consideration is trauma in a patient with incomplete maxillofacial growth. With trauma, the patient's age will significantly impact treatment choice as various treatment options for a young patient with incomplete maxillofacial growth are available. Argonin and colleagues showed, on average, young women complete their growth at age 17.8 years and young men at age 20.12 Treatment planning for a younger patient will differ significantly from that of an adult patient. For a completely grown adult, management of the traumatized tooth is not nearly as complicated.
Implant therapy should be delayed until the end of skeletal growth. The placement of implants in growing patients is not recommended as a routine practice because submergence or infraposition of the implants may result in complications in growing patients. Maintaining the traumatized tooth until all maxillofacial growth is complete can minimize case complexity. Comprehensive assessment of the traumatized tooth should be performed with endodontic, periodontal, and restorative input in addition to orthodontic consultation, especially when evaluating a patient's skeletal growth. Immediate treatment may be rendered dependent on the definitive treatment plan.13
Managing Resorption
The management of resorption is another key aspect of treatment planning when considering tooth retention versus extraction/implant placement. A complex entity, resorption, in all of its forms, can complicate endodontic treatment-planning considerations. An endodontist is best suited to treat resorption. A lack of referral when indicated can reduce the prognosis for this class of cases. The term resorption encompasses external root resorption (ERR) and internal root resorption (IRR).
It is theorized that both precementum and predentin are the barriers to ERR and IRR. If the cemental layer is absent or damaged, canal toxins can reach the periodontal ligament (PDL) through the dentinal tubules that drive the ERR resorptive process. Alternatively, if a tooth is necrotic, bone resorption can occur. However, root resorption will generally not occur if the precemental layers are present. If the odontoblastic layer and predentin layer are lost, in combination with a nonvital pulp, IRR can occur.
IRR can be further broken down into replacement resorption (RR) and internal inflammatory resorption (IIR). RR is characterized by dentin resorption with hard-tissue deposition in the canal. IIR also denotes dentin resorption but no hard-tissue deposition. IIR is commonly found cervically and is clinically observed as a pink hue that is transparent through the enamel. IRR is rare in human permanent teeth and asymptomatic.8
There is some debate as to the exact source and nature of the pulp tissue found in IRR. One author suggests that the tissue is "metaplastic" in nature. Yet another proposes that the pulp tissue is replaced by connective tissue with osteogenic and osteoclastic capabilities, which are substantially different from normal pulp. In either event, odontoblasts or predentin are scarce in the presence of IRR.14,15
ERR has four subtypes: external surface resorption (ESR), external inflammatory root resorption (EIRR) (which is further subdivided into a cervical subclassification resulting from a physical or chemical insult to the cervical epithelial attachment), transient apical breakdown, and ankylosis. IRR and ERR can be present simultaneously on the same tooth, and the two independent lesions may reach one another.8,16,17 Nonvital teeth with periapical radiolucencies demonstrate the highest occurrence of ERR apically. ERR has also been found apically in vital teeth with apices that are radiographically normal.18,19 To a statistical significance, teeth with root canal fillings demonstrate less ERR than nonvital teeth without root canal fillings.19
According to Trope20, EIRR falls into two primary classes: a self-limiting injury, whereby after the injury once the damaged tissue on the root surface is removed healing can occur; and a progressive stress, in which the injury occurs and an inflammatory stimulus is present, preventing healing.
Self-limiting injury: A self-limiting injury can be mild or severe. If mild, a localized area of resorption can occur due to damage of the cemental surface, and healing can be expected in 14 days. Many of these defects are not radiographically visible. If the tooth is vital or has no evidence of pulpal necrosis, the clinician should wait and observe if healing occurs. If the tooth undergoes a mild injury such as a subluxation and has no additional inflammatory stimuli, spontaneous healing and repair of the surface of the root can take place in approximately 14 days. If the injury is severe, as in intrusive luxation and avulsion, ERR can result.
