You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Occlusal splint therapy has been shown to be useful for the diagnosis and management of various masticatory system disorders.1 Occlusal splints are frequently recommended by dentists and other health professionals to treat a variety of conditions, including bruxism/parafunctional habits, fatigued masticatory muscles, headaches, sore teeth, worn teeth, malocclusion, and noisy and uncomfortable temporomandibular joints (TMJ).
Occlusal splints have three primary purposes in modifying masticatory system dynamics:
1. alteration of the dental occlusion
2. reduction of muscle contraction and associated forces2
3. repositioning of the TMJ
Occlusal splints vary in design and application. Two basic types of splints are: permissive and directive.3 There are three basic designs of splints: anterior midpoint contact permissive splint; full contact permissive splint; and anterior repositioning directive splint. The decision to prescribe a particular splint is based on several important factors, including the findings from the examination, the differential diagnosis, and an understanding of the effects of each splint design. This article will discuss recommendations to guide decision-making.
Examination and Differential Diagnosis
Dr. Peter Dawson coined the phrase: “Dentists are the physicians of the masticatory system.” Dentists are exposed daily to conditions that lead to a full appreciation of the dynamic relationships of the TMJ, mastication muscles, dental occlusion, the trigeminal system, and central nervous system (Figure 1).
Many signs and symptoms are commonly manifested in the masticatory system and relate to disharmony, dysfunction, and deformation. A thorough history and examination of the teeth, muscles, and joints is the starting point for comprehensive care for all dental patients and is critically important for those experiencing masticatory system problems. The complete examination is essential for a differential diagnosis (Figure 2).
A systematic approach will differentiate problems into three basic categories:
- Extracapsular: a masticatory system problem without joint derangement
- Intracapsular: a derangement inside the TMJ capsule
- Other: a medical condition affecting the masticatory system, which often requires expertise outside of dentistry to diagnose and treat, eg, systemic, neurologic (Figure 3).
During the examination, a few key questions are contemplated, starting with: “Where is the source of discomfort, if any?” At times, discomfort involves factors extending beyond the masticatory system. Examples include:
- referred pain from the cervical region;
- multi-sited systemic tenderness caused by fibromyalgia, chronic fatigue syndrome, or rheumatoid arthritis;
- radiating pain from reflex sympathetic dystrophy or chronic regional pain syndrome;
- central neurologic, pathologic, vascular, migrainelike phenomena; and
- trigeminal neuralgia with peripheral symptoms.
These illustrate problems that fall into the “other” category and should be referred to an appropriate medical specialist for evaluation and treatment recommendations. Occlusal splint therapy may or may not be therapeutic, depending on the diagnosis.
The next question is this: “Does the problem appear to be intracapsular (in the joint)?” If the answer is yes, it is very important to clarify a joint diagnosis before treatment starts. The Piper Classification4,5 is used. Intracapsular disorders generally manifest as discal displacements (partial or complete) with potential osteoarthritis, as well as internal joint pathoses, such as rheumatoid arthritis or osteoma. Treatment options, including splint therapy, vary according to the joint diagnosis. Tomography, computed tomography scan, or magnetic resonance imaging may be necessary to clarify the internal status of a deranged joint. When in doubt, go find out. Diagnose and then treat.
The next question: “Does the problem appear to involve the masticatory muscles and/or occlusion?” Extracapsular occluso-muscle disharmony with parafunctional activity is most successfully treated with permissive splints. The clinician should think of each muscle pulling to create a specific mandibular movement; examination through muscle palpation will reveal tenderness of hyperactive masticatory muscles. For example:
- Clenchers will typically express tenderness of the temporalis and masseter muscles.
- Chronic forward posturing creates tenderness in the lateral pterygoid and anterior neck muscles.
- Hit-and-slide occlusions (centric relation to maximum intercuspation) with clenching/bruxing can create tenderness to palpation in all of the above mentioned muscles (Figure 4 and Figure 5).
It has also been demonstrated that hyperactive temporalis muscles are responsible for tension headaches as well as creating a noxious stimulus for sympathetic vascular changes that provoke migraines.6
Occlusal Splints
Two basic types of occlusal splints are permissive and directive. Permissive splints are designed to eliminate noxious occlusal contacts and promote harmonious masticatory muscle function. The primary function of these splints is to alter the occlusion so that teeth do not interfere with complete seating of the condyles and to control muscle forces. These represent the flat-plane appliances. The two classic designs of permissive splints are anterior midpoint contact splints and full contact splints.
