You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
When discussing implant placement in premolar and molar areas, it is important to note that such therapy cannot be appropriately executed unless done so within the context of a comprehensive diagnosis and case work-up, with the development of a multi-disciplinary treatment plan. The cornerstones of such an approach are a thorough examination, appropriate radiographs and models as necessary, and a willingness to listen to the patient, thus better ascertaining his or her needs and desires.
When contemplating removal of a premolar or molar and its replacement with an implant-supported prosthesis, the clinician must first consider the feasibility of other potentially less “aggressive” treatment approaches. While specific clinical scenarios, including extensive caries, tooth or root fracture, root resorption, endodontic perforation, or other concerns, will mandate tooth removal, the loss of supporting bone and attachment apparatus due to periodontal disease, with or without concomitant furcation involvement, is not an absolute indication for tooth extraction. Proven treatment modalities exist, whether they be resective, regenerative, or a combination of the two, by which periodontally involved teeth can be successfully treated.
However, such treatment decisions must be made in the context of an appropriate definition of therapeutic success. Successful periodontal therapy is not characterized by short-term clinical health and immediate gratification. Rather, the net result of successful periodontal therapy should be an ease of patient maintenance, long-term predictability, and tooth retention in a healthy state for as long as possible. Predictability is defined as stable attachment levels, and having no continued loss of supporting bone or periodontal attachment.
Naturally, specific patient considerations impact the definition of success. If a patient of advanced age, or one with a medical status that contraindicates specific therapies, is to be treated, a more compromised definition of success must often be accepted. Nevertheless, all medical contraindications to therapy and actuarial considerations will be ignored for the purposes of this discussion.
Furcation Involvements
Furcation involvements represent a unique and challenging area of potential increased plaque accumulation and, hence, rapid periodontal breakdown. A sampling of literature underscores the inadequacy of most therapies in the “maintenance” of periodontal health around invaded furcations, without elimination of the aforementioned furcation involvement. Becker et al,1 in a longitudinal study of patients who refused active periodontal therapy but remained under continued maintenance care, reported an overall rate of tooth loss of 9.8% in the mandible and 11.4% in the maxilla. Mandibular furcated teeth were lost at a rate of 22.5%, while maxillary furcated teeth were lost at a 17% rate.
This pattern of teeth with furcation involvements being less amenable to “maintenance care” than their single-rooted counterparts is confirmed by Goldman et al,2 who assessed tooth loss in 211 patients treated in a private periodontal practice through root planing, curettage, and open flap debridement, and maintained for 15 to 30 years on a consistent recall schedule. Furcation involvements were not eliminated. The overall rate of tooth loss was 13.4%. Maxillary and mandibular teeth with furcation involvements were lost at a rate of 30.7% and 24.2%, respectively, a rate that was higher than the incidence of non-furcated tooth loss.
McFall,3 reporting on tooth loss in 100 treated patients with periodontal disease maintained for 15 years or longer following active therapy, noted loss of maxillary and mandibular teeth with furcation involvements at rates of 22.3% and 14.7%, respectively. Similar findings have been consistently reported in the literature.4-6
A study by Fleisher et al7 underscores the extreme difficulty in performing total debridement of a periodontally involved furcation. Fifty molars were treated through closed curettage or open flap debridement, and were then extracted and stained to assess the efficacy of debridement. Only 68% of the tooth surfaces facing the involved furcations were calculus-free. Although the use of microscopy and newer instrumentation greatly improves the clinician’s ability to thoroughly debride involved furcations, such debridement does not eliminate the furcation involvement itself, which represents a harbor for plaque. While debridement may “slow down” the rate of progression of periodontal disease in the involved furcation, it is not a desired treatment endpoint in most clinical situations. The furcation must be eliminated, thus providing the patient with a milieu amenable to appropriate plaque control efforts.
Cemento-enamel projections prevent the establishment of connective tissue attachment to the root surface, as connective tissue attachment to enamel does not predictably occur. As a result, cemento-enamel projections represent a potential compromise in periodontal heath and treatment outcomes. While a Class I cemento-enamel projection, which extends less than 25% of the root trunk toward the furcation entrance, poses little concern, Class II (extending more than 50% of the dimension of the root trunk toward the furcation entrance) or Class III (extending to or into the entrance to the furcation) cemento-enamel projections must be eliminated if the appropriate attachment apparatus is to be re-established to protect the furcation entrance.
