You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Since Hunter published his observations of non-carious loss of tooth structure (NCLTS) in 1728,1 dentistry has taken notice and has expressed its curiosity regarding this now commonly occurring pathology with volumes of papers with unproven suppositions and hypotheses.2-11 Because of this, a review of the literature reveals a state of confusion as to the etiology and especially the differentiation of this ever-increasing problem as people are living longer and retaining more teeth. Dentistry has a clear understanding of caries and periodontal disease, not only of their causes and diagnoses but their treatment and cures as well. However, the occurrence of NCLTS is more common than these other two diseases combined, giving dentistry a huge challenge as to the determination of its restoration and cure. Dentistry clearly knows what a normal tooth looks like anatomically and, therefore, easily recognizes NCLTS, but is confounded with the specific cause. This article provides a diagnostic system developed through an exhaustive study of the literature and observation in clinical practice that will enable oral healthcare providers to determine and differentiate the exact etiology of NCLTS simply by the recognition of the pathognomonic patterns that consistently result from the major causes of NCLTS. These patterns were developed from the application of accurate casts poured from alginate impressions12 mounted anatomically in adjustable articulators in centric relation, and the replacement of NCLTS with colored wax in its entirety to compare to normal dentition. The NCLTS collectively based on the quantity, position, and juxtaposition of all the affected teeth in an entire arch and the relationship of both arches to each other revealed patterns so consistent that they could be named pathognomonic. Upon learning the pathognomonic patterns of NCLTS, expeditiously, one does not need to wax nor mount casts in an articulator to determine the etiology and diagnosis of the cause(s). This, however, cannot be accomplished by mouth examination nor imaging; accurate casts is the best and only tool. Because everyone has some amount of NCLTS, the efficiency and accuracy of this system is greatly needed.
Terminology
A lack of uniformity in terminology to name pathology and disease creates confusion in medicine and dentistry. Fortunately, this is rare in medicine and dentistry, but strangely, on the subject of NCLTS our profession has not ever been consistent regarding how to define what it is observing. Even though Miller gave a complete listing of excellent definitions in 1907,13 dentistry could not reach consensus on etiology, so terminology waned and continues to do so today. Words such as wasting1 and denudation1 were used and even today there are terms like thegosis,7 abfraction,9 and corrosion.11 These examples have their origin from misunderstanding the cause and relying on imagination.
The classic dental texts organize the subject of NCLTS into three categories: attrition, abrasion, and erosion.16 Attrition is defined as the normal physiological loss of tooth structure from mastication. Abrasion is defined as the pathological loss of tooth structure from a mechanical/rubbing process. Erosion is defined as the pathological loss of tooth structure from a chemical/dissolving process. Closer examination of these definitions led to a significant development in the understanding of the etiology of NCLTS. The definition of the use of the word attrition, typically cited in the literature, is not appropriate or particularly useful for the assessment of NCLTS. The amount of tooth structure loss from mastication is insignificant due to the low abrasivity of food and the minute tooth-to-tooth contact during this function; and as such, does not warrant a separate categorization. The word attrition, which means a gradual decrease, would be more accurately defined, in reference to NCLTS, as the pathologic loss of tooth structure from abrasion and erosion. Even though NCLTS has multiple causes it can only occur from the two processes: abrasion or erosion. To separate abrasion and erosion into categories is very helpful to determine the specific etiology of the cause.
Cupping or Cratering
The invaginations that are commonly observed on the surfaces of teeth have become a conundrum for dentistry to solve, especially because their occurrence is increasing. Logical but erroneous thinking would direct one to the process of erosion, but this study reveals that cupping/cratering can occur from either of the two categories. Because teeth are multi-layered, ie, enamel and dentin, once the enamel is abraded (Figure 1) or dissolved (erosion) (Figure 2), dentin, being softer and less mineralized, continues to be removed at a more rapid rate than the peripheral, surrounding enamel, creating morphologically a cup or crater on the tooth surface. This is not limited to the cusp tips, which are circular in shape, but can be found on any surface of any tooth with asymmetrical peripheries. The bottom of the cup/crater can be concave, flat, or even wedge-shaped, depending on how the abrasive or acid is delivered to the surface of the tooth. The simple definition of cupping/cratering is the non-carious invaginations on the surfaces of teeth caused by either abrasion or erosion.
