You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Both evolutionary and revolutionary trends in dental materials science have been observed in the past decade. Among them has been an emphasis on the advancement of esthetic restorative materials. The characteristics or properties of an ideal restorative material are as follows1:
- It should be biocompatible. There should be no release of any byproducts during the chemical reactions of material hardening and, thereafter, no chemical leakage from the material.
- It should exhibit properties similar to those of enamel, dentin, and other tissues.
- It should be resistant to masticatory forces, wear (attrition and abrasion), and chemical insult (erosion) without fatiguing, and should provide heat insulation to vital tooth tissues from thermal changes.
- It should match the natural appearance of the surrounding tooth structure in shade, translucency, and texture.
- It should bond permanently to tooth structure, be easy to dispense and manipulate, and be capable of initiating tissue repair or regeneration of missing and damaged tissues.
Contemporarily, resin-based composite (RBC) materials are the most prominent esthetic restorative materials because of their universal usage, minimal loss of tooth structure, and ability to be directly placed without laboratory procedures. Advances in the resin materials and usage techniques have further allowed RBCs to fulfill almost all the ideal requisites of a restorative material. This article overviews currently available RBC materials and recent developments in RBC material science.
Evolution
During the early 20th century, silicates were the only material available for anterior teeth restorations. Acrylic resins, which offered such properties as tooth-like appearance, insolubility in oral fluids, ease of manipulation, and low cost, replaced the silicates, as silicate restorations showed dissolution in oral fluids.2,3 However, the excessive thermal expansion and contraction of acrylic resins caused stresses at the cavity margins, leading to early clinical failure.2 A major advance was made by Dr. Ray L. Bowen in 1962 through the development of bisphenol A glycidyl methacrylate (bis-GMA), a dimethacrylate resin, and an organic silane coupling agent to form a bond between the filler particles and the resin matrix.4 Later, light-activated RBCs and a UV-light cure unit (Nuva Light, DENTSPLY Caulk, www.caulk.com) were developed. In 1974, Foster and Walker introduced urethane dimethacrylate (UDMA), which has lower viscosity with a higher degree of conversion than bis-GMA.5 Early RBCs contained large (20 μm to 30 μm) spherical particles. These were followed by products containing large irregular shaped particles, fine particles (0.4 μm to 3 μm), microfine particles (0.04 μm to 0.2 μm), and, finally, blends (microhybrids) containing mostly fine particles with some microfine particles3 (Figure 1).
Later, RBCs were reinforced by incorporation of fibers or single crystals, or by addition of whiskers. Following this, materials having the combined properties of RBCs, glass-ionomer cement, and ceramics were formulated. Though nanofillers (such as colloidal silica filler particles) have been used for the past 30 years in the fabrication of RBCs, contemporarily nanofilled (containing a mixture of nanofillers and nanoclusters) and nanohybrid RBCs are being marketed by manufacturers as nanocomposites or nanoRBCs. More recently, materials based on epoxide chemistry (silorane monomers – oxirane + siloxane) have been made available. Every formulation and/or material has its own advantages and disadvantages as a restorative product. These are discussed in the following sections.
Composition
The structural components in RBCs consist of a matrix (forms continuous phase and binds the filler particles), filler particles (reinforcing particles and/or fibers), and a coupling agent (promotes adhesion between the filler and resin matrix). An initiator-accelerator system is added to bring about polymerization of the material. RBCs are typically classified based on the particle size, distribution, and composition of their inorganic filler particles2 (Figure 1). Another system of classification has been proposed by Jackson and Morgan6 on the basis of viscosity of materials that classifies RBCs as light-body composites (low viscosity), medium-body composites (medium viscosity), and heavy-body composites (high viscosity) (Figure 2).
Flowable RBCs
A modification of the small-particle-filled and hybrid RBCs has resulted in the so-called flowable RBCs.2 These are fabricated either by altering the filler level (reduced filler content) or by modifying the resin or silane technology, keeping the filler content similar to that of conventional hybrid RBCs. The consistency of these RBCs enables the material to flow readily, spread uniformly, and intimately adapt to the cavity form. They contain inorganic fillers with a particle size of 0.7 μm to 3.0 μm and filler loading of 42% to 53% by volume. Consequently, they have inferior physical properties such as lower wear resistance, strength, and radiopacity.7 These materials are speculated to show increased polymerization shrinkage compared to hybrid RBCs due to their higher resin content.8
Braga, Hilton, and Ferracane9 reported that flowable RBCs caused stress levels similar to nonflowable materials and did not produce significant stress reduction when used under nonflowable RBCs. Their use in conjunction with Class 2 resin restorations has demonstrated either similar or more cervical microleakage than when the RBCs are used without them. Flowable RBCs are usually indicated for the restoration of small Class I and Class V restorations, or as pit-and-fissure sealants, marginal repair materials, or, more infrequently, as the first increment placed as a liner under hybrid or packable RBCs. A pink color flowable RBC has been introduced to be used in Class V restorations to simulate gingival esthetics.
