You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
The United States' population is "graying" at a considerable rate. In 2003, the United States Census estimated that by 2013 there would be over 44.7 million Americans over the age of 65. In 2016, the number of Americans aged 65 and older was projected to more than double from 46 million to over 98 million by 2060. According to the American Association of Retired Persons (AARP), it is estimated that by the year 2060, people 65 years of age and older will represent nearly 24% of the population base. Currently, there are an estimated 53,000 persons in the United States 100 years old or older, the largest number of them residing in California, New York, and Florida. Advances in health care technology along with the baby boom of the 1940s and 1950s has resulted in more individuals surviving into the eighth and ninth decades of life and beyond, resulting in a larger percentage of the population being elderly.
In addition to the medical advances that have enabled people to live longer and healthier lives, dental advances have resulted in the preservation of healthy dentition in these later years. Edentulousness and dentures are no longer the inevitable consequences of aging. In 1958, 65% of the older adult patients were edentulous and wore full dentures; in 1985 the percentage dropped down to 48%; although the percentage continues to steadily decrease, the increase in the population of elderly people will offset the decrease to some extent. With the increases in retention of natural dentition, more elderly patients are being seen in dental practices more regularly to maintain their oral health. The older adult patient frequently presents a variety of treatment dilemmas during dental care, and certain factors should be considered when rendering treatment.
OLDER ADULT POPULATION
For persons born in the United States, the life expectancy has increased consistently during the last century. Greater numbers of older individuals are consequently seeking dental treatment. These patients require a full range of dental care: crown and bridge work, endodontics, periodontics, oral surgery, and restorative work as well as preventive dental care. Although many of these individuals appear to be in good health, it is important to remember the possible presence of other physical disabilities and that elderly patients are much less able to tolerate the stresses normally involved in planned treatment.
Gerontologists have divided the study of the older population into several categories based on chronological age:
• New-old...............(55-64 years)
• Young-old.............(65-74 years)
• Middle-old...........(75-84 years)
• Old-old.................(85-plus years)
Whatever terms are used to define your patients, two very important facts exist. Foremost, characterizations of age should be based on ability, not chronological age; and second, the majority of older adults perform at a high degree of independent function.
The majority of older adults with functional limitations and compromised health are over the age of 75 years. Chronological age refers to age as measured by calendar time since birth, while functional age is based on performance capacities. Although a calendar may signify a particular age, functional ability should be the standard that differentiates an individual's capability to maintain activity. There is a third definition of age, and that is subjective age. Subjective age is concerned with how the individual defines themselves and how one perceives him or herself in age is greatly dependent on one's functional age. The two most important factors in determining subjective age are one's activity level and one's health.
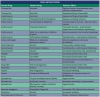
Table 1 lists the many changes frequently encountered in the geriatric patient. Decrease in tissue elasticity is a primary physiological change that has a consequential effect on organs throughout the body. For example, at 75 years of age, cerebral blood flow is around 80% of what it was at age 30; cardiac output has declined to 65% of what it previously produced, and the renal blood flow has decreased to 45% of its former volume. This decrease in renal perfusion has a potentially significant bearing on the actions of certain drugs, primarily those in which urinary excretion is a principal mode of removing the drug and its metabolites from the body. Drugs such as penicillin, tetracycline, and digoxin exhibit greatly increased beta half-lives in the older patient. Decreased tissue elasticity also affects the lungs. Pulmonary compliance decreases with age.
MEDICAL HISTORY
Updating medical histories of any patient but especially the older adult patient is crucial for diagnosis, treatment planning, treatment, and prognosis. For the initial appointment, a medical history form should be sent out by mail or email depending upon patient preference before the initial visit, so the patient does not feel rushed in filling out the form. If there is not enough time to mail out a form, asking the patient to bring a list of any medications and dosages can be very helpful to both the patient and dental team. It is often best to interview the patient alone in the treatment room, but for those with compromised mental health, a relative or caregiver should accompany the patient into the treatment room. In some instances, the patient may not be aware of all of the medications that he or she is taking, and it may be necessary to confer with the primary caregiver or physician before rendering treatment. Medical histories should be as specific as possible and consultation with the patient's physician may be necessary to resolve any questions that may arise from the medical history. All consultation notes must be documented in the patient record.
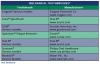
Prescription medications and all over-the-counter medications, vitamins, and herbal supplements should be listed with the medical history. Since adults are the leading consumers of multiple types of medications for various health conditions, the pharmacological implications of successful dental treatment must be carefully assessed. Certain medications may interact with some of the drugs used in the dental office, creating potential medical emergencies, especially if the dental team is unaware of the medication being taken. (See Appendix 1: Potential Drug Interactions) A complete and precise review of the medical history should be done at each appointment before treatment, even if the patient was in two weeks ago. Medications and medical conditions can change frequently; therefore, it is important to update the history at the start of each visit.
Many routine dental procedures, including ordinary brushing and flossing of teeth, can release bacteria into the bloodstream. In most instances, the resulting bacteremia poses no threat and the body's natural defenses attack and eliminate the invading microorganisms. Even in individuals who are endocarditis-susceptible, the bacteremia is usually eliminated by natural defense mechanisms. However, certain heart patients and joint replacement patients are vulnerable to the invading bacteria. Bacteremia in these patients can lead to infective endocarditis, a serious and often fatal condition. Even with the advancements of medical science, we are unable to predict with absolute certainty which patients will develop endocarditis or which procedures will be responsible for the infection. Therefore, every dental team member must identify patients with predisposing conditions and take measures to protect them from this condition. It is important to know which medical conditions put patients at risk and the relative severity of the risk. In the past, many dental patients were premedicated with antibiotics prior to certain dental procedures.
