You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
According to the National Institute of Health, there are over 100 million people missing teeth, and the need for implant dentistry is stronger than ever. The number of implants placed in United States increased 10-fold between 1983 and 2002 and continues to increase every year.1 Dental implants are the standard of care today to replace a missing tooth. It is critical for the dental team to be familiar with the dental implant procedures available today. Patients often ask the dental team members questions regarding dental treatment options and post-operative details. It is important to appear confident and up to date when talking to our patients regarding dental implants. Knowledge of the current procedures for implants is a must for anyone in the dental field.
Any patient with one or more missing teeth is a candidate for dental implants. By becoming knowledgeable about different implant options, dental professionals will be able to help patients make educated decisions regarding their dental needs.
HISTORY OF DENTAL IMPLANTS
Pre-osseointegration
Human skulls dating from 600 A.D. show that man attempted to implant carved shells into the lower anterior jaw. However, the first documented dental implant did not appear until 1809.2 Dr. Maggiolo reported this, but with poor success rate.3
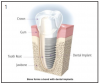
Teeth are anchored into the alveolar bone by the periodontal ligament. This ligament is a muscle attachment that acts like a shock-absorbing mechanism. Dental implants integrate directly into the alveolar bone, without a periodontal ligament.4 (Figure 1)
Prior to the era of osseointegration, there were various designs of dental implants and frameworks used to support dentures and partial dentures, called subperiosteal implants.Some of these were functioning well for several years, but most designs had an unpredictable success rate. The first of these type of framework was first described in 1949 by Drs. Goldberg and Gershkoff.5 There were a few complications associated with this method. Exfoliation of the bone connecting screws and exposure of the frame through mucosal perforation were a big problem. Because of these low success rates, this implant is no longer used today.
Almost 25 years later, in 1968, another dental implant concept was published by Dr. Small, called the transosseous implant.The name was derived because it transverses the lower jaw from the bottom to the top.6 This implant is inserted underneath the chin. A flat bone plate is fitted under the skin against the inferior border of the mandible. Several threaded posts project into the anterior mandible from the plate. Two to four of them go all the way through the mucosa, in the oral cavity to help fixate the denture prosthesis. Transosseous implants were machined from titanium or titanium alloy or a gold alloy. This procedure was done under general anesthesia in a hospital setting and it is quite invasive. Another downside was that bone loss around the posts with bleeding on probing was a frequent problem. This implant design is no longer used today because it was replaced by endosseous implant.
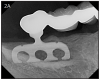
In 1966, Dr. Linkow presented the blade implant around the same time the transosseous implant was published.7 This was the first endosseous implant.(Figures 2A, 2B) This implant is inserted in the jaw by making a groove inside the jaw bone from the oral cavity. One or several posts area attached to the fin shaped plate, which anchors the restoration. The success rate for this implant was under 50%, and is no longer used today.8,9 The problem with it was that it got loose and infected eventually, and had to be removed.
Discover of Osseointegration
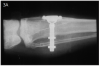
The concept of osseointegration was an accidental discovery in the early 1960s by professor Per-Ingvar Branemark. He was working on his thesis, studying bone regeneration in rabbits.10 He developed a titanium chamber to study wound healing. This device was implanted in the bone of a rabbit. At the end of the study, when he wanted to remove the chamber from the bone, it could not be removed, because the bone fused to the titanium surface. The bond was so strong that it could not be broken.11 (Figure 3A) He conducted several other experiments to confirm the idea that titanium could indeed integrate and become part of the bone. After this discovery, dental applications were the first that came to mind.
Branemark's first patient, Gosta Larson (Figure 3B) (1931-2006) was born with severe chin and jaw deformities, congenitally missing several teeth. He was treated in 1965, with the first implant supported bridge, in Gothenburg, Sweden. Four implants were inserted in the lower jaw, which integrated within 6 months. The prosthesis was then attached and that prosthesis was in place all his life.11
Following this first patient, Dr. Branemark did extensive clinical research and placed more implants with regular follow-up appointments. In the beginning, he only used fully edentulous patients and the procedure was done in a hospital setting. In 1977, Dr. Branemark presented his data to the Swedish government for its aid.12 He received the support needed to collect a large amount of data. The American Dental Association gave "full acceptance" for his dental implants, for a variety of uses, including: single tooth replacement, partial and fully edentulous bridges, implant supported overdentures.
