You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The recent emergence of bioactive dental materials has been a highly promising development for endodontic and restorative dentistry. One clinical challenge faced in restorative dentistry today is the ability to facilitate the remineralization of hypomineralized (affected) dentin to protect and preserve the vitality of the dental pulp. With current advances in bioactive materials, vital pulp therapy techniques such as pulp capping and partial and complete pulpotomy are re-emerging as a means of addressing this challenge.
TRADITIONAL CAVITY LINERS
Traditional cavity liners include calcium hydroxide and resin-modified glass ionomer cements. Calcium hydroxide has traditionally been the pulp capping material of choice for pulpal exposures.1 With direct pulp capping, the exposed vital pulp is treated with a therapeutic material before the placement of a base and restoration, which promotes healing, maintains pulp vitality, and protects the pulp from bacteria and noxious agents.2 However, a major limitation of calcium hydroxide is its high solubility, which may lead to the dissolution of the pulp capping material.2 This in turn results in the formation of defects in the reparative dentin underneath the capping material and a failure to provide a permanentseal against bacterial invasion.3Calcium hydroxide is also contraindicated under composite resins, owing to its interference with the set of the material. In addition, many of the light-cured glass ionomer liners are resin reinforced, which can limit any benefit from the release of fluoride, depending on the resin content.4
BIOACTIVE CAVITY BASES AND LINERS
Broadly speaking, the bioactivity of a restorative material (ie, its ability to elicit a biological effect) refers to the potential of the material to induce specific and intentional remineralization of dentin substrate.5 In terms of restorative dentistry, bioactive dental materials are described as "[those] that form a surface layer of an apatite-like material in the presence of an inorganic phosphate solution."6Thus, the remineralization of demineralized dentin is the process of restoring minerals through the formation of inorganic "mineral-like" substances, which in turn restores the structural health of the affected tissues.7
Bioactive liners have been a great advancement in the treatment of dental caries. By helping restore the missing calcium and phosphate ions that are lost as a result of acid attack, bioactive liners have been shown to have clinical advantage over more traditional cavity-lining materials. Bioactive liners can help remineralize affected dentin (dentin that is demineralized but bacteria-free) and convert it back into healthy dentin,8 while the use of round, polymer burs (Smart BurII, SS White) that are fabricated at the specific Knoop hardness of healthy dentin (90) can be used to ensure that only infected dentin (dentin that is demineralized but full of bacteria) is removed during the excavation process. Affected dentin may be "sticky" to the tactile touch, but it should not be removed. Placement of a bioactive liner can then help rebuild the remaining affected dentin.
Calcium silicate-based materials are bioactive materials capable of forming apatite by using calcium silicates or calcium aluminates. These materials are also considered to be biointeractive,9 because they release ions needed to stimulate dentin bridging. Mineral trioxide aggregate (MTA) is a calcium silicate-based material that is used in direct and indirect pulp capping in both primary and permanent teeth. MTA has been reported to be superior to calcium hydroxide for pulp capping of exposed pulps.10-12 However, MTA has several disadvantages, including handling difficulties, long setting time, tooth discoloration, and incompatibility with other dental materials.13
Among the new calcium silicate materials that have recently been introduced, Biodentine (Septodont), a calcium silicate-based bioactive dentin substitute used as pulp capping material, was developed to avoid the disadvantages of MTA. Biodentine is composed of tricalcium silicate cement, zirconium oxide, and calcium carbonate.14 This material is placed directly into the prepared cavity and induces dentin bridge formation. TheraBase (Bisco Dental Products) is a dual-cure calcium- and fluoride-releasing self-adhesive base/liner material that can be placed alone (if there is no pulp exposure) or with a layer of TheraCal™ LC (Bisco Dental Products) (if there is a pulp exposure). The hydrophilic resin matrix facilitates calcium release, which makes it a good dentin replacement that can then be layered with composite to complete the restoration.
TheraCal LC is a single paste calcium silicate-based material for use as a pulp capping agent. It is also used as a protective liner with restorative materials, cement, or other base materials. Unlike calcium hydroxide, TheraCal LC promotes the formation of a "moisture-proof seal" as one of its protective functions for long- term clinical success.
Deep caries removal often results in pulp exposure and the need for subsequent root canal treatment. Currently this trend is undergoing a reversal by the promotion of biologically based treatment strategies for partial caries removal that have been undertaken to avoid carious pulp exposures.15 In fact, current thought is that complete caries removal may be considered overtreatment.16 Strategies for the treatment of caries-induced pulp exposures is shifting toward avoidance of pulpectomy, while vital pulp treatment (VPT) techniques such as pulp capping and partial and complete pulpotomy are reemerging as preferred therapies.17 Under these circumstances, the retention of the natural teeth is the clinical goal. Many of these changes in treatment strategies are occurring because of the increased development of bioactive dental materials.15,18
CASE REPORT 1
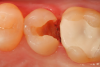
A 66 year-old female patientpresented with a "stained" occlusal groove in tooth No. 13 that did not "stick" with an explorer tip (Figure 1). Upon radiographic examination (Figure 2), a rather large carious lesion was discovered that encroached upon the dental pulp. There were no other clinical or subjective signs to alert the clinician or patient to the extent of the damage that had already occurred in the tooth. Figure 3 through Figure 5 show selective caries removal using a round end plastic polymer bur (SmartBurII, SS White). Before caries removal, isolation of the operative quadrant was achieved using Isovac (Zyris). Because of its Knoop hardness of 90, SmartBurII allows for removal of infected dentin only, while allowing affected dentin to remain for potential remineralization with a bioactive liner or base material.