Anterior midpoint contact permissive splints are designed to disengage all teeth except the incisors. This accomplishes several objectives:
- It removes occlusal interferences to complete joint seating on closure.
- Simultaneously, it allows freedom for full seating of the mandibular condyles when the elevator muscles contract on closure.7
- It encourages release of the lateral pterygoid and anterior neck positioning muscles on closure.
It has been shown through electromyography that molar contact allows 100% clenching force; cuspid contact permits approximately 60% maximum clenching force; and incisor contact minimizes elevator muscle clenching force to 20% to 30% of maximum clenching force.8 Therefore, muscle clenching forces are reduced significantly when contact is isolated exclusively on the incisors. The width of the midpoint contacting platform is limited to the width of the 2 lower incisors, measuring 8 mm to 10 mm. Eliminating posterior teeth contact significantly reduces noxious sensory feedback, through the trigeminal afferents, from previously sore temporalis muscles, which can evoke sympathetic vascular changes intracranially. This is the premise of the nociceptive trigeminal inhibition (NTI) splint (Figure 6). Other examples of anterior midpoint contact permissive splints include the Lucia jig (Great Lakes Orthodontics, LTD, Tonawanda, NY) (Figure 7) and the B splint (Figure 8).
Full contact permissive splints are designed to create an idealized occlusion in a reversible manner (Figure 9). Uniform contacts are established on all teeth when the joints are fully seated by the elevator muscles or manually by the clinician. Dawson’s bimanual manipulation technique is used to seat the joints when adjusting the splint occlusion in centric relation (Figure 10). It is critically important that the joints be fully seated to harmonize the occlusion properly in this border position of mandibular function. Attention to this one detail is often the key for maximizing therapeutic outcomes with full-contact splints. In excursive movements, only the anterior teeth touch, so as to reduce elevator muscle activity. A smooth, shallow cuspid-to-cuspid ramp is designed to provide anterior guidance, which provides horizontal freedom of movement as well as immediate disclusion of all posterior teeth.
The benefits of full contact permissive splints include:
- elimination of discrepancies between seated joints and seated occlusion (CR = MI)
- a large surface area of shared biting force
- reduced joint loading
- idealized functional occlusion
- the opportunity to observe for occlusal and joint stability over time
Full contact permissive splints can be made on the upper or lower arch (Figure 11). Lower splints have certain advantages that make them a favorite for many experienced clinicians. These advantages include:
- fewer speech changes (compared with upper splints)
- lower visibility in social settings
- shallower anterior ramps
- less tooth soreness when retention is gained exclusively on the lingual of the lower posterior teeth
- better patient compliance when instructed to wear their splints during the day as well as at bedtime
Directive splints guide the mandibular condyles away from the fully seated joint position when a painful joint problem is present. Whereas permissive splints clear the occlusion to allow the condyles to be fully seated superiorly/anteriorly by the elevator muscles, directive splints prevent full seating of the joints by guiding the mandible into a forward posture on closure into the occlusal splint.
Anterior repositioning directive splints are useful in two scenarios of joint management: severe trauma with retrodiscal edema and chronic, painful disc displacement disorders (Figure 12).
Severe Trauma with Retrodiscal Edema
In acute injury situations, with swelling of soft tissue behind the condyle, it may prove prudent to hold the condyle forward to prevent compression on the damaged retrodiscal tissues. Dr. Parker Mahan, former chairman of the Facial Pain Center at the University of Florida, College of Dentistry, coined the phrase “Cheerleader syndrome” because of the number of patients who fell on their chins at summer cheerleading camps and experienced painful joints with swelling edema and acute posterior open bites. “Airbag syndrome,” “Barfight syndrome,” and “Extreme Games syndrome” are a few more examples. In each case, moving the condyles forward for a period of 10 to 14 days will therapeutically decompress the injured, swollen, tender tissues. This approach is combined with a nonchew diet, antiinflammatory medications, and physical therapy.
Chronic, Painful Disc Displacement Disorders
If an anterior disc displacement is causing retrodiscal compression by the condyle, there may be a benefit to moving the condyle to a more forward position both in the fossa and underneath the disc. If it is possible to achieve complete reduction of the disc in a forward joint position but not in a superiorly seated joint position with a permissive splint, a directive splint may help maintain condyle disc alignment. The challenge is the long-term instability of this arrangement. It is generally not possible to realign the damaged condyle disc assembly in a forward position and then carry it back intact to the most superior musculoskeletally braced position. This can become a long-term management dilemma. Serious concerns include fibrotic contracture of the lateral pterygoid muscles, unstable soft tissue formation in the joint, and an unstable bite.