Post-osseointegration
The Branemark system was introduced into United States in 1982. These implants were machined to be cylindrical in shape, with a screw type design. (Figure 4) Since then, other endosseous implant design have been introduced. Root-form dental implant devices today are characterized by four geometrically distinct types: basket, screw, solid cylinder, and hollow cylinder.
In order to improve the attachment of the bone cells to the implant surface, some companies have placed coatings on the implant surface. These coatings are Hydroxy-appatite (HA), and titanium plasma spray. Hydroxy-appatite was shown to attract bone cells, especially in areas where bone density is compromised.13,14 One of the biggest problems was that this coating can separate from the implant within the jaw bone, with the implant becoming loose and having to be removed.15,16
One way to increase the rate and success of osseointegration is to increase the surface area of the implant. This can be accomplished by spraying of the machined implant surface with liquid titanium or by dipping the implant in an acid that created microporosities. (Figure 5) Most of the implants available today have a surface that is porous to allow the bone cells to better attach to the implant surface.17 (Figure 6)
Many implant studies were conducted in the 1980s. Since then, numerous implant companies have appeared on the market. In order to sell implants in United States, the manufacturer needs to submit research and documentation to the Food and Drug Administration for approval, also known as the 510(k). Clinical testing is not required anymore for endosseous implants, since numerous studies have proven their success. (http://www.fda.gov)
RATIONALE FOR DENTAL IMPLANTS
As the baby boomer generation is aging, the need for dental implants increases. Implants offer several advantages over bridges and dentures. People who are missing teeth are compromised in chewing ability, speech, nutrition, facial appearance and self-confidence. When a tooth is lost, the surrounding bone start atrophying because it is not being stressed by masticatory forces. (Figure 7) Dental implants help maintain the bone profile and volume when chewing, by applying direct forces to the bone.18 These forces are essential in maintaining strong muscles and bone. Dentures or partial dentures have the opposite effect on the jaws. They create resorption of the bone because they only replace about 10% of the chewing strength of the teeth. This is not enough to maintain the bone, and we see a gradual loss of facial structure.19
Since chewing ability is reduced with dentures, atrophy of the muscles of mastication is seen, giving patients that sunken look of the cheeks. Implants also help keep these facial muscles, aiding in improved chewing ability. After receiving dental implants, many patients who have been missing teeth for a long time notice a natural "face-lift" effect when the muscles of mastication are being used again properly.
Those who are rehabilitating their mouth using dental implants, gain a priceless, new self confidence. Replacing missing teeth with implants is the best and closest to natural teeth. (Figure 8) Recipients are able to smile with confidence without worry of denture displacement or the gap or showing gaps when smiling.
Dental implants can last a lifetime if properly maintained and cleaned. The crown on top of the implant may need to be replaced for esthetic reasons, but the implant fixture in the bone, once integrated, is part of that patient's body.
ENDOSSEOUS IMPLANTS
There are several designs of root-form implants. The original Branemark implant was designed as a cylindrical implant. In the 1980s, a tapered implant came on the market. The advantage of this is that it has a "wedging effect" into the bone, allowing better initial stability, especially in softer bone. However, if too much pressure is exerted on the bone, then necrosis or death of the cells occurs, causing severe pain and implant loss within a month from surgery.20
Vent holes were also introduced toward the apex of the implant to allow for locking of the implant into the bone.4 This mechanical retention occurred as new alveolar bone grew into the vent holes inside the implant.
The thread design of the implant also varies from system to system. This can be self-tapping, meaning that the treads are sharp to cut their way through the bone (i.e. Nobel Biocare), or they can be non-cutting (i.e. Straumann). A self-tapping thread has the advantage that the osteotomy can be perfected as the implant is being placed, to allow for a close fit between the implant and the bone.
The implant platform can also have different shapes. It can be internal connection or external connection with the abutment. The original Branemak system had an external connection. The internal connection platform is the most preferred today in dental practices due to ease of handling. (Figures 9A-C)
Any clinician or dental assistant may be easily overwhelmed by the variety of implants available on the market today. The dentist should choose a dental implant system based on evidence based research. First, the system should prove reliability and a high clinical success rate for at least 5 years. It is also important to work with a reputable company, whose system is easy to use and versatile.4
Mini-implants
Mini-implants were introduced in dentistry as a temporary implant. These were placed to support a denture, or temporary prosthesis during the healing time following implant surgery.21,22 (Figure 10) Several manufacturers are now produce mini-implants for permanent restoration of missing teeth. The cost of mini-implants is approximately ¼ of the cost of a regular implant; however, the studies show a success rate of 60-70% during 5 years in function.