Since 2007, the American Heart Association (AHA) published updated guidelines for antibiotic prophylaxis, several times, thus eliminating the need of short-term antibiotics as a preventative measure for most of these patients before their dental treatment. Prior to 2012, premedication prior to dental procedures was common for joint replacement patients, even though there was little evidence to support the practice of premedicating for routine dental procedures. The updated AHA guidelines are based on a growing quantity of scientific evidence that shows the risks of taking preventive antibiotics out-weighing the benefits for most patients. The risks to the patient include adverse reactions to antibiotics that range from mild to potentially severe and, in very rare cases, death. Inappropriate use of antibiotics can also lead to the development of drug-resistant bacteria, a growing concern in the healthcare community. Research has also found no convincing evidence that taking prophylaxis antibiotics prior to a dental procedure prevents infective endocarditis in patients who are at risk of developing a heart infection. Their hearts are already often exposed to bacteria from the mouth, which can enter their bloodstream during necessary daily activities such as brushing or flossing. The current AHA guidelines are based on a comprehensive review of published studies that suggests infective endocarditis is more likely to occur as a result of these daily activities than from a dental procedure. (See Appendix 2: Endocarditis Risks) The AHA guidelines are designed for patients who would have the greatest threat of an adverse outcome if they developed a heart infection.
Knowing which dental procedures pose the greatest threat to susceptible patients is also important. Reduce the risk factor with careful planning and by educating the patient. The dentist in consultation with the patient's physician will then choose the antibiotic regimen most appropriate for each patient. (See Appendix 3: Prophylactic Regimens) Occasionally, a patient with a total joint prosthesis may present to the dentist with a recommendation from his or her physician that is not consistent with the new guidelines; this could be due to lack of familiarity with the guidelines or to special considerations about the patient's medical condition that are not known to the dentist. In this situation, the dentist is encouraged to consult with the physician to determine if there are any special considerations that might affect the dentist's decision on whether or not to premedicate. Following the consultation, the dentist may decide to follow the physician's recommendation or, if in the dentist's professional judgment antibiotic prophylaxis is not indicated, may decide to proceed without antibiotic prophylaxis.
The dentist is ultimately responsible for making treatment recommendations for his or her patients based on the dentist's professional judgment. Any perceived potential benefit of antibiotic prophylaxis must be weighed against the known risks of antibiotic toxicity; allergy; and development, selection, and transmission of microbial resistance. Generally, patients with joint replacement are premedicated for up to 24 months following placement, during which they are susceptible to infection.
In general, for patients with prosthetic joint implants, prophylactic antibiotics are not recommended prior to dental procedures to prevent prosthetic joint infection. For patients with a history of complications associated with their joint replacement surgery who are undergoing dental procedures that include gingival manipulation or mucosal incision, prophylactic antibiotics should only be considered after consultation with the patient and orthopedic surgeon. The orthopedic surgeon makes the determination for the necessity of antibiotic prophylaxis. As a reminder, to assess a patient's medical status, a complete health history is always recommended when making final decisions regarding the need for antibiotic prophylaxis.
The clinical reasoning for the changes in the recommendation for joint replacements includes the following:
• There is evidence that dental procedures are not associated with prosthetic joint implant infections.
• There is evidence that antibiotics provided before oral care do not prevent prosthetic joint implant infections.
• There are potential harms of antibiotics including risk for anaphylaxis, antibiotic resistance, and opportunistic infections like Clostridium difficile.
• The benefits of antibiotic prophylaxis may not exceed the harms for most patients.
• The individual patient's circumstances and preferences should be considered when deciding whether to prescribe prophylactic antibiotics prior to dental procedures.
In the past, according to the American Heart Association, patients with nearly every type of congenital heart defect needed to receive antibiotics one hour before dental procedures or operations on the mouth, throat, gastrointestinal genital, or urinary tract. However, in 2007 the American Heart Association (AHA) simplified its recommendations. Today, according to the 2017 AHA guidelines, antibiotics before dental procedures are only recommended for patients with the highest risk of infective endocarditis, those who have:
• A prosthetic heart valve or who have had a heart valve repaired with prosthetic material.
• A history of endocarditis.
• A heart transplant with abnormal heart valve function
• Certain congenital heart defects including:
° Cyanotic congenital heart disease (birth defects with oxygen levels lower than normal), that has not been fully repaired, including children who have had a surgical shunts and conduits.
° A congenital heart defect that's been completely repaired with prosthetic material or a device for the first six months after the repair procedure.
° Repaired congenital heart disease with residual defects, such as persisting leaks or abnormal flow at or adjacent to a prosthetic patch or prosthetic device.
Preventive antibiotics are no longer recommended for any other congenital heart disease than the following conditions:
• Cyanotic congenital heart disease (birth defects with oxygen levels lower than normal), that has not been fully repaired, including children who have had a surgical shunts and conduits.