RBCs for Posterior Restorations
Posterior RBCs have shown an acceptable clinical performance with proper application of restorative techniques.10,11 They possess excellent resistance to wear with a low annual failure rate of 0% to 10%.12-16 The following modified RBCs are used primarily in the posterior region.
Packable RBCs—Because of their highly plastic composition in the pre-cured state, composites cannot be packed vertically into a cavity in such a way that the material flows both laterally and vertically to ensure intimate contact with the cavity walls. The development of packable RBCs is thus an attempt to accomplish two goals: easier restoration of a proximal contact; and handling properties similar to that of amalgam.17
The earlier term used for these RBCs was "condensable"; however, they are better described as "packable" because no real condensation occurs during placement. They generally have a chemically modified resin matrix with slightly higher filler content,18 and may have elongated, fibrous filler particles of about 100-μm length and/or textured surfaces that tend to interlock and resist flow. Their filler loading (fibers or porous or irregular particles) is 66% to 70% by volume.3
Packable RBCs feature less stickiness and stiffer consistency than conventional RBCs and a wear rate similar to that of amalgam. Because of increased viscosity and resistance to packing, some lateral displacement of the matrix band is possible, which allows for convenient placement and easier establishment of interproximal contacts in the posterior teeth. However, there is no clinical evidence that their properties (ie, strength and polymerization shrinkage) are better than those of conventional RBCs.19 A bulk-fill technique has been recommended20 but has not yet been demonstrated effective in clinical studies.21
Some commonly used posterior RBCs are Alert® (Jeneric/Pentron, www.pentron.com) (conventional barium borosilicate filler and "chopped" glass fibers), SureFil® (DENTSPLY Caulk) (multimodal fine, medium, and coarse particle-size distribution), Solitaire® 2 (Heraeus Kulzer, www.heraeus-dental-us.com) (porous filler particles with roughened external surfaces), and Filtek™ P60 (3M ESPE, www.3MESPE.com) (Zr/silica prepolymerized filler particles).22
Indirect posterior RBCs (laboratory RBCs)17,18,23—Crowns, inlays, veneers bonded to metal substructures, and metal-free bridges may be constructed indirectly from RBCs and processed in the laboratory using various combinations of light, heat, pressure, and vacuum to increase the degree of polymerization and wear resistance.18 These restorations are luted to the tooth with resin cements. The first generation of indirect RBC restorations suffered from low flexural strength, low modulus of elasticity, and low resistance to wear abrasion. Though a second generation of indirect RBCs are being promoted as a hybridization of composite and ceramic technologies,24 they have microsized filler particles and polyfunctional methacrylate monomers similar to conventional RBCs. They contain silanized ceramic fillers with mean particle sizes of less than 1 μm, with a narrow distribution of filler particles and high filler loading (70% to 80% by weight and 50% to 60% by volume) that helps to reduce the polymerization shrinkage and increase the modulus of elasticity. Also, they cause less abrasion of the natural dentition compared to ceramic restorations and can be easily repaired. Some of the commercially available indirect RBC products include Artglass (Heraeus Kulzer), BelleGlass HP (Kerr Corporation, www.kerrdental.com), Coltène Inlay System (Coltène Whaledent, www.coltene.com), Sculpture® (Jeneric/Pentron), and Targis (Ivoclar Vivadent, www.ivoclarvivadent.com).24
Nanocomposites or NanoRBCs
While not new to resin-based composite technology in dentistry, nanofillers feature filler particles in the size range of 1 nm to 100 nm (> 0.1 µm). Nanosized colloidal silica filler particles have been used for fabrication of optimal sized particle RBCs (eg, Esthet-X® HD, DENTSPLY Caulk; Herculite® Ultra, Kerr Corporation).18 The newer generations of nanoRBCs are basically nanohybrid RBCs, containing either a combination of nanofillers with nanoclusters or a combination of different types of filler particles, including nanofillers. The size of nanofillers used in RBCs is below the wavelength range for visible light (0.02 μm to 2 μm)25 and, thus, they do not produce light scattering or absorption. These RBCs have high filler loading, workable consistency, excellent polishability, as well as good handling, strength, and wear properties.25 However, due to extremely high surface area-to-volume ratio they require a higher degree of silanization than larger particulate fillers. One example is a contemporary, commercially available nanofilled product (Filtek™ Supreme, 3M ESPE) that contains a unique combination of nanofillers/nanomers (discrete non-agglomerated and non-aggregated particles) (5 nm to 75 nm) and nanoclusters (loosely bound agglomerates of nanosized particles) embedded in an organic polymer matrix. Another nanohybrid RBC (Ceram.X™ Mono/Duo, DENTSPLY DeTrey, www.dentsply.de) contains 62% volume of fillers, including glass fillers (~1 μm), nanofillers (~10 nm), and organically modified ceramic nanoparticles (2 nm to 3 nm).