In 1983, Creekmore and Eklund started working with small-sized bone screws as anchors for elastics in orthodontics.23 These mini-implants, known as temporary anchorage devices (TADs), started getting more attention in orthodontics. They are usually placed and left there for 6-9 month, after which they are easily removed.24 TADs have a diameter of 1.2-2 mm and are especially useful to intrude and distalize molars and to close open bites.25
Zygomatic Implants
Certain patients do not have adequate amount of bone remaining in the maxilla, especially if they've had missing teeth for a long time or they were missing parts of the maxilla due to cancer. When posterior maxillary teeth are missing for a long time, the sinus can pneumatize or enlarge, and only a shell of bone remains between the sinus and oral cavities. Branemark wanted to find a treatment solution for these patients. He noticed that there's good quality bone in the zygomatic arch behind the maxillary sinus. The zygoma is situated at the upper and lateral part of the face and forms the prominence of the cheek. The initial 10-year study Branemark and his coleagues did with this implant found a survival rate of 94%.26
The lengths of the zygoma implants are 32.5 to 52.5 mm, which is 2 to 5 times the size of a regular implant. By using zygomatic implants, we can decrease the cost, the need for bone grafting and the morbidity necessary for implant rehabilitation. A multicenter study done in 1997, shows a success rate of 96.3%.26
PROSTHETIC OPTIONS
Single tooth
Most adults (70%) are missing at least one tooth.27 Developing a diagnosis and treatment plan for tooth replacement is the dentist's responsibility. However, all dental team members should be familiar with the different options, risks and benefits of replacing a single missing tooth.
There are 3 options to replace a single missing tooth:
1. A removable partial denture,
2. A 3-unit fixed bridge, or
3. An implant with a permanent crown.
Often times, an implant is the most conservative option to replace a missing tooth because it preserves the integrity of the adjacent teeth, as well as the bone structure in that area.
The removable partial denture (RPD) is the least expensive alternative out of the three treatment options. Many patients, however, do not like a removable prosthesis, especially if they suffer from severe gagging reflex. It is also uncomfortable when speaking and eating to most patients. The RPD needs to be removed at night to allow the tissues to breathe. As the jaw changes shape due to bone resorption, the RPD needs to be relined or changed, otherwise it gets loose.
A bridge involves replacing the tooth with a pontic which is connected by one or more crowns. This involves removing healthy tooth structure to create space for the thickness of the bridge. It is difficult to clean underneath a bridge, making them more prone to caries and periodontal disease. Also, the adjacent teeth are taking a heavier load, which increases their risk of root fracture. If a problem develops with one of the teeth supporting the bridge, then the entire bridge needs to be removed. Studies show up to 50% failure rates from 10 to 15 years in function.28
An implant most closely replicates the feel of a natural tooth. Once it is osseointegrated, many patients cannot differentiate an implant from a natural tooth. Furthermore, dental implants do not decay or need a root canal. Even though the cost is slightly more than a bridge, it is a great investment for the future, as implants usually last longer than a bridge. A 10-year report on posterior single implants shows a success rate of 97%.29 Once an implant is placed, an integration/healing time of approximately 4 months is necessary before final crown is placed. A temporary crown can be placed the same day the implant is placed. (Figures 11A-E)
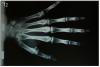
Young patient under 16-17 years old cannot receive dental implants. A hand-wrist radiograph is taken to determine if growth is complete . (Figure 12) If the patient is still growing, a resin-bonded bridge can be used as an option until their growth is complete and they are an implant candidate.
Partially Edentulous
When patients are missing multiple consecutive teeth, the best option for their replacement is dental implants. A bridge is not a preferred choice due to the long span of edentulism, causing excessive stress on the abutment teeth. A removable partial denture is the least expensive, non-surgical options. However, the anchor teeth supporting this prosthesis are subject to excessive forces. Studies show that up to 44% of the anchor teeth for the RPDs are lost early.30
There are two options when treatment planning partially edentulous patients:
1. Replace every tooth with an implant
2. Fixed bridge on several implants
Replacing every missing tooth with an implant may not be possible in every case, nor is it necessary to achieve good esthetics. However some patients want to have individual teeth. The hardest part about having individual teeth in the esthetic zone (anterior zone) is maintaining or creating the soft tissue architecture (papillae) predictably. The best results occur when implants are placed immediately following extraction, to preserve the gingival architecture.