• A congenital heart defect that's been completely repaired with prosthetic material or a device for the first six months after the repair procedure.
• Repaired congenital heart disease with residual defects, such as persisting leaks or abnormal flow at or adjacent to a prosthetic patch or prosthetic device.
Under the current guidelines, patients who have taken prophylactic antibiotics routinely in the past but no longer need them prior to dental treatment include patients with:
• Mitral valve prolapse
• Rheumatic heart disease
• Bicuspid valve disease
• Calcified aortic stenosis
• Congenital heart conditions such as ventricular septal defect, atrial septal defect, and hypertrophic cardiomyopathy
Furthermore, taking antibiotics just to prevent endocarditis is not recommended for patients who have procedures involving the reproductive, urinary, or gastrointestinal tracts.
For patients who are not sure whether they need to be premedicated, a telephone consultation with the physician is necessitated. Before the conclusion of the consultation, the dentist should ask for written documentation from the physician in the form of a letter to be kept with the patient's chart. When a patient forgets to premedicate, the antibiotic should be given in a single dose 30 to 60 minutes before treatment. This time period is recommended so that there will be high blood levels of antibiotic at the time bacteremia occurs; if the antibiotic accidentally is not administered, the dosage may be given up to 2 hours after the procedure. However, it is important to note that the recommendation is to give the antibiotics 30-60 minutes before treatment. Infective endocarditis is one of the most serious complications that can occur following a dental appointment. Although the percentage of affected patients surviving endocarditis has greatly increased through the years, prevention is the best way to manage the disease.
AGING OF THE DENTAL TISSUES
The enamel of our teeth endures both chemical and morphological changes through the years. These tissues become less hydrated and experience superficial increases in fluoride content with age, especially with the uses of dentifrice and tap water. Thickness of the enamel changes over time, especially on the facial, proximal contacts, incisal edges, and occlusal surfaces due to the many chewing cycles and cleaning with abrasive dentifrices. The disappearance of the outer layer of enamel over time changes the way in which the tissue interacts with acidic solutions. With age, the volume of dentin increases through the apposition of secondary dentin on the walls of the pulpal chamber and because of caries or dental excavation. Aged dentin is more brittle, less soluble, less permeable, and darker than it was earlier in life.
The size of the pulp chamber and volume of the pulpal tissue decreases with reparative and secondary dentin. The odontoblastic layer surrounding the pulp changes progressively from a multilayer organization of active columnar cells to a single layer of relatively inactive cuboidal cells. Calcification of the nerve canals increases with age, and the cementum volume within the alveolus increases gradually over time, notably in the apical and periapical areas.
Aging affects the potential diagnosis and subsequent treatment planning by altering the radiographic appearance of teeth. Teeth that appear pulpless usually are not, making the instrumentation during an endodontic procedure a challenge. Furthermore, radiographic images of older teeth that appear to predict an impending coronal pulp exposure may be misleadingly pessimistic. Apposition of apical cementum has been shown to alter the association between the apical foramen and the radiographic apex.
DENTAL TREATMENT
The incidence of root caries in the older adult has been estimated at approximately 1.6 root surfaces per 100 root surfaces at risk. The nature of the root caries appear to be more severe in males and most likely to affect the molar regions (Figure 1 and Figure 2). Significant factors associated with root caries include decreased salivary flow, impaired manual dexterity, and systemic conditions requiring medications that decrease salivary flow. Other risk factors influencing the higher incidence of root caries among the older patient include abrasion at the cementoenamel junction, fixed bridgework, removable partial dentures, long-term institutionalization, and soft diets consisting of refined sugars and sticky, fermentable carbohydrates. Root caries prevention and therapy include application of topical fluoride, dietary counseling, plaque control, and prevention of gingival recession.
Restorative dental treatment for the older patient must take into account dental, functional, and medical considerations if the quality of care provided is to be equal to that of younger patients. The dental team must keep in mind the changes that have taken place in the tooth structure as well as the impact of medical conditions when planning and delivering restorative care to their patients. Due to the nature of increased brittleness of the clinical crown, numerous pre-existing restorations and general recession, the dental practitioner may be especially challenged when treatment planning the restoration of carious lesions in the mouth of an older patient. Highly reinforcing restorations such as onlays and full crown coverage enhance the durability and strength and reduce the likelihood of non-restorable tooth fractures. Extending the crown preparation apically and placing the margins subgingivally is indicated occasionally to reduce the likelihood of developing primary or secondary and recurrent root caries on the exposed surfaces of the teeth. Smoothing the compromised root surface, improving access to oral hygiene, and applying a topical fluoride may successfully treat shallow root caries. Deeper compromised surfaces need to be cleaned out and restored with a restorable dental material.
There are four types of materials currently used to restore carious lesions on the root surfaces: amalgam; composite resins; auto-cured and dual-cured glass ionomer cements; and dentin bonding materials. However, restorative techniques and materials developed for and proven in the mouths of younger patients should not be assumed to perform identically in the older dentition.
Amalgam is a restorative material that requires mechanical undercuts and adequate condensation, two factors that may be difficult to meet when restoring carious root lesions. Due to the lack of fluoride release, esthetics, and the need for conventional retention form, amalgam is not always the material of choice for root area restorations. However, amalgam works remarkably on surfaces that act as anchor teeth for removable partial dentures.
