You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
One of the most noteworthy influences on the oral healthcare profession was the emergence of the human immunodeficiency virus (HIV) in 1981.1This epidemic transformed the clinical oral health care setting, leading to better understanding of disease transmission and prevention and a greater application of infection prevention and control measures in the dental setting.1 Prior to the COVID-19 pandemic, dental healthcare professionals (DHCP) ensured infection control in dentistry by following the guidance of the Centers for Disease Control and Prevention (CDC). The CDC document, Guidelines for Infection Control in Dental Health Care Settings, 2003,2 provided key recommendations to prevent and control infectious disease transmission in dental settings. In 2016, the CDC published a summary guide based on the 2003 guidelines. This guide highlights the existing CDC recommendations on the basic infection prevention principles, reaffirms standard precautions as the foundation for preventing the transmission of infectious agents during patient care, and provides links to the full guidelines and source documents for more detailed background on the recommendations. Another feature of the 2016 summary document was more detailed descriptions and checklists regarding administrative measures for instrument processing and disinfection, infection prevention education and training, respiratory hygiene and cough etiquette, dental unit waterline quality, and safe injection practices.3 While these resources have been free and readily available for all DHCP in the United States (US), research shows not all DHCP were in compliance with the CDC guidelines.4
Although reports of transmissions of bloodborne pathogens (BBPs) in dental settings are uncommon, there is evidence that breaches in infection control protocols by DHPs are the leading cause of these transmissions.5-7 Breaches include a case of patient-to-patient transmission of Hepatitis B Virus (HBV) in a dental practice setting, the acute HBV infection of five individuals in a free dental clinic, and the first recorded case of patient-to-patient transmission of Hepatitis C Virus (HCV) within an oral surgery practice.5 Research continues to show inconsistencies in infection control compliance in all aspects of the dental setting.1,4,8 Both the CDC as well as the Occupational Safety and Health Administration (OSHA) guidelines are frequently breached within dental laboratories, making these settings one of the most vulnerable infection control areas within dentistry.8 In studies conducted in the US, there continues to be a low level of compliance in regard to having an exposure control plan (ECP),9 maintaining and monitoring dental unit water quality, medical safety device use, recording percutaneous injuries, and having a designated infection control coordinator.4 Underreporting of violations, failure to link dental setting transmissions due to the long incubation period of HBV, HCV and the asymptomatic progression of Human Immunodeficiency Virus (HIV), are common limitations found in research focused on disease transmission in dentistry.5-6
Knowledge, attitudes, and perceptions of infection control protocols have a direct connection to infection control compliance, and breaches within the dental profession10-13 Though research has shown compliance in infection control protocols to be generally lower in developing countries due to financial constraints, basic knowledge in this area should not be deficient regardless of location and economic status.11 Furthermore, the recent discovery of the novel COVID-19 virus should encourage all members of the dental team to be well versed in such guidelines, and the attitudes of DHCPs in following CDC infection control guidelines should be closely observed. The purpose of this study was to examine DHCPs knowledge, attitudes, practices and barriers regarding the CDC infection control guidelines in dentistry (2003, 2016). The study was completed prior to identification of COVID-19 in the US.
Methods
The MCPHS University's Institutional Review Board granted this study an exempt status under 45 CFR 46.104d(2) (i) and assigned protocol number IRB120419B.The study design was a descriptive, cross-sectional survey, with a convenience sample of DHCPs (dental assistants, dental hygienists, and dentists; n= 397) within the United States. In order to participate the DHCP needed to be at least 18 years of age, must be assisting with or providing patient care in a clinical setting in the US at least one day/week, and be fluent in reading and speaking English. Dental assistants did not have to be DANB certified, licensed, or graduated from a CODA accredited program. Those not meeting one or more of the criteria were excluded from participation. A power analysis (G*Power) for the most conservative planned statistical test (one-way ANOVA, two-tailed, four groups) using a medium effect size (f=0.25), α=.05, and 80% power suggested a minimum sample size of n=180. Adjusting for expected attrition of 30% the final recommended sample size was n=257.
Survey Instrument
This survey was designed based on the literature consisted of the following sections: demographics (4 items), familiarity with the 2003 CDC infection control guidelines and the 2016 Summary (9 items), infection control knowledge (10 items), participants' current practices in infection control (8 items), barriers with one open-ended question to report additional barriers (8 items), attitudes in seeking information on infection control (3 items) for a total of 42 items. The ten familiarity (perceived knowledge) questions were paired with the ten related knowledge questions. The pairing of these sections helped to identify the knowledge of each participant more accurately and to subsequently compare these responses to how familiar the individual reported being with each subject. A Likert scale of 1 (not familiar) to 5 (very familiar) was used to measure respondent's familiarity while the Likert scale of 1 (extremely unlikely) to 7 (extremely likely) was used to determine the likelihood of DHCP to further their infection control knowledge within the next 12 months.15
The survey instrument was validated using the content validity index (CVI) to evaluate the relevance of each survey questions to the study variables16 and was conducted with five content raters who had background and expertise in infection control. The validation process resulted in a S-CVI= 0.97 and revisions were made based on feedback. The survey was pilot tested with dental professionals (n= 10) who met inclusion criteria to assess comprehension and readability. Feedback given by the content raters resulted in slight edits to the survey content as well as to the implementation of an additional question.