Implant-supported bridges are a predictable and more cost-efficient way of replacing several missing teeth. As with a tooth-supported bridge, oral hygiene requires patients to floss underneath it. If they fail to clean under the implant-supported bridges, bone loss around the implants may arise, otherwise known as peri-implantitis.
Completely Edentulous
Many fearful dental patients avoid dental treatment, resulting in loss of teeth due to periodontal disease or extensive decay. With the advancements in today's dental implant technology, the dentist can insert implants immediately following extractions and deliver a fixed temporary full-arch prosthesis connected to the implants.31 Many patients are unaware of this option, and it is a preferred options since many of them are fearful of getting a denture. It is the responsibility of the dental team to educate the patients and become familiar with the new implant options.
After 4-6 months of healing, the final fixed bridge can be fabricated. This can be made out of acrylic reinforced by a CAD-CAM milled framework or out of porcelain with a titanium or zirconia framework. Both can achieve a great esthetic result, but porcelain is 3 to 4 times more expensive. Recent studies show that it is beneficial to splint implants together with an immediate, fixed temporary prosthesis because it decreases their risk of implant failure compared to using a removable transitional denture.19
As stated earlier, dentures replace only about 10% of chewing function. This causes digestive problems, due to an inability to chew food properly, also leading to malnutrition, due to an increase in consumption of softer, more processed foods. This inability to chew also results in atrophy of the alveolar arches due to lack of adequate pressure on the bone. When the denture is pressing on the mental foramen, then patients will experience pain and numbness of the lower lip. A good solution for these denture wearers is to place 2 to 4 implants in the mandible to stabilize the denture. The denture is then attached to the implants via snap-on attachments or a bar. (Figures 13A-C) According to the 2002 McGill Consensus Statement on Overdentures, mandibular two-implant overdentures are superior to conventional dentures in all clinical trials, even up to nine years in function.32
Since the maxillary arch is wider than the lower arch, and the bone in more porous, we need 4 to 6 implants for an overdenture. The advantage of having an implant-supported overdenture in the maxilla is that the palatal area can now remain uncovered. Having the palate open to the taste buds allows for an enhanced sense of taste. The overdenture can be removed by the patient and allows for thorough cleaning. Furthermore, it can give better lip support for patients who have lost bone in the anterior area, as compared to a fixed implant prosthesis. To restore the lip support, a flange is often necessary or extensive amount of bone grafting. We cannot attach a flange onto a fixed bridge because the patient will not be able to clean under it. (Figure 14)
DIAGNOSTICS
There are a few records needed to determine the different dental implant treatment options for the patient.
CT imaging
The standard of care today is to have a CT-scan prior to implant placement, to be able to visualize the jaw structure, position of the nerve canal and the quality and quantity of bone available. The CT scans have been used since 1973, and in dentistry since 1987. The latest technology in CT scans is cone beam, which offers less radiation than traditional x-rays. Medical CT scans use 40 to 60 times more radiation than cone beam CT scans in dentistry.19 Some dental offices have CB-CT scanners and dental assistants may be trained to take scans, similar to taking a panoramic x-ray. (Figures 15 and 16)
A radiographic guide may be given to the patient to wear during the jaw CT scanning procedure. This is made by the dental laboratory or in the dental office. Impressions of both arches are required to obtain mounted dental models. The correct occlusion relationship and the location of the teeth to be replaced with implants must be noted. The patient wears the radiographic guide when the CT scan is being taken. The radio-opaque markers from the radiographic guide are visualized on the CT scan, marking the position of the desired implant orientation. (Figure 17)
Treatment planning software
Different companies are providing a solution for accurately treatment planning the implant cases. Surgeons can simulate the placement of the implants prior to surgery. Once the implants are planned, a precise surgical guide can be fabricated, leaving little or no room for error.
SURGICAL PROTOCOL
Any licensed, properly trained dentist can place dental implants. It is important to understand the implant drilling protocol of the system to be used. A team approach will result in a smoother procedure and a happier patient.
Patients count on the dental assistants to answer questions regarding the procedure, usually when the doctor is out of the treatment room. The dental assistant can ease a nervous or confused patient. It is important for the dental team to have confidence and be comforting to the patients.
It is important to follow the sterile technique and preparation for any implant surgery. This will minimize the number of infections post-surgically. Pre-packaged, customizable, sterile implant kits can be purchased from different manufacturers. (Figure 18) While setting up for implant surgery, it is recommended to have a second assistant, who can get the supplies while the other assistant, wearing sterile gloves, prepares the treatment area. A proper surgical set up requires about 30 minutes. Several DVDs on how to properly set up the room are available on the market and are highly recommended, especially in the beginning.