Causes of NCLTS
Bruxism and toothpaste are the two major causes of NCLTS from abrasion; the three major causes from erosion are regurgitation, soda-swishing, and fruit-mulling. It is important to note that these causes rarely exist alone; combinations of causes are common. Consequently, the determination of the etiology of NCLTS can become complex. However, even though multiple patterns can overlay each other, the differentiation remains clear and pathognomonic. In contrast to what some authors have erroneously claimed,17 the patterns remain intact and pathognomonic regardless of the severity of tooth structure loss.
The following physical descriptions of the patterns based upon position and quantity of loss illustrated with images, an unraveling of the combination of causes, and a commentary of the patients' behavioral profiles are designed to assist oral healthcare providers in differentiating the five major causes, plus a method to decipher the minor miscellaneous causes as well. It is important to re-emphasize that this identification system can only be accomplished with accurate dental casts in hand. The pathognomonic patterns from abrasion and erosion detected on dental casts are an archaeological imprint that tells the story of what occurred before and likely (possibly) what is still happening (current).
Abrasion from Bruxism
Bruxism is the action of teeth rubbing together when not eating, with the mandible rubbing the mandibular teeth against the maxillary teeth. It is the major cause of NCLTS from abrasion. It occurs in a subconscious state of mind, predominately nocturnally during sleep, but also to a lesser degree diurnally during non-sleep. The pathognomonic pattern reveals the loss of tooth structure to be progressively greater toward the anterior teeth, because of the leverage change created by eccentric posterior interferences. The posterior tooth contact becomes the fulcrum point instead of the temporomandibular joint (TMJ), which alters the leverage system increasing the force applied to the anterior teeth. An exception to this would be the patient with an anterior open bite, but the pattern would still remain the same, ie, posterior greater than anterior. Cupping and cratering is commonly encountered with the effects of bruxism, but will be from a secondary cause, which is most often from toothpaste; patients who are heavy bruxers tend to brush their teeth with the same vigor as they brux.
A significant result from this study revealed that NCLTS from bruxism can be identified in everyone's dentition. This means that, in contrast to what dentistry has thought,17 all human beings brux; there are no exceptions. This author's continuous study, since 1972, of the NCLTS observed on dental casts worldwide has never produced a set of diagnostic casts that did not exhibit NCLTS from bruxism. Therefore, it should be noted that NCLTS from bruxism will always be present and can be in combination with other causes. The distinction between bruxism and clenching is important; bruxism is teeth together with mandibular movement, whereas clenching is teeth together without mandibular movement. All human beings also clench, but the compressive force is not enough to cause NCLTS and, therefore, is not a factor.
Bruxism is a parafunctional activity controlled by the central nervous system and the frequency is associated with stress.18 This coincides with the ubiquitous findings of bruxism because all humans harbor a degree of stress. Confirming the diagnosis can be accomplished through the recognition of the pattern and the observation that the NCLTS facets from bruxism of hand-articulated casts will coincide. Asking the patient whether they grind their teeth or not is futile and not necessary.
The patient shown in Figure 3 and Figure 4 exhibited severe NCLTS from bruxism. Examination of the casts indicated that the NCLTS was progressively greater toward the anterior teeth. Cupping and cratering was not present because there was no secondary cause. Figure 5 and Figure 6 detail another bruxism patient, but to a lesser degree and one with cupping/cratering caused by toothpaste. The cups or craters were not caused from bruxism because the teeth could not touch the bottom of the invaginations. In both featured patients, upon hand-articulating the casts, the NCLTS facets matched up and the diagnosis of bruxism was confirmed.
Abrasion from Toothpaste Abuse
Toothpaste abuse, as evidenced by patients brushing overzealously with toothpaste, is the second major cause of NCLTS from abrasion and can be viewed in combination with any of the other referenced causes. When toothpaste abuse is present, the anatomical detail of the affected surfaces is faded with a sandblasted appearance on dental casts, but is smooth, polished, and glossy intraorally. The quantity and positional pathognomonic pattern reveals the facial surfaces of the mandibular canines and premolars to be affected the most, and when the enamel is abraded through to the dentin, cupping and cratering will form. The NCLTS is not limited to these mandibular teeth, and can occur on any surface of any tooth, ie, wherever the toothbrush carries the toothpaste.