Class I furcation involvements may not always be eliminated through ondontoplasty. If the bone loss in the area of the Class I furcation involvement has a vertical component that extends to such an extent that positive architecture may not be developed, the problems in this region cannot be resolved in such a manner. Such developments are rare with Class I furcation involvements. The roof of the furcation is recontoured to eliminate the cul de sac that traps plaque, and the newly established tooth contours are carried onto the radicular surfaces of the tooth to create a continuous, smooth morphology conducive to patient plaque control efforts. Osseous resection with apically positioned flaps is performed at the same time in the conventional manner. The result of treatment is elimination of both deeper pocket depths and Class I furcation involvements. When such therapy has been performed, success is defined as there being no entrance of the probe into the furcation of the tooth, and no probing depths in excess of 3 mm around the tooth. Coincident to the ondontoplasty is the elimination of all cemento-enamel projections, thus enhancing the ability to form an appropriate attachment apparatus to protect the furcal entrance. Such ondontoplasty is highly predictable and may be carried out without a prosthetic commitment. If early furcation involvements are not eliminated through ondontoplasty, continued periodontal breakdown and attachment loss in the furcation area will occur, resulting in an untreatable situation and eventual tooth loss.
Such aggressive treatment of Class I furcation involvements is conservative therapy. For example, if a 25-year-old patient presents with excellent home care, minimal probing depths, and a Class III cemento-enamel projection in the buccal furcation area of a lower first molar as evidenced by examination following retraction of unattached soft tissues in this area, the clinician must make a decision between two treatment approaches: 1) The patient could be placed on a strict maintenance schedule, and the clinician could attempt to “maintain” the furcation in question through repeated professional prophylaxis visits. This approach may appear to offer advantages to the patient; however, the net result of such a “treatment” approach will be progression of periodontal disease in the furcation area, periodontal attachment loss, and/or development of a furcation involvement. 2) A flap may be reflected and ondontoplasty performed to eliminate the cemento-enamel projection and any early furcation involvements that have developed. The result of such a treatment will be elimination of anatomical factors contributing to periodontal breakdown in the furcation area, the development of an appropriate attachment apparatus, and establishment of appropriate hard- and soft-tissue morphologies that are conducive to home care efforts.
Timely intervention is crucial when faced with Class I furcation involvements and/or Class III cemento-enamel projections, so as to preserve the alveolar bone and attachment apparatus on the tooth and eliminate the need for more aggressive therapies later. Such an interceptive approach predictably eliminates a furcation at an early stage, resulting in periodontal health and tooth retention with a minimal amount of therapy. Failure to diagnose and treat Class I furcations will result in the need for more aggressive, less predictable periodontal therapy, or tooth removal and replacement.
Class II furcation involvements may not be eliminated through ondontoplasty, as such tooth recontouring would result in a tooth morphology that is deeply notched and not conducive to plaque control efforts. If a tooth with a Class II furcation involvement is to be maintained, regenerative techniques employing membranes, graft materials, growth factors, or other substances must be employed. It is not within the purview of this discussion to review regenerative options when faced with Class II furcation involvements. However, readers would be well advised to familiarize themselves with the indications, contraindications, therapeutic potentials, and technical execution of periodontal regenerative treatment modalities.
Implant Placement in Molar Sites
Performing implant placement with concomitant regenerative therapy at the time of removal of maxillary and mandibular multi-rooted teeth offers the potential to lessen both the number of surgical sessions and the overall length of treatment. This approach should only be utilized if the final treatment outcomes will not be compromised compared to more conventional therapeutic approaches, including tooth extraction with augmentation therapy, and implant placement in a second surgical visit 6 to 8 months later.