Once selective caries removal was complete, without a direct exposure of the dental pulp, a sectional matrix, wedge, and ring were placed to begin the restorative process (Garrison 3D Sectional Matrix, Garrison Dental Solutions) (Figure 6). A bioactive pulp protectant/liner (TheraCal LC, Bisco Dental Products) was placed on moist dentin to a thickness of about .5 mm, then light cured (Figure 7). The remainder of the preparation was filled using a bulk fill packable composite material, sculpted to proper anatomic form, and light cured (Figure 8). Figure 9 shows the final radiograph after restoration of tooth No. 13 was completed. The tooth is planned to be checked clinically and radiographed every 2 to 3 months for the first year postoperatively to make certain that the tooth is responding favorably to the vital pulp therapy.
CASE REPORT 2
A 32 year-old female patientpresented with old composite restorations in tooth Nos. 18 and 19 that exhibited marginal leakage with potential for recurrent decay (Figure 10). After excavation, both teeth had deep decay beyond the extent of the restorative material, with tooth No. 19 having a "pinpoint" carious exposure of the pulp chamber (Figure 11). Figure 12 is a diagrammatic representation of the therapeutics that were used after removal of infected dentin and control of the bleeding from the pulp exposure. A pulp protectant/liner that is indicated for use on a direct pulp exposure (TheraCal LC, Bisco Dental Products) was placed directly on the exposed area and light cured. Both preparations were then filled with a bioactive dentin replacement (TheraBase, Bisco Dental Products) to a point just apical to the dentoenamel junction (Figure 13). Selective etch protocol was then used, etching the enamel (Select Etch HV, Bisco Dental Products) for 15 seconds (Figure 14), then rinsing with water and drying. Next, a universal bonding agent (All-Bond Universal, Bisco Dental Products) was placed, air thinned, and light cured (Figure 15). Figure 16 is an occlusal view of the completed restorations. Both teeth are planned to be followed and radiographed periodically to ensure that the pulps are responding favorably.
CONCLUSION
The use of bioactive liners and bases are changing the techniques and predictability of vital pulp therapy in dentistry. The more conservative we can be both in terms of the restoration materials and techniques that are selected and in maintaining the vitality of the dental pulp, the more likely our success in helping patients maintain their natural teeth and healthy dentition for their lifetime.
REFERENCES
1. Stangvaltaite L, Schwendicke F, Holmgren C, et al. Management of pulps exposed during carious tissue removal in adults: a multi-national questionnaire-based survey. Clin Oral Investig.2016;21(7):2303-2309.
2. Hilton T. J. Keys to clinical success with pulp capping: a review of the literature. Oper Dent.2009;34(5):615-625.
3. Stencel R, Kasperski J, Pakiela W, et al. Properties of experimental dental composites containing antibacterial silver-releasing filler. Materials (Basel).2018;11 (6):1031.
4. Kan KC, Messer LB, Messer HH. Variability in cytotoxicity and fluoride release in resin-modified glass ionomer cements. J Dent Res. 1997;76(8):1502-1507.
5. Nair P. N. R., Duncan H. F., Pitt Ford T. R., Luder H. U. Histological, ultrastructural and quantitative investigations on the response of healthy human pulps to experimental capping with mineral trioxide aggregate: a randomized controlled trial. Int Endod J.2008;41(2):128-150.
6. Faraco IM, Holland R. Response of the pulp of dogs to capping with mineral trioxide aggregate or a calcium hydroxide cement. Dent Traumatol.2001;17(4):163-166.
7. Aeinehchi M., Eslami B, Ghanbariha M, Saffar AS. Mineral trioxide aggregate (MTA) and calcium hydroxide as pulp-capping agents in human teeth: a preliminary report. Int Endod J.2002;36(3):225-231.
8. Sauro S, Pashley DH. Strategies to stabilise dentine-bonded interfaces through remineralising operative approaches - State of The Art. Int J Adhesion Adhesives 2016;69:29-57.
9. Barszczewska-Rybarek I, Chladek G. Studies on the curing efficiency and mechanical properties of bis- GMA and TEGDMA nanocomposites containing silver nanoparticles. Int J Mol Sci.2018;19(12):3937.
10. Hench LL. Bioceramics. J Am Ceram Soc.2005;81(7):1705-1728.
11. Jefferies SR. Bioactive and biomimetic restorative materials: a comprehensive review: Part I. J Esthet Restor Dent.2014;26(1):14-26.
12. Cao CY, Mei ML, Li QL, Lo ECM, Chu CH. Methods for biomimetic remineralization of human dentine: a systematic review. Int J Mol Sci.2015;16(3):4615-4627.
13. Pameijer CH, Garcia-Godoy F, Morrow BR, Jefferies SR. Flexural strength and flexural fatigue properties of resin-modified glass ionomers. J Clin Dent.2015;26(1):23-27.
14. About I. Biodentine: from biochemical and bioactive properties to clinical applications. Giornale Italiano di Endodonzia.2016;30(2):81-88.
15. Schwendicke F, Frencken JE, Bjørndal L, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Adv Dent Res2016;28(2):58-67.
16. Bjørndal L, Simon S, Tomson PL, Duncan HF. Management of deep caries and the exposed pulp. Int Endod J.2019;52(7):949-973.
17. Tyas M. J. Pulp protection under restorations-do you need a liner? Aust Endod J.1998;24(3):104-108.
18. Camilleri J. Hydration characteristics of biodentine and theracal used as pulp capping materials. Dent Mater.2014;30(7):709-715.