Dresch et al26 reported that after 1 year nanofilled RBC showed similar performance as compared to other packable and microhybrid RBC. However, the nanoRBCs have shown poor resistance to staining as compared to hybrid RBCs.27 Thus, it is important to use this material judiciously in areas of esthetic concern, and frequent finishing and polishing of the restorations may be required on a regular-basis.
Fiber-Reinforced RBCs
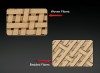
Fiber-reinforced RBCs consist of a reinforcing component, which provides strength and stiffness, and a surrounding matrix that offers support and enables workability. Generally, polyethylene, carbon fibers, or glass fibers are incorporated into the composite.17 The fibers may be arranged in various configurations; unidirectional fibers (long, continuous, and parallel) are the most popular, followed by braided and woven fibers (Figure 3). Most currently used fibers have diameters of 5 μm to 10 μm and effective lengths of 20 μm to 40 μm. They possess an adequate flexural modulus and flexural strength with excellent strength in the primary fiber direction.28 Orientation of fibers is found to have a significant effect on direction of shrinkage strain.29 For continuous unidirectional fiber composites, in which fibers run parallel and in one direction, properties are highest in the direction parallel to the fibers and lowest in the direction perpendicular to the fibers (anisotropic properties [properties dependent on the direction of fiber orientation]). Conversely, bidirectional fibers (weaves) give orthotropic properties (properties independent of direction within each plane) for the material in plane, and randomly oriented fibers (chopped fibers) give isotropic properties (same properties regardless of the direction in which they are tested) in plane or even 3-dimensionally.30
Typically, it is difficult to efficiently pack the fibers or orient their direction,25 leading to heterogeneous and anisotropic properties of fiber-reinforced RBCs. Other shortcomings of fiber-reinforced RBCs are surface degradation of the initial polish, high wear rates, high levels of post-insertion sensitivity and delamination from the fiber-reinforcing substructure. Their main applications are in dental splints, reinforced composite structures and root posts, reinforcement of denture bases, fixed partial dentures, and reinforced biomedical implants.
Chopped glass fibers have also been used as fillers for dental resins.31 Recently, branched-fiber fillers, in which each filler particle consists of a porous network of fibers, have been incorporated into RBCs and cements.32 Single crystals featuring symmetric shape as long plates are also being used; they are much stronger than noncrystalline or polycrystalline fibers.33 Unfortunately, the crystals are colored and not well suited for esthetic compositions.
Whisker-Reinforced RBCs
Silica-fused ceramic whiskers (0.1 µm to 2 µm in diameter and 2 µm to 30 µm in length) are used to reinforce dental RBCs.33,34 Silica particles are thermally fused onto the whiskers (silica nitride or carbide) to facilitate silanization, minimize whisker entanglement, and enhance whisker retention in the resin matrix by roughening the whisker surfaces. The whiskers are highly elongated, making them effective in bridging microcracks, preventing crack propagation, and resisting dislodgement from the matrix during wear. More suitable for contact and wear applications, whisker RBCs have relatively isotropic and homogeneous properties. They also possess high strength and fracture resistance.34,35 Silicon-nitride whiskers have shown to increase the strength and toughness of RBC more than the silicon-carbide whiskers. The main problem with whisker-reinforced RBCs is desilanization of whiskers.
Polyacid-Modified RBCs (Compomers)
Formulated without water, compomers contain polyacid-modified monomers with fluoride-releasing silicate glasses. These materials have two main constituents: dimethacrylate monomer(s) with two carboxylic groups present in their structure; and filler that is similar to the ion-leachable glass present in glass-ionomer cements (GICs).36 The ion-leachable glass is partially silanized to ensure some bonding with the matrix. The liquid portion of compomers contains polyacrylic acid along with water and visible light-activated monomers. The volume percent filler ranges from 42% to 67%, and the average filler particle size ranges from 0.8 μm to 5.0 μm.3
Setting occurs primarily by light-cured polymerization, but an acid-base reaction also occurs as the compomer absorbs water after placement and upon contact with saliva. Curing continues for approximately 24 hours. Compomers release fluoride by a mechanism similar to that of glass and hybrid ionomers, but the amount of fluoride release and its duration are lower than those of glass and hybrid ionomers. Also, compomers do not get recharged from fluoride treatments. Compared to conventional RBCs, compomers possess lower flexural modulus of elasticity, compressive strength, flexural strength, fracture toughness, and hardness.36,37 They also show excessive water sorption. Bonded to tooth structure using accompanying bonding agents,38 compomers are used for restorations in low stress-bearing areas and for patients at medium risk of developing caries, or when employing sandwich technique.