Prior to initiating therapy, it is crucial to standardize definitions of success. While numerous authors have demonstrated the ability to place implants immediately into single or multi-rooted extraction sockets and attain predictable osseointegration, such a treatment outcome is not in itself an acceptable result. Lazzara8 documented implant placement at the time of tooth removal in 1989. The implant was inserted into a fresh maxillary bicuspid extraction socket and attained “fill” of the residual extraction socket defect as well as osseointegration. While this paper paved the way for the use of immediately placed implants, careful examination reveals two parameters that were less than ideal by today’s standards. The implant was placed significantly sub-osseous crest, a position not advocated by most clinicians. In addition, some buccal and palatal ridge collapse was evident at clinical re-entry. Such collapse may have significant esthetic and functional ramifications in specific clinical scenarios. Becker9, while reporting upon implant placement into fresh mandibular extraction socket defects, described attainment of osseointegration and high levels of implant success under function. However, examination of the available clinical re-entry photographs once again demonstrates significant buccal-lingual ridge collapse. When reporting upon placement of implants at the time of maxillary molar extraction and subsequent restoration with single crowns, Schwartz-Arad et al10 stated that all implants attained osseointegration and were functioning successfully. The authors’ definition of success was limited to short-term implant stability, characterized by maintenance of bone levels around the implants and lack of clinical mobility. However, the clinical case presented in the paper demonstrated that the implants were placed in the palatal root sockets of the extracted maxillary molars and angled toward the buccal, so that the crowns were fabricated in acceptable restorable positions. Although therapy was successful according to the parameters defined by the authors, patients restored in such a manner are left with more difficult areas in which to perform plaque control. In addition, the implant restorations are necessarily fabricated with buccal cantilevers, and the implants are subjected to significant off-angled forces during occlusion.
If implants are to be placed at the time of maxillary or mandibular molar tooth extraction, the clinician must be able to insert such implants in ideal restorative positions. When such positioning is not attainable, teeth should be extracted, appropriate augmentation performed, and implants placed in a second surgical visit.
Implant Placement in Mandibular Molar Sites
Replacement of hopeless mandibular molars with implant restorations has undergone significant evolution since the introduction of osseointegrated implants in the 1980s. Over the past 12 years, various treatment approaches have been advocated, including the following:
1. Tooth extraction, defect debridement, and implant placement approximately 12 months following resolution of any “inflammatory lesions” in the bone. While agreeing with the original protocols concerning implant placement in “infected sites,” this approach significantly protracts the course of therapy. In addition, the degree of alveolar ridge resorption post-extraction is unpredictable, often resulting in less than ideal alveolar bone at the receptor site for eventual implant placement.
2. Tooth extraction and defect debridement, followed by immediate placement of two implants in the root extraction sockets. This approach helps to avoid post-extraction bone resorption and permits the clinician to affect implant placement in a fresh extraction socket of sufficient dimension. However, the final prosthetic result of two “bicuspids” is less than ideal, as the concept of “bicuspidization” of a mandibular molar presenting with a deep furcation involvement was developed for utilization during resective periodontal therapy, and periodontal prosthetic reconstruction is inherently flawed. The result of sectioning a mandibular molar is not two bicuspids. If the ratio of the mesio-distal dimension to the bucco-lingual dimension of the created “interproximal space” is examined, it does not approach the ratio of the space between two mandibular bicuspids unless the roots of the mandibular molar are more dramatically flared than normal, or orthodontic therapy is employed to separate the sectioned roots. The result is an interproximal space that heals with a non-keratinized concave soft-tissue col form, posing a significant challenge to home care efforts. Although the osseointegrative bond has been shown to be less susceptible to extension of an inflammatory lesion from the gingival sulcus than its natural tooth counterpart, it is not impervious. Therefore, a treatment approach that results in a potential area for greater plaque accumulation and difficulty in plaque control efforts is not ideal.
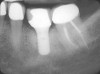
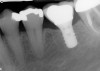
3. Extraction of a hopeless mandibular molar, defect debridement, and placement of an implant in one of the root sockets, followed by restoration with a molar-sized crown. This approach addresses the concern of two implants being placed closely together in the root extraction sockets. However, this treatment appropriately results in a mesial cantilever of the implant restoration and an area of potential plaque accumulation (Figure 1).