Patients who abuse toothpaste typically dislike the color of their teeth. These individuals mistakenly believe that the more they brush their teeth, the whiter they will become. Actually, the opposite occurs; as the enamel becomes thinner, the dentin is closer to the surface, resulting in a darker overall appearance, which encourages more brushing. Even though a demographic study by Ervin in 194419 revealed that the majority of people who use toothpaste exhibit the loss of tooth structure, this problem ensues undetected; the occurrence today is rampant with the greater emphasis on oral hygiene and whiteness. Confirming the diagnosis can be accomplished through observing the pathognomonic pattern and noticing that the worn surfaces of the hand-articulated casts do not coincide. In addition, it is helpful to have patients demonstrate their toothbrushing style. It will be apparent that they habitually rapidly scrub with horizontal strokes. A close examination should be made during their demonstration to observe the particular tooth surfaces that the toothbrush is delivering the toothpaste to correlate the positional wear on the casts. The amount and rate of loss is also based upon time, speed, and pressure of their stroke. All toothpastes are abrasive.20 An analogy to the potential harm can be tested in polishing an acrylic resin denture. It is the pumice that polishes the denture, not the rag wheel. Fine flour of pumice will wear the plastic just as much as coarse pumice; it is strictly a matter of time, speed, and pressure. Therefore, lower-abrasive toothpastes can be as damaging as high-abrasive toothpastes, and certainly not the solution to the problem.
Figure 7 and Figure 8 are examples of NCLTS resulting from toothpaste. Upon examination, one could see that the overall anatomical detail of the teeth was faded with a sandblasted appearance. A closer view of the facial surfaces (Figure 9 and Figure 10) illustrates this to a greater degree and one can observe that the normal intricate facial anatomy was completely missing. It is interesting to note there was no cervical recession of the gingiva, even though every surface of every tooth had been abraded. This is due to the fact that this patient had always used a soft, round-ended filament toothbrush.21-22 This patient's sole desire regarding her oral hygiene was to get her teeth whiter.
So that the previous example is not misleading, the behavioral profile of the toothpaste abuser is not necessarily the "caries-free immaculate oral hygiene patient," but can be virtually anyone who brushes their teeth with toothpaste. Figure 11 and Figure 12 illustrate a more advanced example of toothpaste abuse showing a patient with multiple restorations and some unkempt teeth. The anatomical details were faded with a sandblasted appearance and the silver alloy restorations were highly polished. The facial surfaces of the mandibular canines and premolars were affected the most, creating the pathognomonic pattern. Figure 13 and Figure 14 are a close-up view of this area, illustrating a cupping or cratering effect, but of the asymmetrical variety. This patient did not like the color of his teeth and spent an inordinate amount of time brushing his teeth. Again, likewise due to the exclusive use of a round-ended, soft-bristle toothbrush, note there was no cervical gingival recession in this case either. When the featured casts illustrating toothpaste abuse (Figure 7, Figure 8, Figure 9, Figure 10, Figure 11, Figure 12, Figure 13 and Figure 14) were hand-articulated, the worn surfaces did not match up and the diagnosis of toothpaste abuse was confirmed.
A distinction between the terms toothbrush abrasion and toothpaste abuse needs to be made, which will hopefully cause a paradigm shift in thinking and a better understanding about the pathological dynamics of the dento-gingivo-cervical junction. The non-rounded, unpolished bristle toothbrush, regardless of degree of stiffness, can damage gingiva (recession).21,22 Toothpaste can damage teeth (NCLTS) regardless of the type of brush.13-15,23-25 Because the deleterious effects of the toothbrush and toothpaste are two separate issues, ie, one can harm soft tissue and the other hard tissue, the all-inclusive term "toothbrush abrasion" is clinically inadequate and misleading. Therefore, the introduction of two new terms is essential: toothbrush recession and toothpaste abrasion (Table 1).
Erosion from Regurgitation
Regurgitation is the major cause of NCLTS from erosion with the quantity and positional pathognomonic pattern indicating that the loss of tooth structure is progressively greater toward the anterior teeth in the maxillary arch. This is caused by the action of the acidic projectile vomitus, which exits the mouth, and the position of the tongue when this occurs. With regurgitation, the acid dissolves tooth structure amorphously from the free margin of the gingiva on the lingual surface of the maxillary anterior teeth. The maxillary posterior teeth are affected more than the mandibular posterior teeth, particularly on the palatal surfaces, and the barrier created by the tongue somewhat protects the mandibular posterior teeth. The mandibular anterior teeth are never affected because the tongue covers and completely protects them. Cupping and cratering is quite common. If amalgam restorations exist, they will appear elevated.