Organically Modified Ceramics (Ormocer)
Ormocers are a packable restorative material that contains a novel inorganic-organic copolymer matrix based on multifunctional urethane- and thioether (meth)-acrylate alkoxysilanes.22 The intraoral curing of an ormocer-based restorative material is achieved by radical-induced polymerization of the attached (meth)-acrylate groups. Ormocers do not release any detectable residual substances, show reduced polymerization shrinkage (1.88%), and have high abrasion resistance.22 Cattani-Lorente et al (2001)39 found that the shrinkage of ormocer was equal to that of hybrid composites despite having less filler content. Annual failure rates for this material range between 0% and 12.7%.13
Giomer
Representing a true hybridization of glass ionomer and RBCs, giomer restoratives have the fluoride-release and recharge properties of glass-ionomer cements along with the excellent esthetics, easy polishability, and strength of RBCs. The composition of giomers is based on PRG (pre-reacted glass ionomer) technology,40,41 which involves the pre-reaction of fluoro-aluminosilicate glass fillers with polyacrylic acid, forming a stable phase glass ionomer described as "wet siliceous hydrogel." The resulting glass ionomer is then freeze-dried, milled, silane-treated, and ground to form the PRG fillers, followed by their incorporation into a resin matrix. PRG technology is classified into two categories: F-PRG (full reaction type), whereby the entire filler particle is attacked by polyacrylic acid; and S-PRG (surface reaction type), in which only the surface of the glass filler is attacked by polyacrylic acid and a glass core remains. S-PRG giomer is indicated for Class I through Class VI cavities; F-PRG is indicated in cervical cavities.41 Sunico et al42 observed that the success rate for S-PRG cervical restorations after two years was 80%, while the success rate for F-PRG cervical restorations was 71%.
Giomers offer increased wear resistance, high radiopacity and shade conformity, and a high and sustained level of fluoride release and recharge. Yap et al43 found that while giomer released fluoride, it did not have an initial "burst" type of release like glass ionomers, and long-term fluoride release (ie, 28-day) was lower than that of the other materials. Like compomers, giomers are light-polymerized and require bonding systems for adhesion to tooth structure.
RBCs with Antibacterial Properties
Yet another innovation in composite resins is to produce materials with anticariogenic properties.44 Different monomer systems have been formulated to achieve this goal, but most of these materials are not commercially available and still have to reach the markets.
Incorporation of chlorhexidine—One approach to prevent plaque accumulation on and around RBC fillings is by incorporating an antibacterial agent such as chlorhexidine compounds into the resin matrix. These experimental materials exhibit antibacterial activity by releasing the chlorhexidine but have shown to possess inferior mechanical properties.45,46
Anti-cariogenic monomer systems—A promising monomer with antibacterial properties is methacryloyloxydodecylpyridinium bromide (MDPB). It is a compound of antibacterial agent dodecylpyridinium bromide and a methacrylyl group. Bis-GMA-based RBC incorporating MDPB has been shown to have an inhibitory effect on surface growth of Streptococcus mutans with no adverse effects on curing or mechanical properties.47,48
Fluoride-releasing RBCs—Flouride49 has been incorporated into a variety of dental materials. Fluoride-releasing RBCs have high strength, good wear resistance, and excellent esthetics, but they release only a small amount of fluoride and have low fluoride-recharge capabilities. Initially, soluble-free salts such as sodium fluoride (NaF), potassium fluoride (KF), strontium fluoride (SrF2), or stannous fluoride (SnF2) were added to sealants and RBCs50 that released fluoride when water diffused through the matrix and dissolved these salts.44 Following this, fluoride-releasing glass fillers such as fluoroaluminosilicate glass or sparingly soluble inorganic salts (Ytterbium[III] fluoride [YbF3]) were used in fluoride-releasing RBCs.44,51 Other fluoride-releasing formulations include acrylic–amine boron trifluoride (BF3) Lewis salt that can copolymerize with Bis-GMA resins,52 methacrylyl fluoride monomers,42,53 and monomers containing an anion-exchangeable fluoride moiety (t-butylaminoethyl methacrylate hydrogen fluoride or morpholinoethyl methacrylate hydrofluoride).44,54 The amine-hydrofluoride-based monomers are capable of sustained fluoride release and recharge but have relatively short shelf life. More recently, a fluoride-releasing dimethacrylate monomer containing a ternary zirconium fluoride has been formulated.55
Smart RBCs
The term "smart materials" refers to a class of materials that are highly responsive and react to changes in environmental variables such as temperature, moisture, pH, or electric and magnetic fields.56 In dentistry these materials are classified on the basis of their fluoride-releasing capacity as "active" and "passive" smart materials.57 Passive smart materials are those that release fluoride ions as the pH of oral fluids decreases, but the release continues above a pH of 5.5, whereas active smart materials tend to release fluoride ions as the pH of oral fluids decreases below 5.5 but terminate the release of fluoride when the pH rises above 5.5.
Ariston pHc (Ariston pHc alkaline glass restorative)—Ariston pHc (pH control) claimed to release fluoride, hydroxide, and calcium ions and is recommended for Class I and II restorations.22,58 But due to poor clinical performance it has been withdrawn from the market.