4. Tooth extraction, defect debridement, and placement of particulate graft material in the extraction socket defects, followed by second-stage implant placement. While this approach has traditionally offered an incremental improvement in treatment outcomes over Option 1, placement of particulate graft materials without the appropriate covering membrane, while effecting somewhat greater socket fill than tooth extraction with no graft material, results in a final alveolar bone quantity and morphology that is non-ideal and unpredictable.
5. Tooth extraction followed by particulate graft placement and utilization of an appropriate covering membrane, with second-stage implant placement. The desired alveolar ridge morphology may be predictably rebuilt in anticipation of implant placement, idealizing implant position and allowing use of the desired implant morphology.
6. Tooth extraction and immediate implant placement in an ideal restorative position, without the use of concomitant regenerative materials. When utilizing this treatment approach, an implant of appropriate dimension must be ideally positioned in the area of the interradicular bone. Assuming that the ideal implant position of a fixture of the desired dimensions and morphology has been attained, failure to perform concomitant regenerative therapy represents a potential treatment compromise. While an implant placed in a mandibular molar extraction socket without concomitant therapy will undoubtedly attain osseointegration, significant socket remodeling will occur in varying degrees, resulting in loss of bucco-lingual socket dimension and crestal height.
7. Tooth extraction followed by ideal implant positioning and concomitant regenerative therapy. This treatment approach should not be employed unless an implant of the desired dimension and morphology can be placed in an ideal restorative position. When such placement may be effected, the use of concomitant regenerative therapy results in preservation of all remaining alveolar bone in the extraction socket area, re-establishment of prepathologic alveolar ridge morphology, and bone buccal and lingual to the implant of sufficient thickness to withstand functional forces over time. The need for a second surgical session is eliminated.
Implant placement at the time of mandibular molar extraction should never be attempted if there is any doubt about the ability to place an ideal dimension implant in the appropriate restorative position and attain primary stability. In such a situation it is better to first perform regenerative therapy at the time of tooth removal and place the implant in a subsequent surgical session (Figure 2 through Figure 4).
All mandibular multi-rooted teeth are hemisected (or trisected in the rare cases of three-rooted mandibular molars) prior to removal. In such cases, a piezosurgical approach is utilized, in conjunction with specifically designed periotomes, to effect atraumatic tooth extraction. If such therapy is performed appropriately, the net result is an extraction socket whose alveolar morphology has been no further compromised through the act of tooth removal. In situations where high-speed rotary instrumentation must be used to help retrieve fractured root portions, the site is deemed no longer amenable to immediate implant placement due to the excessive trauma having been placed on the alveolar bone in the area. Regenerative therapy is performed employing appropriate graft materials and covering membranes, and the implant is placed in a second surgical visit. Such instances are rare.
Following tooth extraction, the defect is thoroughly debrided, and the extent and morphology of alveolar bone destruction are assessed. The presence or absence of periapical and/or periodontal inflammatory lesions prior to defect debridement plays no role in the determination of whether or not to immediately insert an implant. Rather, it is the morphology and quantity of residual alveolar bone in the extraction socket area that determines whether or not an implant will be placed at the time of tooth extraction.
Although ideal implant positioning may be attained in the vast majority of situations at the time of extraction of a mandibular molar, it is imperative that the surgical site is assessed after tooth removal and defect debridement is accomplished.
Implant Selection, Design, and Neck Diameter
Options available to clinicians regarding implant dimensions and morphologies have expanded greatly over the past few years. However, the plethora of available designs must not be viewed as a substitute for appropriate diagnosis and execution of therapy, but rather as an adjunct to the care to be performed. It is crucial that the appropriate implant dimension and design be employed in a given site that provides the most ideal restorative platform possible while resulting in the greatest volume of bone on the buccal and lingual aspects of the implant following healing.
Essentially, two implant designs are available for use. The first, often called a “tissue level” implant, is characterized by a stock or custom abutment being placed in the implant following attainment of osseointegration and the subsequent restorative margin resting on the shoulder of the implant body. The second design is referred to as a “bone level” implant. Such an implant configuration results in the crown margin resting upon the abutment, which has been inserted into the implant. A tissue-level implant design is preferable when replacing a missing molar, as greater stability is provided for the restoration following functional or parafunctional force application.