The NCLTS from regurgitation is always found in the person who suffers from bulimia, a life-threatening, complex psychological disorder that is characterized by binge-eating and self-induced vomiting.26 It is never the result from other types of issues commonly associated with regurgitation, such as excess alcohol or pregnancy, and is extremely rare with gastroesophageal reflux disorder (GERD). The buffering capacity of saliva has to be overwhelmed before teeth can dissolve (erode) from low pH attacks.27 NCLTS from regurgitation can be present in combination with other causes, with the exception of soda-swishing and fruit-mulling. The binging/vomiting process is done rapidly, while soda-swishing and fruit-mulling are time-consuming. Diagnosis through discussion with the bulimic patient is very difficult because they characteristically deny their problem. Confirmation of the diagnosis is obtained through the recognition of the pathognomonic pattern and observing that the affected surfaces of the hand-articulated casts do not coincide. When a confession of the disorder is offered with a claim to be cured, but seems invalid, a small test amalgam is placed on the lingual surface of a maxillary anterior tooth; it is carved flush and then observed 6 months later. If it appears elevated, further confirmation and current active status is verified. Dentistry's role with the bulimic patient is to diagnose their disorder via the pathognomonic pattern and compassionately refer them to an eating disorder program.28
Figure 15 and Figure 16 exhibit NCLTS from regurgitation. When one visually compares abnormal to normal and positionally quantifies the loss of tooth structure, the pathognomonic pattern for regurgitation can be observed. Here, the amount of NCLTS on the maxillary teeth was progressively greater toward the anterior. The maxillary anterior tooth loss was amorphously smooth from the free margin of the gingiva on the lingual surface. The maxillary posterior teeth were affected more than the mandibular posterior teeth, particularly the palatal surface, due to the predominance of the bolus of vomitus on the dorsum of the tongue. The mandibular posterior teeth were partially protected by the tongue, and the mandibular anterior teeth were not affected from the acid. Cupping and cratering was present. When these diagnostic casts were hand-articulated, they did not match up. Figure 17 and Figure 18 display a more severe example demonstrating the same pattern, including restorations that appear elevated.
Erosion from Soda-Swishing
Swishing with carbonated soft drinks, the rapid back-and-forth movement of soda to reduce the carbonation and avoid the uncomfortable sensation in the throat, is the second major cause of NCLTS from erosion. Any brand of carbonated soda applies, including sugar-free varieties. Carbonated water, beer, and beverages other than soda have not shown to be a cause of NCLTS, regardless of pH. The quantity and positional pathognomonic pattern reveals the posterior teeth to be affected to a greater degree than the anterior because of the position of the tongue when this habit occurs. The mandibular first molars, which typically erupt at age 6, are affected the most because of gravity and the early childhood age this habit begins, ie, before the adult tooth erupts. Cupping and cratering with sharp enamel edges is always present. If amalgam restorations exist, they will appear elevated.
It should be noted that soda-swishers generally are not high-volume drinkers of soda because swishing takes a great deal of time; it can take some soda-swishers several hours to consume one can. Basic chemistry has shown that the motion of acid geometrically increases the rate of dissolution29, which is why high-volume consumers of soda may have a caries problem, but will not exhibit NCLTS. Soda-swishing can be observed in combination with other causes except regurgitation and fruit-mulling. Soda-swishing takes too much time for the bulimic, and fruit-mullers typically are too health-conscious to drink soda.
Confirmation of diagnosis occurs when the pathognomonic pattern is determined and the affected surfaces of the hand-articulated casts will not coincide. Unlike regurgitation, patients will freely admit to soda-swishing, and usually a family member has complained about the habit.
Figure 19 and Figure 20 are examples of NCLTS from soda-swishing. The posterior teeth were affected to a greater degree than the anterior teeth, with the mandibular first molar being affected the most. A chronological history can be observed by comparing the amount of loss of tooth structure of the mandibular second molars with the first molars, understanding when these teeth erupt, ie, ages 6 and 12 respectively (Figure 21); this archeological process can be used throughout both arches of teeth for the soda-swisher. Cupping and cratering was present with sharp enamel edges. When these casts were hand-articulated, they did not match up. The patient admitted the habit and the diagnosis of soda-swishing was confirmed.