Amorphous calcium phosphate (ACP)-containing composite59,60—At neutral low pH values (5.8 or below), as occur during a carious attack, amorphous calcium phosphate (ACP) converts into hydroxyapatite (HAP) and precipitates, thus replacing the HAP lost to the acid. Also, once the calcium phosphate is released, it acts to neutralize the acid and buffer the pH (Figure 4). It has been observed that biaxial flexure strength, diametral tensile strength, and compressive strength of ACP-containing RBCs is lower than that of conventional RBCs, and, therefore, they are mechanically weaker than other polymeric RBCs.61 ACP in combination with casein phosphopeptide (ACP-CPP) is available commercially as dentifrices and chewing gums. But ACP-containing RBCs have not been marketed thus far.
Low-Shrinkage RBCs
Various materials have been developed, tested, and tried for the purpose of minimizing the polymerization shrinkage and associated stresses of RBCs. One of the earlier developments includes the introduction of eutectic monomer systems such as bis (2-methacrylyloxyethyl) esters of phthalic (MEP), isophthalic (MEL), and terephthalic acids (MET)62 and the use of liquid crystalline monomers that shrink less when photocured.63 Bicyclic ring-opening monomers like spiro-orthocarbonate (SOC) were developed that exhibit homopolymerization via double spiro-cyclic ring opening, resulting in no shrinkage or even expansion on polymerization.64
SOCs with decreased melting points and containing additional alicyclic rings fused to the SOC body have also been investigated. These SOCs, however, have significantly less reactivity than methacrylate resins, resulting in decreased cross-linking leading to inferior mechanical properties.64 Epoxy-based monomers exhibiting a significantly reduced shrinkage on polymerization have also been tried. However, the experimental epoxy-based RBC shows a decreased degree of conversion within the first hour following irradiation, which may compromise the flexure strength of the material.65 Low-shrink experimental oxirane RBCs (EXL596 and H1) have also been tested that have decreased wear resistance compared to methacrylate-based RBCs.66 The most recent additions to this RBC category are silorane-based RBCs.
Silorane-based RBCs
Silorane monomers are silicon-based monomers with oxirane functionality that are derived from the combination of siloxanes and oxiranes. The network of siloranes is generated by the cationic ring-opening polymerization (ROP) of the cycloaliphatic oxirane moieties. These cationic ROP-based silorane RBCs have low volumetric shrinkage and, thus, resultant low polymerization stresses.67 Because of the hydrophobic nature of the resin, no oxygen inhibition layer is formed68 and better chemical stability in an aqueous environment is provided. A reduced adherence of oral streptococci to these RBCs has also been observed.69 In vitro microleakage, polishability, color stability, and gloss retention of silorane RBCs is superior to that of conventional composites.68,70 They also show decreased water sorption and solubility.71
A low-shrink posterior restorative introduced in the US market that is based on silorane chemistry is claimed to shrink less than 1% and reduce polymerization stresses by up to 80% while providing excellent marginal integrity; however, more in vivo studies are required in order to comment on its clinical performance. Moreover, it must be used with a two-step self-etching bonding system for optimal bonding.
Self-Adhering (Self-Etch) RBCs
Recently, a new type of RBC has been manufactured by effectively fusing together the self-adhesive bonding agent and the resin-based composite restorative technology. These self-adhering (self-etch) RBCs can bond to both dentin and enamel without the use of a separate adhesive/bonding system, thus reducing the chances of postoperative sensitivity and allowing for a faster restoration that can save operators time and patients money. As per manufacturers' claims, they possess high bond strengths to dentin and enamel and are easy to handle.
The first commercially available self-adhesive flowable RBC that etches, primes, bonds, and restores using only one product has been developed. Able to be used alone or together with other bonded RBCs, the product is formulated by combining 4-methacryloxyethyl trimellitic acid (4-MET) technology with a new proprietary BPA-free resin. Available in A1, A2, A3, and B1 shade, the RBC is indicated for restoring small Class I, Class III, and Class V carious lesions; as pit-and-fissure sealant; for blocking out undercuts; and as a base liner. Another commercially available self-adhering RBC incorporates a bonding agent into a flowable RBC.
In vitro and in vivo clinical studies of self-adhering RBCs approving of their use as a potential restorative material are, however, still lacking.
Other Uses of RBCs
RBC core materials (eg, Ti-Core Auto E, Essential Dental Systems, Inc., www.edsdental.com; ParaPost® ParaCore, Coltène Whaledent; CompCore™ AF, Premier Dental, www.premusa.com; Build-It® FR™, Pentron) are typically two-paste self-cured and/or dual-cured composites and are usually tinted (blue, white, or opaque) to provide a contrasting color.17,18 RBC cores have high rigidity, are easy to contour, are bonded to dentin, and can be finished immediately. For core buildup on a fiber post, dual-cure RBCs appear to be preferable to light-cured RBCs.72 RBCs are also being used for the fabrication of temporary/provisional inlays, crowns, and long-span bridges.18 Microfilled RBCs are being used as resin-veneering materials, which are polymerized by using either visible light or by a combination of heat and pressure.17 Resin cements that are used as luting agents are filled to a lesser degree than hybrids and possess properties approximating that of flowable RBCs.