Progressive stress: In the case of a severe injury (intrusion or tooth avulsion with an extended dry time), the attachment of the tooth can be produced after healing. After the initial inflammation and if cementum is lost, ankylosis is a risk. Damage to the precementum is common in avulsion injuries and related to the length of dry time. If an inflammatory stimulus such as a nonvital pulp is present, long-standing ERR can continue until the root is destroyed or therapy is performed to arrest the resorption. After trauma, the cell type that attaches to the root surface determines the degree of healing possible. If cementoblasts reattach to the root surface, healing is more predictable. A lack of cementoblast attachment after trauma will result in ankylosis (with root structure being replaced by bone). If more than 20% of the root surface is damaged from trauma, ankylosis is predictable. Alternatively, smaller areas of root damage favor deposition of cementum and healing without ERR. 21 After ankylosis has occurred, it cannot be resolved.
It is noteworthy that dry times greater than 15 minutes in cases of avulsion are correlated with ERR, with the wet storage medium showing no significant association with the development or prevention of ERR. Teeth with visible contamination at the time of intentional replantation have been shown to provide a more rapid onset of ERR. EIRR has a more rapid onset than ankylosis.22
As an aside, one study used radiographic evaluation to assess idiopathic resorption. The investigators found all patients demonstrated ERR apically in at least one root of a permanent tooth. In 81% of the teeth observed, no clear or obvious reason for the ERR was evident. As a result, it was concluded that idiopathic resorption is common and exists in all permanent dentitions. The same study also noted that orthodontics was correlated with ERR to various degrees.23
Treatment modalities associated with all types of resorption have been comprehensively summarized by Trope.24 The recommendations here are adapted from his work. In the most general terms, treatment for resorption is divided into those cases that possess either a short- or long-term stimulus. For cases with a short-term stimulus that may or do have a damaged PDL, treatment includes:
- efforts to prevent injury in the first place.
- preventing additional damage after the initial injury (replantation of the avulsed tooth within 15 minutes).
- pharmacologic manipulation (minimize the initial inflammatory response through antibiotics such as tetracycline and steroids such as Ledermix).
- stimulation of cemental healing (using enamel matrix proteins such as Emdogain).
- efforts to slow down an "inevitable" ankylosis (if the PDL has been destroyed and ankylosis is predictable, all the remaining PDL can be removed and Emdogain applied).
If a long-term inflammatory stimulus is present, RR will continue. Tumors, orthodontics and impaction, and a lack of vitality all provide such a stimulus. If the pressure is removed, resorption ceases. When dental trauma is significant and the pulp becomes nonvital, cemental damage is common. As mentioned above, toxins move through dentinal tubules, driving ERR. Endodontic therapy in these clinical cases removes such toxins. EIRR will not occur with a vital pulp. Root canal therapy can have a high degree of success in cases of IRR and EIRR, assuming that the periodontal status of the tooth is uncompromised and there is minimal risk of vertical fracture. Adequate root canal treatment controls intrapulpal bacteria and arrests the resorption process.
For teeth with closed apices, endodontic therapy should be started 7 days to 10 days after a severe injury that results in cemental damage and a necrotic tooth, and should ideally be finished in 1 day. If the case cannot be finished in one visit, calcium hydroxide should be placed and treatment finished within 1 month. Alternatively, calcium hydroxide can be placed for up to 6 months after starting treatment. If access has not been commenced within 10 days of the trauma or at the first observance of EIRR, calcium hydroxide should be placed and replaced as needed at 3-month intervals until the case is clinically ready for obturation. In the presence of established EIRR, long-term calcium hydroxide is preferable to short-term treatment.25
Cervical Inflammatory Resorption
Cervical inflammatory resorption (CIR) is a subclass of ERR. It is possible to have ERR below the epithelial attachment. In these clinical cases of CIR, the pulp is normal. Sulcular bacteria are suspected of providing the inflammatory stimuli that drive the process. Clinical management of this complex condition may be surgical, nonsurgical, or a combination of both modalities. It may also include orthodontic tooth movement or intentional replantation. It has been found that the treatment of cervical resorption is not as predictable if the process has progressed beyond the coronal third of the root.26
In invasive CIR, root canal therapy may not be absolutely necessary because the infection originates from the periodontal sulcus and initiates the pathological process. To adequately arrest the condition long-term, it is essential to remove the granulation tissue from the resorptive bay and seal the area. As a result, if the bacterial etiology can be removed and the pulp is vital then root canal therapy may not be necessary. However, often the granulation tissue cannot be removed comprehensively without traumatizing the pulp.