Figure 22 and Figure 23 exhibit a more advanced example with significant NCLTS from bruxism that can be observed on the anterior teeth. Even though dentists restored some of the NCLTS with bonded composite restorations, an analysis interpolating that incursion allowed the pathognomonic pattern to still be uncovered. The posterior teeth were affected more than the anterior teeth. The mandibular first molars were affected the most. Cupping and cratering was evident with sharp enamel edges. The patient admitted the habit and, again, the pathognomonic pattern was recognized. The hand-articulated casts did not coincide, and the diagnosis of soda-swishing was confirmed.
Erosion from Fruit-Mulling
Fruit-mulling, the third major cause of the NCLTS from erosion, is a habit frequently observed in health-conscious patients, who consume fruit throughout the day with a delay in swallowing the pulp of the fruit so it can be mulled between the teeth, not unlike animals who ruminate. These patients are often vegetarians and heavy bruxers from a high level of stress. The quantity and positional pathognomonic pattern is similar to that caused by soda-swishing, but with some distinctive differences. The posterior teeth are affected more than the anterior teeth because of the position of the pulp of the citrus fruit the patient is mulling. During this mulling process, however, the acidic pulp is contacting the maxillary teeth and mandibular teeth simultaneously, thus causing an equal loss of tooth structure to all the posterior teeth, which distinguishes fruit-mulling from soda-swishing and regurgitation. Cupping and cratering is always present but with abraded enamel edges from the mulling/bruxing process. If amalgam restorations exist, they will appear elevated. NCLTS from fruit-mulling can be observed in combination with other causes with the exception of regurgitation and soda-swishing, because fruit-mulling takes too much time for a bulimic and the two have very dissimilar behavioral profiles. The fruit-muller's health-conscious diet eliminates soda as a cause.
Figure 24 and Figure 25 exhibit NCLTS from fruit-mulling. The posterior teeth were affected to a greater extent than the anterior teeth, with the maxillary and mandibular posterior teeth affected equally, not only to each arch, but every tooth juxtaposed to each other. Cupping and cratering was present with abraded enamel edges from the mulling action. The diagnosis was confirmed from the pathognomonic pattern along with the match-up of abraded enamel edges peripheral to the cups and craters and the admission of the habit by the patient.
Miscellaneous Causes
There are, of course, miscellaneous causes of NCLTS such as lemon-sucking, pipe-smoking, snuff-dipping, bobby pins, dental floss, antacid chewing, GERD, etc. The pattern will be unique to the particular habit. These miscellaneous causes can occur in combination with the major causes presented; however, they will only comprise a very small percentage of the patients who have NCLTS. Before the discovery of these pathognomonic patterns dentistry has approached the subject of NCLTS from a miscellaneous viewpoint, ie, assumptions, hypotheses, coincidental findings, questionnaires, and "garage logic" with little from which to draw convincing conclusions and nothing to differentiate the cause(s). Good dental literature is sparse, but there is enough information to dispel most of the popular erroneous hypotheses. To discover the less common miscellaneous causes, the differential diagnosis can be accurately determined by first eliminating the pathognomonic patterns of the five major causes featured in this article, and if some NCLTS is observed that does not fit into the five major patterns, then question the patient about his/her oral habits. Only one question is necessary for this: What do you put into your mouth every day between meals? This sometimes requires a 7-day inventory by the patient, but with patient cooperation the miscellaneous cause can easily be found.
Conclusion
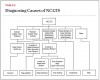
The pathognomonic patterns of NCLTS are collectively based on the quantity, position, and juxtaposition of all the teeth in an entire arch and the relationship of both arches to each other that is consistently specific to the cause. The effective loss of tooth structure will vary quantitatively and positionally with the time, pressure, and speed of motion of the abrasive or the acid on each individual tooth. When this is consistently repeated without variation, a pathognomonic pattern is established. By observing the quantity and positional NCLTS on accurate dental casts, the dental practitioner will discover these patterns and be able to precisely identify the various causes of this ever-increasing problem. Table 2 is a flowchart designed to expedite the diagnostic process for the etiology of NCLTS. To be successful in the treatment of any disease or disorder, one must be able to determine the cause before a cure is possible. The success of the restoration of NCLTS is dependent on this axiom. The clinical value of this author's discoveries should be obvious.
References
1. Hunter J. The decay of the teeth, by denudation. In: Diseases of the teeth, Section II; The Natural History of the Human Teeth. 2nd ed. London: J. Johnson; 1728:24-26.