When replacing a missing molar, the widest implant neck diameter that is feasible is preferred due to mesio-distal space and tooth size limitations. Use of a wider neck diameter implant places the body of the implant under a larger portion of the restoration, thus reducing circumferential cantilever effects, providing greater support for the restoration, and lessening peak stress values to the peri-implant crestal bone.
Implant Body Diameter and Configuration
Upon their introduction, wider diameter implants were often utilized indiscriminately to replace missing molars in atrophic alveolar ridges, leading to a number of untoward results. Numerous authors reported loss of buccal bone around these implants under function over time, in the absence of inflammatory lesions. This bone loss was most probably due to the implants having been placed in areas that resulted in thin residual buccal alveolar plates post-insertion. Such thin alveolar bone is highly labile and susceptible to resorption under functional load. This is especially true around implants, as the forces placed upon the implants are distributed primarily to the crestal bone region.
When an implant is to be placed in an area where a mandibular molar is missing, and some ridge atrophy has occurred, implant design must be carefully considered. Two wide platform implant designs are available for use in such situations, one being a tapered implant, which presents with a 6-mm-wide or 6.5-mm-wide restorative platform and tapers to a narrower “apical” diameter; the second has a non-tapering body and flaring to the desired wider restorative platform supracrestally. The results attained utilizing each implant design differ.
If a mandibular molar is missing and significant ridge atrophy has occurred, a threaded implant is utilized with a 4.8-mm-wide straight-walled body and a 6.5-mm-wide restorative platform. The implant flares from 4.8 mm to 6.5 mm in width in the supracrestal area, between the bone crest and the implant collar (Figure 5). Use of this design affords the advantages of a wider restorative platform while preserving the maximum thickness of bone on the buccal and lingual aspects of the implant.
When a more conventional tapered implant design is employed, which is 4.8-mm-wide at its base and has a 6.5-mm-wide restorative platform but begins to flare to the final restorative dimension subcrestally as the diameter of the implant increases, the residual alveolar bone thickness on the buccal and lingual aspects of the implant is significantly reduced (Figure 6). This thinner bone is more susceptible to resorption under functional load.
If an implant is placed at the time of mandibular molar sectioning and extraction, such concerns are not present; the bucco-lingual dimension of the extraction socket is significantly greater than that encountered in an area where ridge atrophy has occurred. Therefore, utilization of either implant design with the appropriate concomitant regenerative therapy will result in bone of adequate thickness bucally and lingually to withstand functional forces over time.
When placing a fixture at the time of mandibular molar extraction, the overriding factor in implant design selection is the ability to attain primary stability in the residual interradicular bone in an ideal restorative position. Therefore, a third implant design may be utilized, which is characterized by a 4.1-mm-wide base and a 6.5-mm-wide restorative platform. The implant does not begin to flare toward the 6.5-mm-wide neck diameter until its midpoint is reached. This implant is especially useful for placement at the time of molar extraction if a narrower implant “apex” is required to anchor the implant in thinner residual interradicular bone.
Technical Variations on Extraction with Simultaneous Implant Placement
Once the tooth has been sectioned and each root has been independently and carefully extracted, implant placement should proceed in one of the following manners.
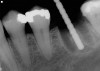
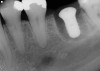
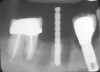
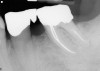
If the most crestal aspect of the interradicular bone is at least 3-mm-wide mesio-distally: A 2.2-mm-wide guide bur is drilled to the appropriate length, a guide pin is inserted, and a radiograph is taken (Figure 7). If necessary, the initial osteotomy is extended apically. A tapered osteotome is inserted into the osteotomy and moved mesio-distally and bucco-lingually to expand the osteotomy site. A 2.8-mm bur is used to prepare the osteotomy to depth, and a 2.8-mm-wide tapered osteotome is inserted in the osteotomy and once again utilized in mesio-distal and bucco-lingual directions to expand the osteotomy site. If the mesial and distal aspects of the interradicular bone are still intact at this point, a 3.5-mm bur is utilized to prepare the osteotomy to depth. A 3.5-mm-wide osteotome is inserted into the osteotomy and utilized in the manner already described. A decision is made as to whether to place a tapered implant with a 4.1-mm-wide base and a 6.5-mm-wide neck, or to use a 4.8-mm-wide bur and prepare the osteotomy to depth, in anticipation of placement of an implant with a 4.8-mm-wide parallel wall body and a 6.5-mm-wide platform. The chosen implant is inserted into the osteotomy (Figure 8), appropriate regenerative materials are placed, and the flaps are sutured. Following maturation of the regenerating hard tissues, the implant is ready for restoration (Figure 9). A radiograph taken 54 months after implant restoration demonstrates stability of the peri-implant crestal bone (Figure 10).