The responsibilities of a surgical assistant are: setting up the treatment room, monitoring the patient, instrument exchange, retraction and keeping the surgical intraoral site as clean and visible as possible from blood and saliva. Ideally, a second assistant, non-sterile, can be a rover to obtain any necessary supplies outside of the sterile area.
A challenge with the implant surgical kit is that there are many small parts that are used intra-orally. (Figure 19) It is important to make sure none of the small drills and screwdrivers are aspirated by the patient. Screwdrivers can be ligated at the handle with a long piece of floss, for easy retrieval, in case they slip down the patient's throat.
Every implant company and each of their systems have a unique drilling sequence. Some are tapered and some are cylindrical. The cylindrical systems have a lot less drills in the kit. It is important to know the correct terminology for each part of the kit prior to first surgery. It is important to contact the company representative to become familiar with a particular implant system.
All implant handpieces are electric and need to be set up prior to start of surgery. The electric unit can be used with any implant drill system and is necessary to run the electric implant handpiece. Sterile saline bags are connected to the unit, which pumps saline to the handpiece at all times during drilling of the osteotomy. This acts as a cooling mechanism to prevent over-heating of the bone by the drill, which may result in implant failure.33 (Figure 20)
RESTORATIVE PROTOCOL
It is common practice today to have a temporary restoration immediately following implant placement surgery. Often times, especially in the esthetic zone, immediate abutments are being placed over the implant to support an immediate temporary restoration.
After 4 to 6 months of healing post-implant surgery, the final restoration is fabricated. An impression is taken either at implant level or at the abutment level to fabricate the final crown. The implant level impression records the implant position, so it needs to be very precise. An impression coping is screwed onto the implant to be transferred into the impression. The copings are utilized for a closed-tray technique or open tray technique. The closed tray technique may be used mostly with one implant, but the open-tray technique is used for multiple implants, when different implant angles exist. (Figures 21A, 21B) With either technique, the impression material most often recommended is polyether.34 Bite registration, shade selection, and opposing models are collected in the usual manner, as for crown and bridge cases.
There are different types, shapes and sizes of abutments that are either pre-fabricated by the manufacturer, or they are custom made by the dental lab. (Figure 22A) The choice of abutment is made by the esthetics desires, thickness of tissue around the implant, and the angle of the implant. What is important to remember is that all abutments are connected to the implant using a screw.
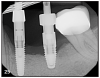
The crown can be cemented or screw retained over the implant. For multiple implant bridge or bar overdenture restorations, the framework try-in appointment is important prior to porcelain build-up or overdenture fabrication to ensure a passive fit, confirmed by an x-ray. Framework trial appointments require a minimal set-up. No anesthetic is required, but a screwdriver for that particular implant system is a must.
The implant prosthesis delivery appointment is similar to that of a crown and bridge. (Figure 22B) If the prosthesis is screw retained, then no cement is necessary and an occlusal filling material, such as composite, is necessary. After bite check, the patient is taught how to maintain the restoration. (Figure 22C)
PATIENT MANAGEMENT
Informed Consent
The informed consent form should be presented to the patient prior to the start of treatment that day. A good informed consent lists the doctor performing the treatment, the patient's name, the procedures being done that day, alternatives to today's treatment, risks involved in performing treatment, and also risks involved in not performing treatment. By signing the consent form, the patient understands the risks of treatment and any alternative options.
A preoperative discussion prior to the surgery date is completed to answer any additional concern that the patient may have. The informed consent should be presented by the doctor, but any member of the staff may be in charge to ensure that this form is signed. It is the doctor's responsibility to review the risks, benefits and alternatives with the patient, prior to an implant procedure.19
It is important to update the medical history prior to the surgical appointment, and to ensure that the list of medication is up to date. Patients who have had a recent heart attack, complications of diabetes, atrial fibrillation, immunosuppression need to be cleared by their physician for the implant surgery.
Pre-Surgical Preparation
The patient should have an oral hygiene appointment within the month of the surgery to minimize the amount of plaque present at the time of surgery. A 30-second rinse with 0.12% chlorhexidine mouth wash (Peridex) also aids in reducing the amount of bacteria present in the mouth at the time of surgery.35 This rinse should be done immediately prior to the start of surgery. Any removable appliances, such as partial dentures and retainers are removed from the patient's mouth prior to the rinse.
