You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Cone beam computed tomography (CBCT) has changed the way clinicians diagnose and determine the best course of treatment. Often this can mean the difference between solving the mystery of a patient's pain or missing a vital indicator. Formerly used only in unusual clinical scenarios, CBCT has advanced to almost commonplace use in dentistry as its costs have decreased and access to the technology has increased.1 As CBCT first became more accessible, dental specialists quickly embraced three-dimensional (3D) imaging as a means by which they could distinguish their practices as being on the cutting edge of technology. Oral surgeons, periodontists, and orthodontists valued the anatomical structures visible in a large field-of-view CBCT scan, whereas endodontists appreciated the extraordinary level of detail achieved in high-resolution focused field-of-view scans. Even maxillofacial prosthodontists such as Scott Ganz, DMD, have pointed out that "there's danger when we're bound by two dimensions in a three-dimensional world."2 Shortly after, general dentists recognized the impact that 3D imaging can have on their ability to make accurate diagnoses. Today, patients expect their dentist to be contemporary and utilize the latest technology available in treatment.
As more clinicians adopt this technology, it is important for users as well as referring practitioners to understand the basic concepts and different applications of this imaging modality. The large field-of-view, low-dose CBCT scan acquired by the patient's orthodontist does not help address the questions raised by the patient's endodontist when a root canal treatment is warranted. Recognizing when CBCT is needed, why it can beneficial, and which imaging protocol provides more relevant information in each case is the key to benefiting from this technology.
Customizing Imaging Protocols for Patients
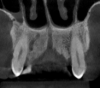
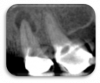
Every patient is unique, and every clinical situation requires a treatment plan customized to meet each patient's needs. In the same way, CBCT imaging can and should be customized to each patient or diagnostic task to optimize image quality and increase diagnostic accuracy. It can be easy to "set it, forget it" and take the same scan on every patient who needs a scan, but tailoring the settings on a CBCT machine can significantly affect image quality and increase diagnostic accuracy (Figure 1 and Figure 2). Some of the configurable factors include field of view, voxel size, patient positioning, and metal artifact reduction (MAR) reconstruction algorithm.
It would also be simple and straightforward to reduce radiation doses to extremely low levels, but such extreme low-dose levels may render images diagnostically useless. In fact, imaging protocols have evolved in adapting the traditional ALARA (As Low As Reasonably Achievable) principle toward ALADAIP (As Low As Diagnostically Acceptable being Indication-oriented and Patient-specific).3 What constitutes adequate image quality depends on the modality being used and the clinical question being asked.
Evaluating CBCT Scans in a Comprehensive Manner
There is little dispute that CBCT provides superior representation of anatomy compared with two-dimensional (2D) plain films. 3D imaging facilitates the localization of anatomical variations, reveals the relationships of structures, and helps identify the origin of pathosis (eg, untreated/unobturated canals, root resorptions, or fractures).
Variations of Normal Anatomical Structures
Knowledge of anatomical variations is extremely important for planning treatment and avoiding complications postoperatively. Precise imaging becomes especially important in surgical cases that might involve vulnerable structures, including sinus cavities, nerve channels, or blood vessels. One of the variations rarely discussed is the canalis sinuosus, a neurovascular canal, nerve branch of the infraorbital canal, that passes the anterior superior alveolar nerve (Figure 3).4
Detection of Periapical Pathosis
Furthermore, 3D imaging identifies up to 40% more of previously undetectable lesions.5 2D imaging modalities provide patchwork information of anatomic segments to represent 3D anatomy. This diagnostic variability is noticeable in endodontically treated and untreated teeth, especially in the posterior maxilla (Figure 4 and Figure 5). Patel et al have also elaborated on the limitations of detecting periapical lesions using periapical radiographs in necrotic teeth.6A visible radiolucency surrounding an apex depends on the size of the lesion, density and thickness of the cortical plate, and the distance between the lesion and cortical plate.
Vertical Root Fractures
In addition, vertical root fractures can be even more difficult to visualize using routine radiographic techniques. Long-standing fractures usually show changes in the surrounding bone pattern. However, a recently fractured tooth can be more difficult to identify radiographically, especially in the presence of metal artifacts caused by metal restorations, endodontic posts, root fillings, and implants. Therefore, reconstruction algorithms such as MAR can greatly enhance the quality of images and reduce the effect of beam hardening and scatter that may be present (Figure 6 and Figure 7).