Teeth with CIR often have a questionable prognosis because of the periodontal and restorative needs that accompany this condition and the compromises that might occur to the long-term health of the periodontium as a result of the treatment. In addition, Class V restorations used to treat CIR are often traumatic to the pulp and lead to root canal therapy. Depending on the extent of the resorptive process, different treatment options have been proposed. Once perforation occurs then the success of retaining the tooth is dependent upon the severity of the defect. If the CIR is detected before perforation of the root, then conventional root canal therapy has a high rate of success. A crown-lengthening procedure can be considered if the area of resorption is not located too far subgingival (or subcrestal), which would affect the esthetics in addition to preventing restorative access. The long-term risk of vertical fracture, the time, costs, and numbers of procedures in addition to the long-term prognosis should be thoroughly reviewed before retaining these teeth. The patient should also be made aware of the long-term periodontal maintenance implications. If the clinician determines the tooth is nonrestorable then extraction with implant placement may be considered.
While not elaborated on here, it is noteworthy that there are a number of additional treatments for resorption that have been suggested in the literature, including calcitonin,27 Emdogain,24,28 and Alendronate (third-generation bisphosphonate in treating EIRR)29 (Figure 6, Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13, Figure 14 and Figure 15).
Conclusion
To summarize, the decision as to whether a questionable tooth should be removed and replaced by an implant versus conventional endodontic treatment and restorative therapy can be challenging even in otherwise common clinical scenarios, much less complex ones. A reliable set of clinical guidelines to direct treatment-planning choices benefits clinicians. Many criteria must be evaluated when treatment-planning a tooth that has sustained a traumatic event, including such tooth variables as periodontal status, restorative status, and endodontic involvement. Biomechanical considerations are especially important when extensive prosthetics are involved. Implant variables are associated with the potential implant site. Ridge morphology and bone density should be evaluated. Patient variables, including systemic health concerns, oral hygiene compliance, and financial limitations, also must be considered.
In addition, the correct diagnosis and management of the particular type of resorption present must be carried out for optimal tooth retention. Each case must be carefully assessed on its merits using the optimal equipment, materials, and clinical skills. All treatment of resorption should be considered against a backdrop of the alternative of extraction and implant placement. Certainly, the patient should be informed as to the prognosis, risks, costs, and alternatives at all times. The esthetics, function, and direct and indirect costs of each modality—tooth retention versus implant placement—should be equally considered before either one is recommended.
References
1. Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod. 2008;34(11):1302-1305.
2. Christensen GJ. Implant therapy versus endodontic therapy. J Am Dent Assoc. 2006;137(10):1440-1443.
3. Ozawa T, Yamazaki S, Tsuchida M, et al. Diagnostic reliability in dental limited cone-beam CT for root fractures. Japanese Journal of Conservative Dentistry. 2005;48(2):266-271.
4. American Dental Association. 2005 Survey of Dental Fees. Chicago, IL: American Dental Association; 2006:13-30.
5. Iqbal MK, Kim S. A review of factors influencing treatment planning decisions of single-tooth implants versus preserving natural teeth with nonsurgical endodontic therapy. J Endod. 2008;34(5):519-529.
6. Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004;15(6):348-381.