Retention of currently available restorative materials should continue to use macromechanical strategies even as micromechanical and chemical adhesive mechanisms provide bonding to dentin that amplifies tensile strength and refines the marginal seal. Undercuts and increased surface area through grooves and boxes enhance the restorative success of bonded restorations and can be used more freely in older teeth without risking pulpal involvement. Pulpal sensitivity is usually greatly decreased or lacking altogether in older teeth. Most restorative procedures can be done with no discomfort in the absence of local anesthetic or with minimal infiltration of anesthetic, with the patient's consent. Excluding the anesthetic is especially advantageous for patients with neurological diseases such as stroke or dementia, as they may traumatize their tissues inadvertently after the appointment while the soft tissues are still anesthetized. The use of a local anesthesia reversal agent is helpful in these situations.
Currently, glass ionomer cements are the preferred restorative materials for carious root lesions because they provide a long-term seal against microleakage, continuous fluoride release, require minimal cavity preparation and are well tolerated by the pulp and gingival tissue. A sandwich technique involving the use of glass ionomer cements as a liner under resin composite restorations optimizes the benefits of both materials. The concomitant use of dentin bonding agents allows for more conservative tooth preparation and improved marginal integrity. Acid etching of enamel is more effective in the older tooth, requiring a shorter time for a retentive bond, and should be used with all types of restorative materials. Research states that there is little need to place a base under a restoration in the older patient other than to create an environment toxic to remaining bacteria when, to avoid an exposure, the clinician has made a decision to leave behind infected dentin. Most bonding agents work well as liners and therefore there is little need for application of a separate product.
Dental restorations should be designed to be proactive as well as reactive with respect to the increasing prevalence and extent of root exposure. Approaches should be targeted specifically toward root caries, and periodontal and restorative therapies aimed toward maintaining gingival height in order to lower the number of potential sites susceptible to root caries attack. Patients with recurrent root caries need to be educated about diet, use of fluoride, recare frequency, and other preventive measures. When caries are present, perigingival margins should be extended slightly subgingivally whenever feasible, in order to reduce the chance of recurrence. Restorative materials for carious lesions on the root surfaces that feature bonding to the dentin and enamel will minimize marginal leakage, but their optimal performance requires careful isolation during the procedure.
To harmonize with adjacent, unrestored teeth, esthetic restorations should use lower-value shades, smoother facial contours, flattened incisal and interproximal areas, and overall greater translucency. Strategically placed fine opaque white lines can mimic natural blemishes found in older enamel and intensify the perceived translucency of the neighboring less-opaque restorative material. Incisal edges enhanced with violet stain effectively imitate the appearance of enamel worn thin by use, without requiring the physical reduction of the facial-to-lingual dimension that could undermine strength and reduce the lifetime of the restoration.
Bleaching of the older dentition can be done the same as for younger teeth, providing that all areas of decay and root sensitivities are filled and the radiographic examination does not show any pulpal involvement. The patient needs to be informed that amalgam, resin, gold, and porcelain restorations as well as denture and partial teeth will not bleach, and that some anterior restorations may need to be replaced with a more esthetically pleasing shade when the bleaching process is complete. For the patient with a removable appliance, an impression for the bleaching trays should be done with the appliance out of the mouth. There are many brands of take-home bleaching materials available to dental offices, with varying concentrations. A 10% - 16% carbamide peroxide solution is usually sufficient for bleaching of the darker dentition. Written instructions should be given along with the verbal instructions, and a follow-up telephone call or office visit a week after receiving the materials is helpful for the patient. Approximately two weeks should be allowed after completing bleaching before progressing with any resin bonding procedures in order to allow for any rebound in the shade of the bleached teeth.
Recent studies have shown that a significant number of dental practitioners have increased the length of their typical dental appointment. Although appointments of less than 60 minutes are still widespread, many practitioners now schedule 1- to 3-hour treatment sessions. Dental therapy is stressful to the patient, and longer appointments are more stressful than shorter appointments. Medically compromised patients are more likely to react adversely when subjected to longer treatment times. Patient anxiety remains an important factor in the delivery and outcome of dental care. Three tips for calming an anxious patient include remaining calm, reassuring the patient continuously, and making sure the anesthetic is effective when being used. Patients can be reassured by providing information about the treatment, allowing time for questions, not rushing to begin treatment, and paying attention to the individual's needs and feelings while providing an environment conducive to communication, understanding, and patient education.
PATIENT POSITIONING FOR COMFORTAND EFFICACY
Aging patients may have impaired physical mobility or sensory perception. Breathing patterns may be irregular, causing the patient to become easily winded. Escorting the patient slowly down the hall, matching their gait, and offering an arm for them to grab onto will help make the patient feel a bit more relaxed. For those traveling by a walker, walk ahead of the patient slowly. For those traveling by wheelchair, slowly push the chair to the treatment room and, depending upon the dental chair position, either back into the room or go forward through the doorway. Line the wheelchair up with the dental chair for easier transfer of the patient.