Conclusion
The search for an ideal direct esthetic restorative material is still ongoing. Among the array of RBC materials, some are readily available in the market (flowable, packable, and fiber-reinforced), others have just recently been introduced (siloranes-based), and a few are still in development phase (fluoride-releasing). Individual properties of different RBC materials define their advantages, disadvantages, and clinical uses. Each type of RBC material has its own virtues in some clinical aspects and shortcomings in other aspects. Every material possesses either one or the other ideal properties of a restorative material, but not all of them. Therefore, it is important for a clinician to use every material judiciously and for a clinical application for which it is best suited (Figure 5, Figure 6, Figure 7, Figure 8, Figure 9 and Figure 10).
The use of RBC restorations is increasing because of the benefits accrued from the development of material technology, improved adhesive bonding, esthetic qualities, and universal clinical usage. Because of the introduction of an array of newer products with improved characteristics, RBC restorations can provide excellent service for many years. Due to the materials' technique sensitivity and individuality, operators are cautioned to use and work with them carefully, so as to achieve long-term success in their clinical practice.
References
1. Anusavice KJ. Overview of materials for dental applications. In: Anusavice KJ, ed. Phillips' Science of Dental Materials. 11th ed. St. Louis, MO: Saunders: 2003:3-20.
2. Rawls RH, Esquivel-Upshaw JF. Restorative resins. In: Anusavice KJ, ed. Phillips' Science of Dental Materials. 11th ed. St. Louis, MO: Saunders: 2003:399-442.
3. Resin composite restorative materials. In: Powers JM, Sakaguchi RL, eds. Craig's Restorative Dental Materials. 12th ed. St. Louis, MO: Mosby; 2007:189-192.
4. Bowen RL, inventor. Dental filling material comprising vinyl-silane treated fused silica and a binder consisting of the reaction product of bis-phenol and glycidyl acrylate. US patent 3,06,112. November 27, 1962.
5. Rawls RH. Dental polymers. In: Anusavice KJ, ed. Phillips' Science of Dental Materials. 11th ed. St. Louis, MO: Saunders: 2003:143-169.
6. Jackson RD, Morgan M. The new posterior resins and a simplified placement technique. J Am Dent Assoc. 2000;131(3):375-383.
7. Hilton TJ. Direct posterior esthetic restorations. In: Summitt JB, Robbins JW, Schwartz RS, Santos JD, eds. Fundamentals of Operative Dentistry. 2nd ed. Hanover Park, IL: Quintessence Publishing; 2001:260-305.
8. Labella R, Lambrechts P, Van Meerbeek B, et al. Polymerization shrinkage and elasticity of flowable composites and filled adhesives. Dent Mater. 1999;15(2):128-137.
9. Braga RR, Hilton TJ, Ferracane JL. Contraction stress of flowable composite materials and their efficacy as stress-relieving layers. J Am Dent Assoc. 2003;134(6):721-728.
10. Kiremitci A, Alpaslan T, Gurgan S. Six-year clinical evaluation of packable composite restorations. Oper Dent. 2009;34(1):11-17.
11. Türkün LS, Türkün M, Ozata F. Two-year clinical evaluation of a packable resin-based composite. J Am Dent Assoc. 2003;134(9):1205-1212.
12. Bernardo M, Luis H, Martin MD, et al. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J Am Dent Assoc. 2007;138(6):775-783.
13. Manhart J, Chen H, Hamm G, et al. Buonocore Memorial Lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent. 2004;29(5):481-508.
14. Opdam NJ, Bronkhorst EM, Roeters JM, et al. Longevity and reasons for failure of sandwich and total-etch posterior composite resin restorations. J Adhes Dent. 2007;9(5):469-475.
15. Leinfelder KF, Wilder AD Jr, Teixeira LC. Wear rates of posterior composite resins. J Am Dent Assoc. 1986;112(6):829-833.
16. Suzuki S, Suzuki SH, Cox CF. Evaluating the antagonistic wear of restorative materials when placed against human enamel. J Am Dent Assoc. 1996;127(1):74-80.
17. Roberson TM, Heymann HO, Ritter AV. Introduction to composite restorations. In: Roberson TM, Heymann HO, Ritter AV, eds. Sturdevant's Art and Science of Operative Dentistry. 4th ed. St. Louis, MO; Mosby Publishing; 2002:471-500.
18. Wakefield CW, Kofford KR. Advances in restorative materials. Dent Clin North Am. 2001;45(1):7-29.
19. Leinfelder KF, Bayne SC, Swift EJ Jr. Packable composites: overview and technical considerations. J Esthet Dent. 1999;11(5):234-249.
20. Sarrett DC, Brooks CN, Rose JT. Clinical performance evaluation of a packable posterior composite in bulk-cured restorations. J Am Dent Assoc. 2006;137(1):71-80.