7. Kratchman SI. Endodontic microsurgery. Compend Contin Educ Dent. 2007;28(7):399-407.
8. Ne RF, Witherspoon DE, Gutmann JL. Tooth resorption. Quintessence Int. 1999;30(1):9-25.
9. Fuss Z, Tsesis I, Lin S. Root resorption—diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19(4):175-182.
10. Seibert JS. Reconstruction of deformed, partially edentulous ridges, using full thickness onlay grafts. Part I. Technique and wound healing. Compend Contin Educ Dent. 1983;4(5):437-453.
11. Spear F. A patient with a central incisor fractured apically in relation to the gingival margin. J Am Dent Assoc. 2009;140(3):355-359.
12. Argonin KJ, Kokich VG. Displacement of the glenoid fossa: a cephalometric evaluation of growth during treatment. Am J Orthod Dentofacial Orthop. 1987;91(1):42-48.
13. Shafer WG, Hine MK, Levy BM. A Textbook of Oral Pathology. 4th ed. Philadelphia, PA: W.B. Saunders; 1983.
14. Wedenberg C, Zetterqvist L. Internal resorption in human teeth—a histological, scanning electron microscopic, and enzyme histochemical study. J Endod. 1987;13(6):255-259.
15. Wedenburg C, Lindskog S. Experimental internal resorption in monkey teeth. Endod Dent Traumatol. 1985;1(6):221-227.
16. Frank AL, Torabinejad M. Diagnosis and treatment of extracanal invasive resorption. J Endod. 1998;24(7):500-504.
17. Gartner AH, Mack T, Somerlott RG, Walsh LC. Differential diagnosis of internal and external root resorption. J Endod. 1976;2(11):329-334.
18. Malueg LA, Wilcox L, Johnson W. Examination of external apical root resorption with scanning electron microscopy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;82(1):89-93.
19. Kaffe I, Tamse A, Littner MM, Schwartz I. A radiographic survey of apical root resorption in pulpless permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58(1):109-112.
20. Trope M. Luxation injuries and external root resorption—etiology, treatment, and prognosis. J Calif Dent Assoc. 2000;28(11):860-866.
21. Toto PD, Restarski JS. The histogenesis of pulpal odontoclasts. Oral Surg Oral Med Oral Pathol. 1963;16:172-178.
22. Donaldson M, Kinirons MJ. Factors affecting the onset of resorption in avulsed and replanted incisor teeth in children. Dent Traumatol. 2001;17(5):205-209.
23. Massler M, Malone AJ. Root resorption in human permanent teeth. A roentgenographic study. Amer J Orthod. 1954;40(8):619-633.
24. Trope M. Root resorption due to dental trauma. Endodontic Topics. 2002;1:79-100.
25. Trope M, Moshonov J, Nissan R, et al. Short vs. long-term calcium hydroxide treatment of established inflammatory root resorption in replanted dog teeth. Endod Dent Traumatol. 1995;11(3):124-128.
26. Heithersay GS. Treatment of invasive cervical resorption: an analysis of results using topical application of trichloracetic acid, curettage, and restoration. Quintessence Int. 1999;30(2):96-110.
27. Wiebkin OW, Cardaci SC, Heithersay GS, Pierce AM. Therapeutic delivery of calcitonin to inhibit external inflammatory root resorption. I. Diffusion kinetics of calitonin through the dental root. Endod Dent Traumatol. 1996;12(6):265-271.
28. Filippi A, Pohl Y, von Arx T. Treatment of replacement resorption with Emdogain—preliminary results after 10 months. Dent Traumatol. 2001;17(3):134-138.
29. Levin L, Bryson EC, Caplan D, Trope M. Effect of topical alendronate on root resorption on dried replanted dog teeth. Dent Traumatol. 2001;17(3):120-126.
About the Authors
Munib Derhalli, DMD, MS, MBA
Associate Clinical Professor
Department of Graduate Periodontics
Oregon Health Sciences University School of Dentistry
Portland, Oregon
Private Practice
Vancouver, Washington
Richard E. Mounce, DDS
Private Practice
Vancouver, Washington