Some older adults find it difficult to sit for extended periods in the dental chair, or may object to being placed in a supine position, while others have difficulties with support and balance. Pillows or rolled towels may be placed underneath knees or behind necks and backs to prevent muscle spasms and provide additional support during treatment. Always ask the patient before moving the chair or adjusting supports, and frequently ask if the patient is still comfortable. Most patients can be treated successfully within the dental office with a few adaptations. Ideally, patients should be treated in the dental chair, but occasionally a patient in a wheelchair may be unable to transfer to the dental chair. In this case, the dental team can move the wheelchair as close to the dental unit as possible, and work standing up. Patients who remain in the wheelchair during treatment will need additional head support in the form of a portable headrest. For those patients treated in the dental chair, care must be taken at the completion of the appointment so the patient is not brought abruptly from a supine position to an upright sitting position. Orthostatic hypotension is a frequent occurrence in the older adult with quick positional changes. Allowing the patient to sit for a minute or two before escorting the patient to the reception area helps them regain their balance.
MANAGEMENT FOR PARTICULAR CONDITIONS
Alzheimer's disease
Alzheimer's disease is a type of dementia that is progressive and a chronic degeneration of cognitive function. The etiology is unknown and onset can begin as early as the fourth decade of life. In most cases, the progression of the disease is a slow deterioration lasting for 15 years or more. The disease can be divided into three stages:
Stage 1- the mild impairment or forgetfulness phase (2-4 years), in which the individual experiences noticeable changes in mood, loss of judgment and memory. Neglect of appearance, denial of deficits, and inability to perform complex routine activities is usually noted.
Stage 2 - the moderate impairment or confusional phase (2-10 years), in which the individual has increased episodes of extreme irritability and confusion. Wandering, constant motion with repetitive movements and unclear speech is usually noted.
Stage 3 - the severe impairment or dementia phase (1-3 years), in which the individual becomes severely disoriented and behavior difficulties become quite apparent. Confinement to bed or chair, incontinence, seizures, and a higher susceptibility to infections is common.
The goals of dental treatment for these individuals are to restore and maintain oral health, and to prevent the progression of oral disease. Due to the degenerative nature of this disease, the first visit represents the best cognitive functioning level of the patient. For this reason, the treatment plan should be designed to restore oral function quickly and to establish an intensive prevention program. Appointment times should be scheduled with an awareness of the patient's best time of day. The presence of a familiar caregiver in the treatment room will often ease the patient's fears.
Arthritis
Rheumatoid arthritis is a systemic disease of unknown etiology, characterized by inflammation of the joints that become chronic and progressive. It can often cause gross deformities and limited motion in the involved joints. The temporomandibular joint may be affected by this disease, resulting in limitations in opening of the mouth and holding open for extended periods. It is important to be aware of what type of medications this patient may be taking, as aspirin, which is most commonly prescribed for rheumatoid arthritis, can extend bleeding times. The patient may also be taking corticosteroids, which may cause a potential drug interaction with some dental drugs. It is best to consult with the patient's physician before prescribing any medications postoperatively. Dental appointments should be kept as short as possible and preferably during the latter part of the day, when gradual use of the joints and muscles throughout the morning has diminished stiffness.
Cardiac conditions
Cardiovascular disorders comprise a variety of conditions including acquired and congenital heart disease, such as atherosclerosis, congestive heart failure, and rheumatic heart disease. These patients may be taking a variety of drugs, and treatment should be planned in collaboration with the patient's physician. Patients with cardiovascular disorders have an increased predisposition to developing bacterial endocarditis and may be required to take prophylactic antibiotic therapy before certain treatment procedures. Individuals who are treated with a monoamine oxidase inhibitor for hypertension should not receive a local anesthetic containing epinephrine, nor should the use of vasoconstrictors for gingival retraction and hemostasis be used.
Diabetes
According to the Centers for Disease Control and Prevention in 2020, more than 34.2 million American have Diabetes and another 88 million are prediabetic and on course to having type 2 diabetes within five years. Over 25% of persons 65 and older have diabetes, and the percentage has remained at this rate for the past decade. Diabetes mellitus is a disease of metabolic dysregulation that develops from either a deficiency in insulin production or an impaired utilization of insulin; there is no cure. There are two types of diabetes, and either type may occur at any age. Type I diabetes is also known as insulin dependent diabetes (IDDM). It was formerly called juvenile-onset diabetes and results from the destruction of insulin producing cells of the pancreas, which may involve autoimmune or a virally-mediated destructive process. Control of this form of diabetes is dependent upon the administration of insulin. Type II diabetes, also known as non-insulin dependent diabetes (NIDDM), was formerly called maturity-onset diabetes. It results from either defects in the insulin molecule or from altered cell receptors for insulin and represents insulin resistance rather than deficiency. In the majority of the cases, Type II is controlled through diet and oral medication. Until recently, Type II has been seen as a disease of genetic susceptibility triggered by environmental factors. The environmental trigger is the change in lifestyle to inactivity and in diet to overalimentation, especially more carbohydrates and fats. The fundamental biochemical basis of diabetes is still unknown, and Type II is not just a single entity. There are several forms of late onset, Type II diabetes being researched. Currently, there is a global epidemic of Type II diabetes with morbidity and mortality of an enormous magnitude. In both cases, the oral manifestations are similar and include:
• Acetone breath; this has the odor of decaying apples or stale cider
• Alveolar bone loss; severe loss of the supporting bone structure and the periodontal ligaments results in the loosening of the teeth
• Dehydration of the mucosal soft tissues; this results from the diminished production of saliva; the dryness is uncomfortable and the tongue may have a burning sensation
• Delayed healing; this is accompanied by a greater susceptibility to infection
• Irritated gingiva; these can be red, swollen, and painful; as the age advances, the gingiva becomes fibrotic and hypovascular
• Toothache in clinically sound teeth; this is due to the arteritis occurring throughout the body
Diabetes mellitus is frequently associated with a classic group of complications including cardiovascular disease neuropathy, periodontal disease, and retinopathy. Periodontal disease is considered the sixth greatest complication of diabetes. The incidence of periodontal disease appears to increase in the diabetic population with age, and is more severe in those individuals with other systemic complications. Prolonged exposure to hyperglycemic conditions results in decreased fibroblast proliferation and collagen synthesis, and basement membrane alteration and thickening, to name a few.