Prior to implant surgery, an antibiotic, and an anti-inflammatory are administered to the patient. Our preferred drugs of choice are 1 g of amoxicillin or 300 mg clyndamycin for the penicillin allergic patients, and also 600 mg of ibuprofen. If a patient cannot have ibuprofen (Advil), then 1000 mg Tylenol may be given for pain control.
Most implant surgeries may be performed without any type of sedation for the patient. However, if the patient requests sedation, then oral or IV sedation should be discussed. Oral sedation is a great option for short procedures, for the mildly anxious patient.
IV sedation is usually necessary for the highly anxious patient. Sedation should be discussed with the patient at the consultation appointment, as they need to make the proper arrangements for transportation.
Post-Surgical Instructions
Written post-operative instructions are given and reviewed with the patient prior to start of surgery and again after the surgery. The dental assistant must be comfortable to review these instructions with the patient. Patients must follow all medication protocols as prescribed, especially in taking the complete course of antibiotic. After surgery, the patients are advised not to smoke and not to exercise for one week, not to brush the surgical site for one week or until the sutures are removed. They are advised to rest, eat soft foods, rinse with salt water for the remainder of the day, then start with the prescribed antiseptic mouthwash the second day post-surgery. The patient is also given an ice pack to minimize swelling and a pack of sterile gauze to be used in case of bleeding.
Written post-operative instruction form may also include recommended homeopathic treatments. The most common of these is the Arnica Montana formulation. This product is commonly used after plastic surgery or any other trauma to reduce bruising and swelling. Arnica Montana homeopathic formulation comes in a gel, cream or sublingual pellets or tincture. Homeopathic formulations are very safe and can be found over the counter at most drug stores.
IMPLANT MAINTENANCE
Implants are different than teeth in the way they attach bone. They do not have a periodontal ligament, the muscle attachment that anchors teeth into the jaw. Therefore, even if the majority of bone is lost around the implant, no mobility is observed. The periodontal ligament (PDL) is a fibrous attachement that anchors teeth into the alveolus. A tooth would get loose and tender once this attachment is lost and bone loss is observed. Often times, peri-implantitis occurs with no symptoms. Therefore, it is imperative that regular dental prophylaxis appointments are scheduled every 3-6 months. If bone loss is detected early, the treatment can be administered quickly to restore health around the implants.36
Home care for dental implant restorations is the same as for natural teeth. Daily brushing and flossing are mandatory to remove plaque build-up, which can cause peri-implant mucositis (gingivitis) and worse, peri-implantitis. Patients rely on the dental team to give them instructions on how to clean their implants. It is important to be comfortable to show the patients how to use any new oral hygiene device that the doctor may recommend. (Figure 24A)
Recent studies have shown that oral irrigators may decrease inflammation and plaque better than string floss around dental implants.37 The oral irrigator has also been shown to be superior to the Sonicare Airfloss. For older patient with poor dexterity due to arthritis, for example, it may be difficult or impossible to clean using dental floss. An oral irrigator is recommended to use daily for these patients. (Figures 24B, 24C) Antiseptic rinses can be added in the reservoir to help reduce the inflammation in the tissues surrounding the implant.38
STERILIZATION AND HANDLING
The instruments used in the dental implant placement and restoration require special care. It is important to contact the manufacturer of the implant system used in your office for specific recommendations of that particular system.
All instruments and reusable drills should be cleaned using an ultrasonic cleaner, with an enzymatic wash. Prior to placing them in the ultrasonic, each drill needs to be cleaned manually with a small brush to remove any blood or bone particles. Some drills have an internal channel used for irrigation during surgery that acts as a cooling system. This channel inside the drills has to be kept free of blockages, by cleaning it after every surgery with an irrigation syringe and water. The screwdrivers and torque wrenches also need to be cleaned with a small brush. The torque wrench has to be taken apart if it was used in a surgical field, to remove any blood from the inside of the device. (Figures 23A-C) It is very important to put the drills back in their proper position in the surgical kit. To prevent rusting, it is important to dry the instrument before sterilization. Dry heat, autoclave, gas, and chemiclave techniques are all acceptable methods of sterilization.
The contra-angle handpiece must be cleaned first under running water and then carefully lubricated. The implant handpiece and motor should be sterilized based on manufacturer's recommendation.
IMPLANT COMPLICATION
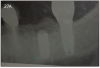
Dental implants are the best option to replace missing teeth. However, complications during treatment may arise, such as failure to integrate or bone loss while in function. (Figure 25)
Implant integration happens in 95%-99% of the cases. Occasionally, infections occur shortly after surgery. This is not surprising, considering that the oral cavity has a few billion bacteria. To minimize infections, it is important for the patient to take the oral antibiotic as prescribed, as well as use the antiseptic mouthwash for at least a week after surgery.