External Cervical Root Resorption
In some cases, incidental findings such as external cervical root resorption require dynamic navigation through the three axes provided on a focused field-of-view CBCT scan to determine prognosis and possible treatment plan options. The clinical presentation of external cervical resorption depends considerably on the size, location, and extent of the resorptive process (Figure 8 through Figure 10). Some cases classified as Heithersay class I or II, typically assigned a "good" prognosis, could present with up to 28% of the root structure affected by the resorptive defects.7
Airway Analysis
The applications of CBCT imaging certainly extend beyond endodontic diagnosis. The ultimate goal of imaging is to portray the anatomic "truth" to help in diagnosis and treatment planning. CBCT imaging for the primary evaluation of the airway has been greatly debated. Studies have shown that certain craniofacial patterns are related with smaller dimensions of the upper airway.8 Some of the most common qualitative factors include retrognathia, steep mandibular plane, hypoplastic maxilla, and reduced transverse dimension of the maxilla. Quantitatively, airway volume, minimum cross-sectional area, and airway length can be automatically computed using the imaging software (Figure 11 and Figure 12).9
3D Imaging for Implant Planning and Beyond
Software capabilities permit visualization of a CBCT scan from any angle, and specific areas in a scan can be segmented for further analysis. The use of CBCT has intensified in part due to its advanced software tools. 3D imaging has not been used simply as a diagnostic tool, but rather as a productivity tool that helps dentists treat patients more efficiently.
Over the next few years, dynamic software applications based on 3D imaging will also mature and become more enriched. We have already witnessed the effect of computer-aided design/computer-aided manufacturing (CAD/CAM) technology and 3D implant planning. CBCT scans can be automatically merged with digital impressions within seconds without points matching. Virtual implants can then be planned with the final restoration in mind. The communication between different platforms makes the entire process faster and more efficient, which is important for a busy practice with many implant surgeries on the schedule.
Improvements in software technology will bring more capabilities, including virtual treatments, simulations, and new possibilities for guided surgery, than are available now. It is anticipated that CBCT will go beyond static imaging to create something tangible.
Some of the applications of CBCT include the ability to incorporate a dynamic element to reproduce occlusion and the movement of the arches. This is driven by the idea that both static and dynamic parameters should be considered in order to achieve complete diagnostics. Other applications involve dynamic navigation systems that track the position of the tip of the implant drill and map it to a preacquired CBCT scan of the patient's jaw to provide real-time drilling and placement guidance/feedback. Dynamic navigation is gaining traction in endodontics as well, especially in calcified canals. These advancements in software and static/dynamic guide partners have brought more proficiency, flexibility, and precision to treatment planning.
Conclusion
CBCT technology is increasingly becoming an integral part of daily dental practice. The anatomic and diagnostic accuracy provided by 3D imaging have enormous impact on the prognosis and reliability of the treatment that is provided. Incorporating 3D imaging will allow practitioners to approach cases in a comprehensive manner, beyond focusing on a specific tooth or other area of interest in the oral cavity.
DISCLOSURE: The author is the Clinical Education Specialist at Carestream Dental.
References
1. Whitesides L. Cone beam computed tomography: is dentistry ready for a new standard of care? Cone Beam - International Magazine of Cone Beam Dentistry. 2014;4.
2. Rinaldi M, Ganz SD, Motolla A. Computer-Guided Applications for Dental Implants, Bone Grafting, and Reconstructive Surgery. 1st ed. Elsevier; 2015.
3. American Dental Association Council on Scientific Affairs. The use of cone-beam computed tomography in dentistry: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2012;143(8):899-902.
4. Arruda JA, Silva P, Silva L, et al. Dental implant in the canalis sinuosus: a case report and review of the literature. Case Rep Dent. 2017;2017:4810123.
5. Pope O, Sathorn C, Parashos P. A comparative investigation of cone-beam computed tomography and periapical radiography in the diagnosis of a healthy periapex. J Endod. 2014;40(3):360-365.
6. Patel S, Wilson R, Dawood A, Mannocci F. The detection of periapical pathosis using periapical radiography and cone beam computed tomography - part 1: pre-operative status. Int Endod J.2012;45(8):702-710.
7. Matny LE, Ruparel NB, Levin MD, Noujeim M, Diogenes A. A volumetric assessment of external cervical resorption cases and its correlation to classification, treatment planning, and expected prognosis. J Endod. 2020;46(12):1929-1930.
8. Neelapu BC, Kharbanda OP, Sardana HK, et al. Craniofacial and upper airway morphology in adult obstructive sleep apnea patients: a systematic review and meta-analysis of cephalometric studies, Sleep Med Rev. 2017;31:79-90.
9. Schendel SA, Jacobson R, Khalessi S. Airway growth and development: a computerized 3-dimensional analysis. J Oral Maxillofac Surg. 2012;70(9):2174-2183