Appointment scheduling of the diabetic patient is crucial because diabetics receiving insulin therapy must consume carbohydrates every three hours during their waking hours. It is best to give these patients early morning appointments so they are not kept waiting, because the stress of waiting may result in an adverse reaction. The patient should be advised to eat and adjust their insulin intake before the appointment. For the diabetic who wears a removable appliance, care must be taken to check the appliance for pressure points, because any pressure or roughness from the appliance can result in gross inflammation of the mucous membranes.
Parkinson's disease
Parkinson's disease is a chronic, progressive disorder caused by the pathological changes in the basal ganglia of the cerebrum, resulting in the deficiency of dopamine. Characteristics include excessive salivation and drooling, involuntary tremors, loss of postural stability, muscle rigidity, and slowness of spontaneous movement. Tremors in lips and tongue, and difficulty swallowing are common, making treatment somewhat of a challenge. Adaptive aids and enlarged toothbrush and floss handles should be provided to these individuals to facilitate self-care and consequently self-determination whenever possible. Special consideration is needed when positioning the patient for treatment, and at the conclusion of treatment when the dental chair is brought to an upright position. Balance and equilibrium are often affected, either by medications or the disease itself. It is crucial to remember that a patient with Parkinson's usually has no impairment in intellectual function. Approximately 1% of seniors have some form of Parkinson's.
Sensory impairment
A patient who is visually or hearing impaired will often come to the office with a friend or family member who plans to aid with communication. It is important to allow the patient to be as independent as possible. A visually impaired patient communicates through other senses, such as hearing, smell, taste, and touch. It is very helpful and beneficial to the patient to have the treatment explained as the appointment progresses and mention to the patient when something may taste unpleasant. Inform the patient before moving the chair position. It may also be helpful to touch the patient reassuringly as the chair is being positioned.
A hearing-impaired patient sometimes has less obvious needs. They may or may not read lips, and may nod or smile and appear to understand out of politeness. If the patient does read lips, stand in front of the patient, and speak slowly without over enunciating the words, with your mask removed. Instructions should be kept as simple as possible. It is best to have a pen and paper handy to aid with communication if needed. Some patients may come to the appointment with an individual who knows sign language. In this situation, speak to the patient directly, with your mask off, while the signer is off to the side signing. When giving post-operative instructions, be sure to include a written copy for the patient.
Loss of speech acuity may account for some of the difficulty a hearing-impaired individual may have in adjusting to speaking with a new removable appliance. The "hissing" sound of "s" will be particularly difficult. If the patient is compliant, after the appliance is properly adjusted to permit proper sound production, have the patient practice difficult sounds until he or she is able to make an acceptable sound. Since the patient can no longer depend on auditory self-monitoring of their speech for self-correction, he or she must learn to judge production by the placement and feel of the tongue against the appliance. Allowing a little extra appointment time for both visually and hearing impaired patients is helpful to both the patient and the dental team.
Stroke
A cerebrovascular accident (CVA) or stroke is the result of damage to part of the brain and is usually caused by a sudden interference of the blood supply to the brain. Although stroke can occur at any age, the greatest incidence is among adults 60 years of age and older. Severity of the stroke varies from one individual to another with little or no paralysis to complete paralysis. On occasion, the part of the brain that controls speech is affected. Stroke patients may have difficulty in swallowing, chewing, or wearing of removable appliances. Maintenance of oral hygiene often times diminishes. Stroke patients should be treated as an adult with respect. Temporary personality changes and display of behavior usually result from injury to the portion of the brain that controls these emotions. Appointment times need to be short with frequent rest periods, as the patient will tire quickly. Modification of toothbrush and floss handles may be needed, depending on the severity of the injury.
Xerostomia
Xerostomia refers to the sensation of a dry mouth. Various factors can play a role in the patient's perception of xerostomia. Prescription medications, surgical intervention, chemotherapy, and radiotherapy treatment of cancer intensifies changes in salivary function. Commonly administered medications associated with xerostomia include anticholinergics, antihistamines, antihypertensives, antimetabolites, antiparkinsonians, diuretics, narcotic analgesics, quinolones, sedatives, and tranquilizers. Other common factors including aging, diabetes, mouth breathing, smoking, and Sjogren's syndrome aggravate the condition. Saliva performs a variety of functions in maintaining dental health, such as:
· Antibacterial and antimicrobial action
· Assistance in swallowing
· Buffering of acids produced by oral bacteria
· Lubrication of tissues and aids in the breakdown of food
· Remineralization of tooth surfaces
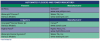
Xerostomia affects women more frequently than men, and is more commonly found in older individuals. Once the diagnosis of xerostomia or salivary gland hypofunction is made and the possible causes confirmed, treatment for the condition usually involves the use of artificial saliva substitutes, and chewing gum and/or toothpaste formulated to treat xerostomia. In the more severe cases, such as patients receiving radiotherapy for cancer of the head and neck, or patients with Sjogren's syndrome, a systemic cholinergic stimulant may be administered if no contraindications exist. In all cases, good hydration is essential, with water being the drink of choice. Caffeine should be avoided as it is dehydrating, as should sugared candies or cough drops, which aid in root caries.