As mentioned earlier, dental implants require daily brushing and flossing, just like teeth. If plaque is allowed to build up around the implant, then peri-implant mucositis (gingivitis) or peri-implantitis may occur. (Figure 26) Signs of this condition include redness, bleeding when brushing and pocket depth increase in the area.
In older patient with a history of osteoporosis and/or aggressive periodontitis, there is a higher incidence of dental implant failure. Osteoporosis patients taking bisphosphonate drugs, such as Boniva and Zometa, which interfere with normal bone healing, may retard osseointegration of dental implants. Cancer patients who have received IV bisphosphonate treatment may develop a condition called Osteonecrosis of the Jaw (ONJ), where bone becomes exposed and infected. It is important to update medical history of patients regularly to identify these patients. Often times, for cancer patients using bisphosphonate medications, implants are contraindicated.39
Mechanical complications include loosening of screws, fractured screws and even fractured implants due to force overload. However, the incidence of fixture fracture has been reported to be less of an issue than that of tooth fracture10 (Figure 27A, 27B).
SUMMARY
Dentistry has advanced significantly in the area of dental implant technology. With the same-day tooth replacement options, patients can walk in with severely disease teeth, have them all removed, implants placed, and an immediate fixed temporary bridge secured in place immediately following implant placement.
Many patients struggle with ill-fitting removable full and partial dentures. Most patients are afraid of losing their teeth because they don't want to wear a denture. But now they don't have to. Furthermore, patients can be assured that dental implants have a high rate of success with a basic home care protocol and regular dental hygiene visits. (Figure 28)
Dental professionals can help patients understand the importance of having an implant vs a bridge. Patients count on the dental team members to educate them on all choices to replace missing teeth. Today, dental implants are and should be recommended as the standard of care for patients.
REFERENCES
1. Millenium Research Group Report: US Markets for Dental Implants, 2006.
2. Ring, M.E., Dentistry: An Illustrated History. . 1985: C.V. Mosby.
3. Ring, M.E., A thousand years of dental implants: a definitive history--part 1. Compend Contin Educ Dent, 1995. 16(10): p. 1060, 1062, 1064 passim.
4. Worthington Philip, L.B.R., LaVelle, W.E., Osseointegration in Dentistry. An Introduction. 1994: Quintessence.
5. Goldberg, N.I. and A. Gershkoff, The implant lower denture. Dent Dig, 1949. 55(11): p. 490-4.
6. Small, I.A., The mandibular staple bone plate. Its use and advantages in reconstructive surgery. Dent Clin North Am, 1986. 30(2): p. 175-87.
7. Linkow, L.I. and M.S. Mahler, Validating the endosteal blade-vent implant. Oral Health, 1975. 65(11): p. 16-23.
8. Kapur, K.K., Veterans Administration Cooperative Dental Implant Study, Part I: Methodology and Comparisons Between Treatment Groups at Baseline. . J Prosth Dent, 1987. 58: p. 499-512.
9. Kapur, K.K., Veterans Administration Cooperative Dental Implants Study, Part II: Comparisons of Success Rates and Periodontal Health Between Two Treatment Modalities. . J Prosth Dent, 1987. 62: p. 685-703.
10. Branemark PI, Z.G., Albrektsson T., Tissue-Integrated Prosthesis: Osseointegration in clinical dentistry. 1985, Chicago: Quintessence.
11. Biocare, N., The Story about an invention that makes people smile. 2005, Sweden: Nobel Biocare.
12. Branemark, P.I., et al., Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl, 1977. 16: p. 1-132.
13. Kay, J.F., Calcium phosphate coatings: understanding the chemistry and biology and their effective use. Compend Suppl, 1993(15): p. S520-5; quiz S565-6.
14. Gottlander, M. and T. Albrektsson, Histomorphometric studies of hydroxylapatite-coated and uncoated CP titanium threaded implants in bone.Int J Oral Maxillofac Implants, 1991. 6(4): p. 399-404.
15. Albrektsson, T. and L. Sennerby, Direct bone anchorage of oral implants: clinical and experimental considerations of the concept of osseointegration. Int J Prosthodont, 1990. 3(1): p. 30-41.
16. Levandowsky JA, J.C., Structural Failure of Osseointegrated Implants at the Time of Restoration: A Clinical Report. J Prosth Dent, 1989. 62: p. 127-129.