21. Bingham V. Comparative depth of cure using two factors: Composite system and curing time [abstract]. Taken from: J Dent Res. 2000;79:1518A.
22. Combe EC, Burke FJ. Contemporary resin-based composite materials for direct placement restorations: packables, flowables and others. Dent Update. 2000;27(7):326-336.
23. Leinfelder KF. New developments in resin restorative systems. J Am Dent Assoc. 1997;128(5):573-581.
24. Nash R. Composite resin: indirect technique restorations. In: Aschheim KW, Dale BG, eds. Esthetic Dentistry: A Clinical Approach to Techniques and Materials. 2nd ed. St. Louis, MO: Mosby Publishing; 2001:97-112.
25. Bayne SC, Thompson JY, Taylor DF. Dental materials. In: Roberson TM, Heymann HO, Ritter AV, eds. Sturdevant's Art and Science of Operative Dentistry. 4th ed. St. Louis, MO; Mosby Publishing; 2002:136-234.
26. Dresch W, Volpato S, Gomes JC, et al. Clinical evaluation of a nanofilled composite in posterior teeth: 12-month results. Oper Dent. 2006;31(4):409-417.
27. Yazici AR, Çelik Ç, Dayangaç B, et al. The effect of curing units and staining solutions on the color stability of resin composites. Oper Dent. 2007;32(6):616-622.
28. Dyer SR, Lassila LV, Jokien M, et al. Effect of fiber position and orientation on fracture load of fiber-reinforced composite. Dent Mater. 2004;20(10):947-955.
29. Tezvergil A, Lassila LV, Vallittu PK. The effect of fiber orientation on the polymerization shrinkage strain of fiber-reinforced composites. Dent Mater. 2006;22(7):610-616.
30. Nielsen LE. Mechanical properties of polymer and composites. 1st ed. New York, NY: Marcel Dekker Inc; 1974:468-488.
31. Krause WR, Park SH, Straup RA. Mechanical properties of BIS-GMA resin short glass fiber composites. J Biomed Mater Res. 1989;23(10):1195-1211.
32. Swift EJ Jr, Thompson JY, Bayne SC. Review of dental materials citations: Part B, July to December 1995. Dent Mater. 1996;12(2):127-141.
33. Xu HH. Dental composite resins containing silica-fused ceramic single-crystalline whiskers with various filler levels. J Dent Res. 1999;78(7):1304-1311.
34. Xu HH, Martin TA, Antonucci JM, et al. Ceramic whisker reinforcement of dental resin composites. J Dent Res. 1999;78(2):706-712.
35. Xu HH, Quinn JB, Smith DT, et al. Effects of different whiskers on the reinforcement of dental resin composites. Dent Mater. 2003;19(5):359-367.
36. Ruse ND. What Is a "Compomer"? J Can Dent Assoc. 1999;65(9):500-504.
37. Meyer JM, Cattani-Lorente MA, Dupuis V. Compomers: between glass-ionomer cements and composites. Biomaterials. 1998;19(6):529-539.
38. Martin R, Paul SJ, Luthy H, et al. Dentin bond strength of Dyract Cem. Am J Dent. 1997;10(1):27-31.
39. Cattani-Lorente M, Bouillaguet S, Godin CH, et al. Polymerization shrinkage of Ormocer based dental restorative composites. Eur Cell Mater. 2001;1(1):25-26.
40. Teranaka T, Okada S, Hanaoka K. Diffusion of fluoride ion from GIOMER products into dentin. Paper presented at: 2nd GIOMER International Meeting; July 1, 2001; Tokyo, Japan.
41. Gordan VV, Mondragon E, Watson RE, et al. A clinical evaluation of a self-etching primer and a giomer restorative material. J Am Dent Assoc. 2007;138(5): 621-627.
42. Sunico MC, Shinkai K, Katoh Y. Two-year clinical performance of occlusal and cervical giomer restorations. Oper Dent. 2005;30(3):282-289.
43. Yap AU, Tham SY, Zhu LY, et al. Short-term fluoride release from various esthetic restorative materials. Oper Dent. 2002;27(3):259-265.
44. Peutzfeldt A. Resin composites in dentistry: the monomer systems. Eur J Oral Sci. 1997;105(2):97-116.
45. Ribeiro J, Ericson D. In vitro antibacterial effect of chlorhexidine added to glass-ionomer cements. Scand J Dent Res. 1991;99(6):533-540.
46. Jedrychowski JR, Caputo AA, Kerper S. Antibacterial and mechanical properties of restorative materials combined with chlorhexidine. J Oral Rehabil. 1981;10(5):373-381.
47. Imazato S, Torii M, Tsuchitani Y, et al. Incorporation of bacterial inhibitor into resin composite. J Dent Res. 1994:73(8):1437-1443.
48. Imazato S, McCabe JF. Influence of incorporation of antibacterial monomer on curing behavior of a dental composite. J Dent Res. 1994;73(10):1641-1645.