Due to the complex nature of xerostomia, management by the dental team is extremely difficult. Although the artificial saliva products do not stimulate salivary production, the use of these products is highly recommended for patient comfort. Xerostomia not only affects the mucous membranes of the oral cavity, it can greatly affect the rate of caries. Many of the products on the market are balanced in terms of pH so that no additional risk of dental caries occurs. In patients with moderate to severe xerostomia, or those individuals with a susceptibility to caries, saliva substitutes can be used in conjunction with topical fluoride treatment programs designed by the dentist to reduce the incidence of caries. Salivary substitutes may provide an allergic potential in patients who are sensitive to some of the preservatives present in the artificial saliva products. Furthermore, there is a risk of microbial contamination by placement of the salivary substitute container in close contact with the oral cavity. Patient education regarding the use of saliva substitutes is essential. The patient with chronic xerostomia should be educated on the need for regular recare visits, optimum performance in home care, and the need to re-evaluate oral soft tissue pathology and any changes that potentially could occur long-term. (See Appendix 4: Artificial Salivary Substitutes)
HOMEBOUND DENTISTRY
Most operative techniques that are used in the dental office can be adapted and employed to homebound care of individuals confined to their homes, nursing homes, and hospitals. An assistant will usually travel with the dentist. The patient should receive the same consideration and quality of care given to patients in the dental office. Portable equipment is compact, lightweight, and relatively self-contained. The equipment should include a means of positioning the patient's head, adequate light, handpieces, and other instruments and materials needed for treatment. Portable radiographic material is also available. Treatment sessions should be shorter than those in the office because the home-confined individual may tire more easily.
Home care aids and suggestions
The instruction and home care regime of the physically challenged patient will depend on the type and severity of the disability. The individual who has a mild physical or mental disability can be taught a simple brushing technique, such as the Fones or press and roll method. Bicycle grips, tennis balls, and Styrofoam molds with the handle of the toothbrush placed inside can be used as alternative brush handles for the patient with decreased manual dexterity. (Figure 3) There are several types of toothbrushes on the market and some can be personalized to meet patient needs. By bending a plastic handle under hot water, the angle of the brush can be adjusted to counterbalance the disability. Supervision by the parent or caregiver may be required at one of the daily brushings, preferably the evening one. The more seriously impaired patient may be instructed in the use of an electric toothbrush. (See Appendix 5: Mechanical Toothbrushes) The patient should be encouraged to brush his or her own teeth during the day. This will help to reinforce the concept that the teeth should be cleaned twice daily and to give the patient a sense of responsibility for his or her own care.
If the patient has the necessary interest and skills, flossing can be taught or reinforced. A floss holder can be a useful device if the patient's manual dexterity is limited, or a mechanical flossing device is also acceptable. Floss holders can also be inserted into alternative handles. (See Appendix 6: Automated Flossers)
Fluoride Treatments
For the caries-prone patient, the use of fluoridated toothpaste is essential. It is recommended that older adults use either a monofluorophosphate (0.76% MFP; Colgate) or sodium fluoride paste (0.24% NaF; Crest). These two dentifrices contain 1000-1100 ppm fluoride. For patients with extensive dental work or for those with a higher decay rate, over-the-counter and prescription mouth rinses, gels, or toothpastes may be indicated. (See Appendix 7: Fluoride Therapy)
Concentrated topical fluoride applications following dental prophylaxis have been evaluated and approved by the American Dental Association and the Food and Drug Administration. There are three types of fluoride in-office delivery systems considered safe and effective:
• 8% Stannous Fluoride (SnF2) - contraindicated for patients with anterior demineralization due to the staining potential
• 1.23% Acidulated Phosphate Fluoride (APF) - has a pH 3.5, contains hydrofluoric acid, and has a potential to etch porcelain and glaze surfaces; contraindicated for patients with crown and bridge work (a sodium fluoride can be used instead)
• 2.0% Sodium Fluoride (NaF) - safe for use with porcelain and resin restorations
For the older individual with little or no decay, one or two fluoride applications annually following a prophylaxis is recommended. For patients with more extensive decay, a more aggressive regimen of four to six applications over four to six weeks to control the caries process may be in order. Multiple surface root caries can be managed as an infection using a combination of an antimicrobial agent (0.12% chlorhexidine) to control bacterial growth and topical fluoride to protect the exposed root surfaces. While chlorhexidine is primarily used as an antimicrobial agent for treating gingivitis and periodontal disease, it is very effective in controlling and eliminating microorganisms responsible for caries formation, specifically streptococcus mutans and the actinomyces organisms.