Treatment Options
What follows are possible applications of the use of occlusal splints ranging from simple scenarios to more complex ones.
Manifestations of simple occluso-muscle problems:
1. signs with minimal symptoms (tooth wear, mobility, drifting, muscle tenderness to palpation)
2. occlusal instability and incoordinated muscle activity because of the discrepancy between the seated joints (CR) and the seated occlusion (MIP)
In such cases, the use of an anterior midpoint contact permissive splint will achieve muscle release typically in a matter of 1 to 5 minutes. Occasionally, total relaxation of the jaw muscles may require deprogramming for several hours or overnight.
1. The occluding surface covers the central incisors only, with perpendicular contact of the opposing central incisors. The Lucia jig relined with warmed stick compound is a very efficient chair-side method.
2. The patient is instructed to rub forward and back several times on the occluding surface, then rest on the deprogrammer in a retruded position for 1 to 2 minutes. The mandible will usually relax very quickly as the elevator muscles seat the joints and the lateral pterygoid muscles release.
3. Orthopedic load testing of the TMJs via Dawson’s bimanual manipulation technique will be negative to tension or tenderness.
4. The occlusal prematurities in centric relation will be easily identified when the deprogrammer is removed.
The deprogramming will prove diagnostic and lead to CR diagnostic study models, occlusal analysis, and appropriate occlusal correction.
Occluso-muscle-parafunction problems result from the combination of “occlusion” and “occluding.” Clinical experience teaches us that it is not only malocclusion but also elevated muscle occluding forces that get many patients into trouble. A poor bite combined with parafunctional habits of clenching and grinding will create more significant signs and symptoms (sore muscles, headaches, sore teeth, tooth wear facets, etc).
Anterior midpoint contact permissive splints are capable of addressing both issues:
1. erasing the malocclusion
2. decreasing muscle forces, by separating all teeth distal to the incisors
Symptoms, such as sore muscles and teeth, can be resolved very quickly with these splints worn 24 hours per day (removed at mealtimes) for 1 to 4 weeks.
B splints and NTI splints are ideal for the treatment of occluso-muscle-parafunction problems. B splints are fabricated in the office, using 1.5 mm of Biocryl (Great Lakes Orthodontics), BIOSTAR® (Scheu Dental, Iserlohn, Germany), orthodontic resin, and a pressure pot. Stock NTIs are relined with snap acrylic chair side or are custom made by Keller Laboratories, Inc (Fenton, MO).
This provides a very effective approach for a short initial phase of occlusal splint therapy.9 Upon successful resolution of symptoms, occlusal analysis and appropriate occlusal correction are implemented. In many cases, symptoms remain absent, without the use of a splint, after definitive occlusal therapy. The perfected occlusion in centric relation, with proper anterior guidance, and immediate posterior disclusion become a built-in full arch permissive splint.
Parafunction can present a problem even in the absence of occlusal discrepancy. In some cases, symptoms may remain after definitive occlusal correction, if parafunctional clenching remains. Clenching can create sore temporalis and masseter muscles, even in a perfected occlusion. In such cases, if this leads to discomfort upon waking, the patient should continue wearing the splint at bedtime, as needed, indefinitely. Counseling regarding daytime parafunction and biofeedback are also important, as has been found through jaw tracking (Bioresearch Associates, Milwaukee, WI). Patients with muscle pain typically hold their teeth together when at “rest.” This daytime hyperactivity of elevator muscles can lead to muscle fatigue and headaches later in the day.
A nightguard to control the harmful effects of nocturnal parafunction may be used indefinitely to prevent muscle symptoms and protect the teeth from excessive wear. However, extended use of a segmental appliance/splint can sometimes lead to intrusion of the teeth touching the splint and supraeruption of the teeth not touching the splint. To prevent undesired tooth movement with extended usage, consider having the patient wear a dual splint covering both arches at night (Figure 13).
Full arch permissive splints provide the traditional approach to treating occluso-muscle-parafunction problems. The author used this design exclusively for more than 20 years with good subjective results in most cases. Less-than-acceptable improvement was typically related to persistent muscle fatigue, continued headaches, or an awareness of clenching on the splint. Muscle relaxants and sleep medications were used, after 1 week of exclusive splint therapy, with approximately 10% of those patients with an occluso-muscle disorder. Experimenting clinically with anterior midpoint contact permissive splints resulted in a significant subjective improvement that reduced the need for medications in these cases to almost zero. It is the parafunction component that can be better managed when the posterior teeth are disengaged continuously. This results in reduced elevator muscle soreness and improved management of both tension headaches and migraines.10
Full arch permissive splints are excellent for idealizing occlusions in a reversible manner and therefore are often effective in treating occluso-muscle problems. When parafunction, in the form of clenching, is thought to be a significant factor, anterior midpoint contact permissive splints have distinct advantages.