49. ten Cate JM, Duijsters PP. Influence of fluoride in solution on tooth demineralization. II. Microradiographic data. Caries Res. 1983;17(6):513-519.
50. Temin SC, Csuros Z. Long-term fluoride release from a composite restorative. Dent Mater. 1988;4(4):184-186.
51. Dijkman GE, Arends J. Secondary caries in situ around fluoride-releasing light-curing composites: a quantitative model investigation on four materials with fluoride content between 0 and 26 vol %. Caries Res. 1992;26(5):351-357.
52. O'Connell JJ, Kwan SC, inventors. Fluoride-containing dental materials. US patent 4,772,325. September 20, 1988.
53. Kadoma Y, Masuhara E, Anderson JM. Controlled release of fluoride ions from methacryloyl fluoride-methyl metha acrylate copolymers. 2. Solution, hydrolysis and release of fluoride ions. Macromolecules. 1982;15(4):1119-1123.
54. Rawls HR. Fluoride releasing acrylics. J Biomater Appl. 1987;1(3):382-405.
55. Xu X, Ling L, Wang R, et al. Formulation and characterization of a novel fluoride-releasing dental composite. Dent Mater. 2006;22
(11):1014-1023.
56. Gautam P, Valiathan A. Bio-smart dentistry: Stepping into the future! Trends Biomater Artif Organs. 2008;21(2):94-97.
57. Bharadwaj TPN, Kachana RS, Parameswaran A. Smart materials in dental restoratives. Trends Biomater Artif Organs. 2003;17(1):3-7.
58. Kukletovám M, Kuklová J, Christoforidis G. Ariston pHc restorative material: Clinical and morhpological study. Scripta Medica. 2003;76(1):39-48.
59. Skrtic D, Antonucci JM, Eanes ED. Amorphous calcium phosphate-based bioactive polymeric composites for mineralized tissue regeneration. J Res Natl Inst Stand Technol. 2003;108:167-182.
60. Skrtic D, Antonucci JM, Eanes ED, Eidelman N. Dental composites based on hybrid and surface-modified amorphous calcium phosphates. Biomaterials. 2004;25(7-8):1141-1150.
61. Park MS, Eanes ED, Antonucci JM, Skrtic D. Mechanical properties of bioactive amorphous calcium phosphate/methacrylate composites. Dent Mater. 1998;14(2):137-141.
62. Bowen RL. Crystalline dimethacrylate monomers. J Dent Res. 1970;49(4):810-815.
63. Satsangi N, Rawls HR, Norling BK. Synthesis of low-shrinkage polymerizable methacrylate liquid-crystal monomers. J Biomed Mater Res B Appl Biomater. 2005;74(2):706-711.
64. Palin WM, Fleming GJ. Low-shrink monomers for dental restorations. Dent Update. 2003;30(3):118-122.
65. Palin WM, Fleming GJ, Burke FJ, et al. Monomer conversion versus flexural strength of a novel dental composite. J Dent. 2003;31(5):341-351.
66. Palin WM, Fleming GJ, Burke FJ, et al. The frictional coefficients and associated wear resistance of novel low-shrink resin-based composites. Dent Mater. 2005;21(12):1111-1118.
67. Guggenberger R, Weinmann W. Exploring beyond methacrylates. Am J Dent. 2000;13(spec no):82D-84D.
68. Duarte S Jr, Botta AC, Phark JH, Sadan A. Selected mechanical and physical properties and clinical applicaton of a new low-shrinkage composite restoration. Quintessence Int. 2009;40(8):631-638.
69. Buergers R, Schneider-Brachert W, Hahnel S, et al. Streptococcal adhesion to novel low-shrink silorane-based restorative. Dent Mater. 2009;25(2):269-275.
70. Bagis YH, Baltacioglu IH, Kahyaogullari S. Comparing microleakage and the layering methods of silorane-based resin composite in wide Class II MOD cavities. Oper Dent. 2009;34(5):578-585.
71. Palin WM, Fleming GJ, Burke FJ, et al. The influence of short and medium-term water immersion on the hydrolytic stability of novel low-shrink dental composites. Dent Mater 2005; 21(9):852-863.
72. Salameh Z, Papacchini F, Ounsi HF, et al. Adhesion between prefabricated fiber-reinforced posts and different composite resin cores: a microtensile bond strength evaluation. J Adhes Dent. 2006;8(2):113-117.
About the Authors
Neeraj Malhotra, MDS, PGDHHM
Assistant Professor
Department of Conservative Dentistry and Endodontics
Manipal College of Dental Sciences
Manipal University
Mangalore, India
Kundabala Mala, MDS
Professor
Department of Conservative Dentistry and Endodontics
Manipal College of Dental Sciences
Manipal University
Mangalore, India
Shashirashmi Acharya, MDS
Professor
Department of Conservative Dentistry and Endodontics
Manipal College of Dental Sciences
Manipal University
Manipal, India