CONVEYING POST-TREATMENT INSTRUCTIONS
Communication with patients, especially geriatric patients, is the most essential element in a successful dental practice. Communication is more than talking; it is listening and understanding. For the hearing-impaired individual, a clipboard with a piece of paper and a pencil is especially helpful for conveying messages. Written post-operative instructions are recommended, in addition to verbal instructions. The patient may be too fatigued from the treatment to understand clearly what they are being told. For hearing-impaired individuals, it is especially helpful to have instructions written out. If the treatment was particularly taxing for the patient, a quick telephone call by a dental team member in the early evening is a nice gesture.
When scheduling dental appointments, it is essential to ask the patient what time of the day they prefer. Special circumstances and patient needs should be taken into consideration. Some older patients have frequent dosing schedules for their medications, while others tend to do better at different times of the day. Patients with arthritis tend to do better in the afternoon. When scheduling an appointment at the completion of treatment, it is helpful to provide the patient with a clearly written appointment card listing the date, day, and time of their next appointment. When a series of appointments is needed, it is helpful to the patient if the appointments are scheduled on the same day of the week and time of the day. If the patient is making an appointment over the telephone and the appointment is over a week away, mail an appointment card to the patient as a friendly reminder. Confirmation calls the day before are also helpful reminders to these patients.
SUMMARY
With the ever-increasing elderly population, new challenges will be presented as this group of individuals continues to live longer, retain more of their natural dentition, and present with specific types of needs for preventive and restorative care. Treating and meeting these requirements of our older patients in the dental office is a challenge at times, but truly a rewarding experience. Dental team members can better prepare themselves to meet these demands with a thorough knowledge of the needs and treatments specific to this demographic.
References
National Diabetes Statistics Report 2020 https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf Accessed March 29, 2020.
Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: U.S. Department of Health and Human Services; 2014.
Cottone, James A., Terezhalmy, Geza T., and Molinari, John A Practical Infection Control in Dentistry. Media, PA., Williams & Wilkins, 2009
Malamed, Stanley F. Medical Emergencies in the Dental Office. St. Louis, Mosby- Year Book, Inc., 2007
Aging and dental health. http://www.ada.org/en/member-center/oral-health-topics/aging-and-dental-health - Accessed August 16, 2017
Dental Health and Heart Health http://www.heart.org/HEARTORG/HealthyLiving/Dental-Health-and-Heart-Health_UCM_459358_Article.jsp#.WaiUbLhBGt8 - Accessed August 10, 2017
http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/TheImpactofCongenitalHeartDefects/Infective-Endocarditis_UCM_307108_Article.jsp#.WaiNFbhBGt8 - Accessed on August 20, 2017
http://www.mouthhealthy.org/en/az-topics/a/joint-replacement - Accessed on August 20, 2017
Statistics about diabetes. American Diabetes Association. http://www.diabetes.org/diabetes-basics/statistics/ - Accessed August 1, 2017
Diabetes facts. Centers for Disease Control and Prevention. https://www.cdc.gov/features/diabetesfactsheet/ - Accessed August 1, 2017
Stroke facts. Centers for Disease Control and Prevention. https://www.cdc.gov/stroke/facts.htm - Accessed August 2, 2017
"Dental Management in the Medically Compromised Patient". Burgess, Jeff, DDS, MSD and Meyers, Arlen D., MD, MBA. http://emedicine.medscape.com/article/2066164-overview - Accessed August 19, 2017
Accessed August 10, 2017
Iacopino, Anthony M., DMD, PhD. "Maintaining Oral Health in the Aging Population: The Importance of the Periodontal-Systemic Connection in the Elderly". September 1, 2006.
http://www.dentistryiq.com/articles/gr/print/volume-1/issue-3/original-article/maintaining-oral-health-in-the-aging-population-the-importance-of-the-periodontal-systemic-connection-in-the-elderly.html - Accessed August 08, 2017
Darby, Michele Leonardi BSDH, MS and Walsh, Margaret M. RDH, MS, MA, EdD Dental Hygiene Theory and Practice. Philadelphia, W.B. Saunders Company, 2014
Jahn, Carol, RDH, MS. "Review of Automated Plaque Removal Products." The Journal of Practical Hygiene, Vol.9 number 5, September/October 2000; 48-52.
Murchison, David F., DDS, MMS. Xerostomia. 2017. http://www.merckmanuals.com/professional/dental-disorders/symptoms-of-dental-and-oral-disorders/xerostomia - Accessed July 31, 2017
Turner, Michael D., DDS, MD; Ship, Jonathan A., DMD, FDS RCS. "Dry Mouth and Its Effects on the Oral Health of Elderly People". Journal of the American Dental Association, September 2007
Volume 138, Supplement 1, Pages S15-S20.
"The Link Between Medications and Cavities". American Dental Association. http://www.mouthhealthy.org/en/adults-over-60/concerns - Accessed July 31, 2017
Scarlett, Margaret I., DDS, "Local Anesthesia in Today's Dental Practice". American Dental Assistants Association; 2014.
"Plaque Has Met Its Match". https://oralb.com/en-us/products/plaque - Accessed August 3, 2017
Sharma, Naresh C., BDS, DDS; Lyle, Deborah M., RDH, BS, MS; Qaqish , Jimmy G., BSc; Schuller Reinhard, MSc. "Comparison of Two Power Interdental Cleaning Devices on Plaque Removal". Journal of Clinical Dentistry, 2012.