Joint disorders commonly present as partial or complete anterior disc displacement. Disc displacements can result from a combination of:
- elimination of symptoms, including sore muscles and joints
- verifiable comfort to orthopedic load testing and joint palpation
- stability of the occlusion on the splint for several weeks, reflecting underlying joint stabilization
1. macrotrauma from injury
2. microtrauma caused by:
a. sustained overcompression of the joint (parafunction) b. anterior tension on the disc from sustained contraction of the superior belly of the lateral pterygoid muscle (malocclusion, parafunction)
3. “weak link” factors, such as collagen disorders, ligament weakness, and hormonal imbalance
Partial disc displacement typically occurs at the lateral aspect (Piper stage III) of the condyle (Figure 14).
Treatment using occlusal splints has three primary goals:
1. harmonizing occluso-muscle-joint relationships
2. decreasing the load to the damaged joint tissues
3. eliminating symptoms related to intracapsular edema and inflammation and muscle pain caused by splinting and parafunction
Full arch permissive splints (Figure 15) are typically prescribed for several reasons:
1. Contact of all teeth is believed to create a large surface area of force distribution at the occlusal end of the jaw system, with a large reduction in compressive loading in the weakened joint complex. It is reported that as little as 5% of the total biting force goes through the joints with this design. Decreased joint loading will decompress the retrodiscal tissues and create a better environment for adaptive healing. More studies comparing joint loading forces using anterior midpoint contact permissive splints vs full arch permissive splints would be helpful. Several excellent clinicians use anterior midpoint contact permissive splints in partial disc displacement cases and report excellent clinical outcomes. The rationale is that the cause of the problem relates to forces and parafunction. Anterior midpoint contact permissive splints are the most effective appliances to control parafunction forces, by separating all teeth distal to the incisors.
Other authorities are concerned that anterior midpoint contact permissive splints may create a risk of further disc displacement; therefore, consider these splints contraindicated.
What is the answer? Further research is needed using both designs to accurately determine the comparative joint loading and vector of forces through the joints.
Until such time, the author recommends full arch permissive splints.
1. Release of the lateral pterygoid muscles decreases tensive forces on the disc anteriorly. Because of the presence of hard and soft tissue damage (not found in occluso-muscle disorders), the time required to achieve adaptive stability with a partial disc displacement is longer. It usually takes 6 to 8 weeks to reach acceptable resolution, with splint therapy and antiinflammatory medications.
Acceptable resolution includes:
Complete disc displacement (Piper stages IV through stage V) can present a complicated derangement in the joint that may or may not be improved through the use of occlusal splints (Figure 16). Patients with the disc off both lateral and medial aspects of the condyle are considered chronically unstable and possible candidates for surgery, similar to an individual who has torn knee ligaments and a meniscus tear. Acutely, innervated and vascular retrodiscal tissue is being compressed and loaded. Chronically, ligament perforations, scar tissue, and bone-to-bone contact with osteoarthritis develop over time.
Occlusal splint therapy for these conditions has the same three primary goals as for partial disc displacements, when possible. The splint occlusion will be adjusted weekly until it stabilizes as the joints hopefully remodel and adapt. In readily adaptable Piper stage IV and V joints, the total time in splint therapy averages a minimum of 3 months. This time will be extended if discomfort persists and/or the splint occlusion keeps changing, both of which reflect continued joint instability.
If the joint cannot be seated fully without discomfort, a hard, wax bite record (Delar wax) will be obtained intraorally in a slightly forward posture and tested for comfort with clenching. If the patient can bite without discomfort on the wax record, a full arch permissive splint will be fabricated on a study model using the wax record at the “treatment position” and a facebow transfer. The splint will be adjusted weekly as the joints adapt and are eventually fully seated.
If the damaged joint can be seated without discomfort only in a significantly forward position, then an anterior repositioning directive splint can be fabricated.11 A wax bite record will be taken in a protrusive, comfortable treatment position. If this approach is utilized, it is as a last attempt to see if avoidance of retrodiscal tissue loading will initiate an adaptive response. This patient’s prognosis for splint therapy is guarded, and a surgical consult should be considered. Typically, the use of this splint is limited to 2 weeks before returning to a full arch permissive splint or referring for a surgical consultation.