2. Black GV. Erosion of the teeth. In: A Work on Operative Dentistry—The Pathology of the Hard Tissue. 1st ed. Chicago: Medico-Dental; 1908:39-59.
3. McCoy G. The etiology of gingival erosion. J Oral Implant. 1982;10(3):361-362.
4. McCoy G. On the longevity of teeth. J Oral Implant. 1983;11(2):248-267.
5. Smith BG, Knight JK. A comparison of patterns of tooth wear with aetiological factors. Br Dent J. 1984;157(1):16-19.
6. McCoy G. Dental compression syndrome: a new look at an old disease. J Oral Implant. 1999;25(1):35-49.
7. Scally KB. Bruxism: a worn out concept. J. Cranio. 1991;9(3):183-185.
8. Lee WC, Eakle WS. Possible role of tensile stress in the etiology of cervical lesions of teeth. J Prosthet Dent. 1984;52(3):374-380.
9. Grippo JO. Abfractions: a new classification of hard tissue lesions of teeth. J Esthet Dent. 1991;3(1):14-19.
10. Zero DT. Etiology of dental erosion—extrinsic factors. Eur J Oral Sci. 1996;104(2 pt 2):162-177.
11. Grippo JO, Simring M, Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. J Am Dent Assoc. 2004;135(8):1109-1118.
12. Abrahamsen TC. Accurate diagnostic casts from the sophisticated alginate impression (DVD). American Academy of Restorative Dentistry. 1999.
13. Miller WD. Experiments and observations of the wasting of tooth tissue variously designated as erosion, abrasion, chemical abrasion, denudation, etc. Dental Cosmos. 1907;49(1):1-23.
14. Miller WD. Experiments and observations of the wasting of tooth tissue variously designated as erosion, abrasion, chemical abrasion, denudation, etc. Dental Cosmos. 1907;49(2):109-124.
15. Miller WD. Experiments and observations of the wasting of tooth tissue variously designated as erosion, abrasion, chemical abrasion, denudation, etc. Dental Cosmos. 1907;49(3):225-247.
16. Shafer W, Hine M, Levy B, eds. A Textbook of Oral Pathology. 3rd ed. 1974; W.B. Saunders Company.
17. Christensen GJ. Treating bruxism and clenching. J Am Dent Assoc. 2000;131(2):233-235.
18. Rugh JD, Harlan J. Nocturnal bruxism and temporomandibular disorders. Adv Neurology. 1988;49:329-341.
19. Ervin JC, Bucher EM. Prevalence of tooth root exposure and abrasion among dental patients. J Dent Res. 1944;66:760-769.
20. Department of Health and Human Services. Food and Drug Administration. Anticaries drug products for over-the-counter human use; final monograph; final rule. Washington, D.C.: Federal Register, 1995; Part II, 21 CFR Part 310.
21. Alexander JF, Saffir AJ, Gold W. The measurement of the effect of toothbrushes on soft tissue abrasion. J Dent Res. 1977;56:722-727.
22. Silverstone M, Featherstone M. A scanning electron microscope study of the end rounding of bristles in eight toothbrush types. Quintessence Int. 1988;19(2):87-107.
23. Manly RS. A method for the measurement of abrasion of dentin by toothpaste and dentifrice. J Dent Res. 1965;44(3):533-540.
24. Sangnes G. Traumatization of the teeth and gingiva related to habitual tooth cleaning procedures. J Clin Periodontol. 1976;3(2):94-103.
25. Dzakovich JJ, Oslak RR. In vitro reproduction of noncarious cervical lesions. J Prosthet Dent. 2007;100(1):1-10.
26. Milosevic A, Slade PD. The orodental status of anorexics and bulimics. Br Dent J. 1989;167:66-70.
27. Bartlett DW, Evans DF, Anggian A, Smith BG. A study of the association between gastro-oesophageal reflux and palatal erosion. Br Dent J. 1996;181(4):125-131.
28. www.edrefferal.com. Eating Disorder Referral and Information Center. Date accessed: September 12, 2011.
29. Housecraft CE, Sharle AG. Chapter 6, Acids, vases and ions in aqueous solution. Inorganic Chemistry. 3rd ed. Prentice Hall. 2008.
About the Author
Thomas C. Abrahamsen, DDS, MS
Diplomate, American Board of Prosthodontics
International Lecturer on Restorative Dentistry
Private Practice Specializing in Prosthodontics
Mansfield, Ohio