If the interradicular bone does not demonstrate a mesio-distal dimension of at least 3 mm, or if the mesial and/or distal aspects of the interradicular septum are lost during site preparation, the following modifications are employed: Following tooth hemisection and extraction, the depth and position of a guide pin are verified radiographically. When continued site preparation will result in loss of the mesial and/or distal aspects of the interradicular bone the bur has a tendency to chatter and “walk out of” the osteotomy into one of the root sockets, due to loss of the mesial and/or distal bony retaining wall(s). A variable pressure drilling technique is utilized to overcome this problem.11 The bur enters the interradicular bone at an angle, with the base of the bur engaging the lateral wall of the most apical extent of the osteotomy preparation. As the bur achieves a set point in the interradicular bone, it is straightened up and osteotomy preparation is begun. As osteotomy preparation continues, the mesial and/or distal aspects of the interradicular bone will be lost. In such a situation, pressure is applied against the buccal or lingual aspects of the interradicular bone as the bur enters the area. This pressure stabilizes the bur and allows the clinician to accomplish osteotomy preparation in an apical direction, thus stabilizing the bur and eliminating “chatter” as the bur enters the wider apical aspect of the interradicular bone. This same variable pressure joined technique is utilized with each subsequent bur.
Case reports of these techniques can be seen in Figure 11 through Figure 19.
Using such techniques ensures predictable ideal implant positioning at the time of mandibular molar extraction. A recent publication documents 341 implants placed and restored utilizing the described protocols. Of these implants 204 were of a parallel wall design with a 6.5-mm-wide restorative platform, and 137 were of a tapered design with a 4.1-mm-wide base and a 6.5-mm-wide restorative platform. Two implants were lost prior to abutment connection, and no implants were lost in function, yielding a cumulative success rate of 99.1% with a mean time in function 30.7 months and a maximum time in function over 6 years.11
Restorative Considerations
The restorative dentist’s decision-making process when considering the restoration of implants placed in posterior regions must include numerous factors. The arch must first be divided into the molar and premolar regions for the purpose of defining the type of implant being placed. Second, the arch that is being restored—the maxillary or mandibular arch—must be considered. At first glance there may not seem to be a difference between the two since similar implant types and sizes are used in both arches. However, there are different characteristics specific to each arch, and these can have a profound effect on the outcome of the restorative plan. Third, the choice of implant type, with respect to bone level or tissue level placement, must be considered. Each of the choices has associated complexities and considerations that must be assessed in the selection process.
There are a number of general issues that transcend the location in the arch, the arch itself, and the type of implant to be used. These issues, which must be considered and planned for before commencing therapy, include:
• Will stock abutments or custom abutments be employed?
• Will the planned restoration be opposed by natural dentition, implant supported-restorations, or a removable prosthesis?
• What will be the manner in which the restorative element is to be retained: will it be cemented “permanently,” provisionally, or screw-retained?
• How important is retrievability of the planned implant-retained prosthesis?
• Does the choice of material used to fabricate the restoration play an important part in the decision process?
• Do adjacent implant-supported restorations need to be splinted?
There are other factors, as well. The molar regions present with unique anatomical considerations, which must be managed surgically. Inferior alveolar nerve position and associated branches and bone thickness, dimension, and quality play significant roles in determining size and placement of an implant. Another anatomical consideration that influences the placement and restorability of an implant in the mandibular molar region is the buccal flair of the body of the mandible when moving posterior, and the acute nature of the mylohyoid space as measured from the mandibular alveolar ridge to the inferior border of the mandible.