Summary
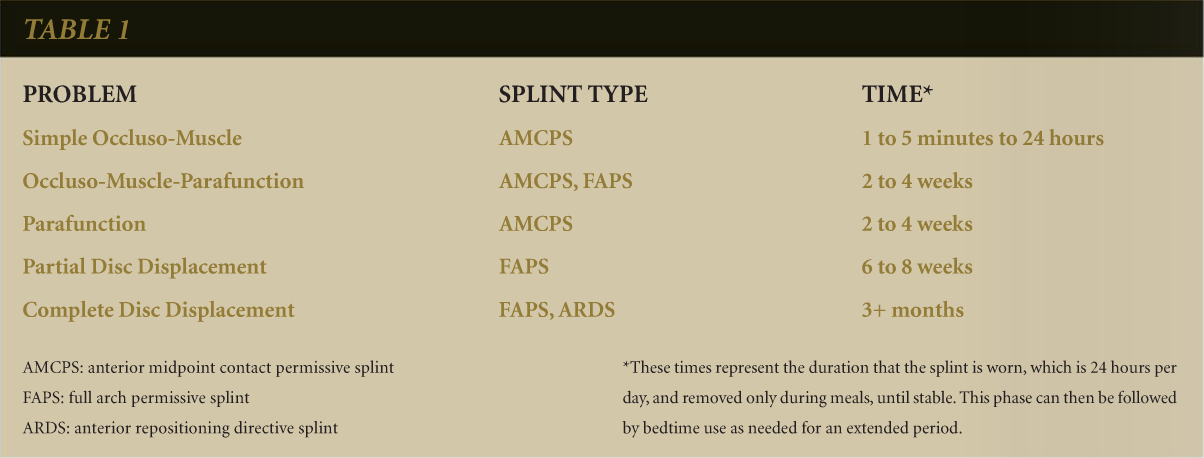
Occlusal splint therapy is an effective means of diagnosing and managing specific masticatory system disorders. A summary of the most typical applications is presented in Table 1.
Conclusion
It is imperative that clinicians have a strong working understanding of masticatory system dynamics. Differential diagnosis through the screening of muscles, joints, and dental occlusion will clarify the presence of signs and symptoms of dysfunction. Controlling the effects of malocclusion and parafunction is typically successful through the selective application of the occlusal splint designs described in this article. Joint derangements are often manageable using occlusal splints, but due to multifactorial etiology, may have some limitations relative to creating long-term joint stability.
References
1. Kreiner M, Betancor E, Clark GT. Occlusal stabilization appliances. Evidence of their efficacy. J Am Dent Assoc. 2001;132(6):770-777.
2. Manns A, Valdivia J, Miralles R, et al. The effect of different occlusal splints on the electromyographic activity of elevator muscles. A comparative study. J Gnathol. 1988;7:61-73.
3. Dawson PE. Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby; 2007:379-392.
4. Piper MA. TMJ diagnostics and basic management. Seminar manual. Piper Clinic, St. Petersburg, FL. 2006.
5. Dawson PE. Functional Occlusion: From TMJ to Smile Design. St. Louis, MO: Mosby;2007:312-320.
6. Shankland WE. Nociceptive trigeminal inhibition-tension suppression system: a method of preventing migraine and tension headaches. Compend Contin Educ Dent. 2002;23:105-113.
7. McKee JR. Comparing condylar positions achieved through bimanual manipulation to condylar positions achieved through masticatory muscle contraction against an anterior deprogrammer: A pilot study. J Prosthet Dent. 2005;94(4):389-393.
8. Becker I, Tarantola G, Zambrano J, et al. Effect of a prefabricated anterior bite stop on electromyographic activity of masticatory muscles. J Prosthet Dent. 1999;82(1):22-26.
9. Boyd JP, Shankland WE, Brown C, et al. Taming destructive forces using a simple suppression device. Postgrad Dent. 2000;7:1-4.
10. Magnusson T, Adiels AM, Nilsson HL, et al. Treatment effect on signs and symptoms of temporomandibular disorders—comparison between stabilization splint and a new type of splint (NTI). A pilot study. Swed Dent J. 2004; 28(1):11-20.
11. Williamson EH. Temporomandibular dysfunction and repositioning splint therapy. Prog Orthod. 2005;6(2):206-213.
About the Author
DeWitt C. Wilkerson, DMD, Senior Faculty/Lecturer, Dawson Academy, Adjunct Professor, University of Florida College of Dentistry, Partner, International Center for Complete Dentistry, St. Petersburg, Florida

