17. Tufekci, E., et al., Microstructures of plasma-sprayed hydroxyapatite-coated Ti-6Al-4V dental implants. Int J Oral Maxillofac Implants, 1997. 12(1): p. 25-31.
18. von Wowern, N. and K. Gotfredsen, Implant-supported overdentures, a prevention of bone loss in edentulous mandibles? A 5-year follow-up study. Clin Oral Implants Res, 2001. 12(1): p. 19-25.
19. Misch, C.E., Contemporary Implant Dentistry. 3rd ed. 2008: Mosby Elsevier. 1101.
20. Palma-Carrio, C., et al., Risk factors associated with early failure of dental implants. A literature review. Med Oral Patol Oral Cir Bucal, 2011. 16(4): p. e514-7.
21. Minsk, L., Interim implants for immediate loading of temporary restorations. Compend Contin Educ Dent, 2001. 22(3): p. 186-90, 192, 194, passim.
22. Mazor, Z., Using transitional implants for immediate fixed temporary prostheses. [Interview]. Dent Implantol Update, 2000. 11(4): p. 29-31.
23. Creekmore, T.D. and M.K. Eklund, The possibility of skeletal anchorage. J Clin Orthod, 1983. 17(4): p. 266-9.
24. Singh, K., et al., Temporary anchorage devices - Mini-implants. Natl J Maxillofac Surg, 2010. 1(1): p. 30-4.
25. Jae-Hyun Sung, H.-M.K., Seong-Min Bae, Hyo-Sang Park, Oh-Wn Kwon, James A. McNamara, Jr., Microimplants in Orthodontics. 2006, Daegu, Korea: Dentos.
26. Sevetz, E., Treatment of the Severely Atrophic Fully Edentulous Maxillsz; The Zygoma Implant Option. Atlas Oral Maxillofac Surg Clin North Am, 2006. 14: p. 121-136.
27. Meskin, L. and J. Brown, Prevalence and patterns of tooth loss in U.S. adult and senior populations.Int J Oral Implantol, 1988. 5(1): p. 59-60.
28. Scurria, M.S., J.D. Bader, and D.A. Shugars, Meta-analysis of fixed partial denture survival: prostheses and abutments. J Prosthet Dent, 1998. 79(4): p. 459-64.
29. Priest, G.F., Failure rates of restorations for single-tooth replacement. Int J Prosthodont, 1996. 9(1): p. 38-45.
30. Aquilino, S.A., et al., Ten-year survival rates of teeth adjacent to treated and untreated posterior bounded edentulous spaces. J Prosthet Dent, 2001. 85(5): p. 455-60.
31. Tarnow, D.P., S. Emtiaz, and A. Classi, Immediate loading of threaded implants at stage 1 surgery in edentulous arches: ten consecutive case reports with 1- to 5-year data. Int J Oral Maxillofac Implants, 1997. 12(3): p. 319-24.
32. Feine, J.S., et al., The McGill consensus statement on overdentures. Mandibular two-implant overdentures as first choice standard of care for edentulous patients. Montreal, Quebec, May 24-25, 2002. Int J Oral Maxillofac Implants, 2002. 17(4): p. 601-2.
33. Piattelli, A., et al., A histologic evaluation of eight cases of failed dental implants: is bone overheating the most probable cause?Biomaterials, 1998. 19(7-9): p. 683-90.
34. Assif, D., et al., Comparative accuracy of implant impression procedures. Int J Periodontics Restorative Dent, 1992. 12(2): p. 112-21.
35. Veksler, A.E., G.A. Kayrouz, and M.G. Newman, Reduction of salivary bacteria by pre-procedural rinses with chlorhexidine 0.12%. J Periodontol, 1991. 62(11): p. 649-51.
36. Jepsen, S., et al., Primary prevention of peri-implantitis: managing peri-implant mucositis. J Clin Periodontol, 2015. 42 Suppl 16: p. S152-7.
37. Magnuson, B., et al., Comparison of the effect of two interdental cleaning devices around implants on the reduction of bleeding: a 30-day randomized clinical trial. Compend Contin Educ Dent, 2013. 34 Spec No 8: p. 2-7.
38. Levin, R.P., Waterpik dental water jet: creating value for your patients. Compend Contin Educ Dent, 2009. 30 Spec No 1: p. 20-1.
39. Etminan, M. and K. Aminzadeh, Bisphosphonates and ONJ. J Am Dent Assoc, 2008. 139(5): p. 535-6; author reply 536.