There is a natural tendency for the mandibular body to open to the buccal, making it difficult to place an implant in alignment with the anterior-posterior aspect of the alveolar ridge. Surgically, one would want to place the implant in bone and follow the bone and the anatomical angle. Restoratively, the implant is often optimally placed in a vertical direction perpendicular to the anterior-posterior aspect of the alveolar ridge. This could result in fenestration of the mandible or other complications.
A restorative challenge develops when the implant is angled to such a degree that the restoration will extend into the lingual space and over-exaggerate the lateral curve of the occlusal table formed by the lingual inclinations of the posterior teeth. This concave curve is referred to as the Curve of Wilson. Such placement of an implant forces the restorative dentist to cause off-angle loading of the implant as there is need to regain an optimal occlusal table position. Custom restorative components must be employed to “change the angle” of the abutments to a more vertical position to accommodate for the final placement of the crown, adding to the overall expense of therapy. Should this occur, the crown(s) will interfere with the function of the patient’s tongue, and the patient will have an uncomfortable awareness of the restoration to which they may never acclimate.
Conclusion
The continued development of new techniques and the evolution of dentistry’s understanding of the potentials and limitations of various therapies afford the conscientious clinician sufficient information to ascertain when to utilize periodontal, implant, and/or regenerative therapies in the treatment of compromised posterior teeth. It is incumbent upon all clinicians to employ this knowledge to maximize treatment outcomes in the most efficient and reasonable manner. Patients deserve no less.
References
1. Becker W, Becker BE, Berg L, et al. New attachment after treatment with root isolation procedures. Report for treated Class III and Class II furcations and vertical osseous defects. Int J Periodontics Restorative Dent. 1988;8(3):8-23.
2. Goldman MJ, Ross IF, Goteiner D. Effect of periodontal therapy on patients maintained for 15 years or longer. A retrospective study. J Periodontol. 1986;57(6):347-353.
3. McFall WT Jr. Tooth loss in 100 treated patients with periodontal disease. A long-term study. J Periodontol. 1982;53(9):539-549.
4. Wood WR, Greco GW, McFall WT Jr. Tooth loss in patients with moderate periodontitis after treatment and long-term maintenance. J Periodontol. 1989;60(9):516-520.
5. Hirschfeld L, Wasserman B. A long-term survey of tooth loss in 600 treated periodontal patients. J Periodontol. 1978;49(5):225-237.
6. Wang HL, Burgett FG, Shyr Y, Ramfjord S. The influence of molar furcation involvement and mobility of future clinical periodontal attachment loss. J Periodontol. 1994;65(1):25-29.
7. Fleischer HC, Mellonig JT, Brayer WK, et al. Scaling and root planing efficacy in multirooted teeth. J Periodontol. 1989;60(7):402-409.
8. Lazzara RJ. Immediate implant placement into extraction sites: surgical and restorative advantages. Int J Periodontics Restorative Dent. 1989;9(5):332-343.
9. Becker W, Becker BE, Polizzi G, Bergstrom C. Autogenous bone grafting of bone defects adjacent to implants placed into immediate extraction sockets in patients: A perspective study. Int J Oral Maxillofac Implants. 1994;9(4):389-396.
10. Schwartz-Arad D, Grossman Y, Chaushu G. The clinical effectiveness of implants placed immediately into fresh extraction sites of molar teeth. J Periodontol. 2000;71(5):839-844.
11. Fugazzotto PA. Implant placement at the time of mandibular molar extraction: description of technique and preliminary results of 341 cases. J Periodontol. 2008;79(4):737-747.
Related content: For more information, read A Retrospective Analysis of 12 Immediate-Implant Restorations in the Maxillary Premolar Region at dentalaegis.com/go/cced186
About the Authors
Paul A. Fugazzotto, DDS
Visiting lecturer at Tufts University
Boston, Massachusetts
Boston University
Boston, Massachusetts
Harvard University
Cambridge, Massachusetts
University of Ancona
Ancona, Italy
Fellow, International Team for Implantology (ITI)
Basel, Switzerland
Private Practice
Milton, Massachusetts
Frederick O. Hains, DDS
Faculty Member and Course Director
Boston University Goldman School of Dental Medicine
Boston, Massachusetts
Private Practice
Braintree, Massachusetts