The survey was administered to a convenience sample recruited through professional dental social media groups including, Facebook, LinkedIn, and Instagram, as well as face-to-face recruitment at a large dental conference in New England. Snowball sampling to obtain a larger sample size of practicing dentists was also used.17
Data Analysis
For the descriptive portion of this study, the sample demographic information and response to survey questions was summarized and reported with measures of variance (e.g. standard deviation). Next, all variables were analyzed for statistical assumptions including normalcy and co-linearity. Variables were assessed for transformation to address issues of non-normal distributions. Outliers were identified and removed, however if the findings are consistent when including outliers, those cases were used in the main analysis. The data was analyzed for missing data and any participant with less than 80% completion was removed from parts or the whole analysis.
Two or more predictors were used to explore the relationship between variables, for continuous variables correlation (Pearson or Spearmen), for categorical variables chi-square tests of independence, and multiple regression (linear, logistic, ordinal, multinomial) for modeling. To test for differences in means between categorical variables t-tests or ANOVA was used, and in the cases where the distribution did not meet assumptions for the Normal model, the non-parametric equivalent (Wilcoxon U, Kruskal-Wallis) was utilized. Whenever appropriate adjustments to family wise error (e.g. Bonferroni) were made for multiple statistical tests. The acceptable alpha level for was set at .05 for hypothesis testing and all measures of effect size (e.g. 95% Confidence Interval, R2, Phi Coefficient) were determined and reported.
Results
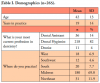
A total of 397 DHCPs opened the survey link; the completion rate was 67%. The mean age of the participants was 42.3 years and had 19.4 years in practice. Most participants were dental hygienists; two-thirds of the respondents were from the Midwest. Sample demographics are shown in Table I.
Participants were asked a series of familiarity (perceived knowledge) questions regarding CDC Infection Control Guidelines (2003, 2016) as shown in Table II. Three-quarters of the respondents reported infection control training was mandatory in their state for license renewal while 10% did not know. All state of practice responses were recoded into the five US regions (West, Southwest, Midwest, South, and Northeast) (Table I). A chi-square test of independence was used to evaluate the relationship between region of practice and infection control licensure requirement. The Midwest had the highest number of participants indicating infection control continuing education was a requirement for licensure (n=155, 86%), while the Southwest had the lowest (n=6, 50%, χ2(8)=24.1, p=0.002, phi=0.30).
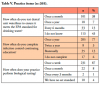
Participants stated they were very familiar to extremely familiar with CDC recommendations regarding dental unit waterline maintenance (63%); dental handpiece infection control practices (80%); the term and meaning of standard precautions (73%); hand hygiene (96%); OSHA bloodborne pathogen standard (85%); CDC recommendations regarding critical items (81%); biological testing (67%); and respiratory hygiene and cough etiquette (73%) (Table II).
Knowledge of CDC Guidelines
Two-thirds of respondents correctly answered 6-9 (out of 13) of the knowledge questions while just one-third of the participants correctly answered items related to the guidelines for treatment of dental unit water lines, the provision of tissues and no-touch disposal receptacles, and hand hygiene as the most important measure to prevent spread of infection (Table III). Only a small percentage of respondents (15%) correctly answered the knowledge regarding the dental health care setting's need to encourage persons with symptoms of respiratory infections to sit as far away from others as possible. An independent sample t-test test of independence was calculated to investigate the relationship between state licensure requirement and knowledge score, but was not statistically significant, p=0.75.
Infection Control Practices
Infection control practices are shown in Table IV and Table V. Providing a mask for people with a visible respiratory infection while in the reception area was the category reported with the least compliance (41%). Three-quarters (77%) of respondents completed an infection control continuing education course annually. Nearly half (43%) of the respondents did not know how often their dental unit waterlines were tested to ensure Environmental Protection Agency (EPA) standards of drinking water while a majority (87%) reported completing weekly biological testing on their sterilizers.
Infection Control Barriers
DHCPs ranked barriers to following infection control guidelines in practice from one to seven, with one being the most relevant barrier within their practice and seven being the least barrier within their practice. The greatest barrier found was a heavy workload (34%), followed by time restraints (25%), expense (15%), and lack of training (13%). The barrier DHCPs found to be the least relevant barrier was lack of good role models (2%) which was ranked as seventh. In the open-ended question, a common trend stated by DHCPs was lack of supplies. In particular, there were not enough handpieces available to comply with proper sterilization methods.
Infection Control Education
Most DHCPs (75%) were extremely likely to further their infection control knowledge by attending an infection control continuing education class within the next 12 months. Less than half of participants (44%) reported they were extremely likely to read the CDC guidelines regarding infection control in dentistry or take an online infection control course (44%) within the next 12 months.
Discussion
This study explored the level of knowledge, practices, attitudes and barriers faced by DHCPs regarding the CDC Guidelines for Infection Control in Dental Health Care Settings (2003) and the Summary of Infection Prevention Practices in Dental Settings: Basic expectations for safe care in dentistry (2016), prior to the COVID-19 pandemic. In the area of knowledge, the findings in this study were consistent with the systematic review by Khanghahi12 concerning the overall knowledge of infection control practices. Although the majority of participants stated they were moderately to extremely familiar with CDC guidelines pertaining to dental unit waterlines; hand hygiene; OSHA bloodborne pathogen standard; and respiratory and cough etiquette, these were the areas where participants in this study were found to be the least knowledgeable.
Infection control practices carried out in clinical settings prior to COVID-19 were examined and it was found that almost half of participants did not know if their dental unit waterlines were tested to ensure compliance with the established Environmental Protection Agency standards for drinking water. Furthermore, 70% could not correctly identify the standards raising concerns regarding whether the CDC regular training on infection control policies and guidelines is taking place.3 Lack of knowledge regarding the contamination levels of dental unit waterlines can ultimately be detrimental to immunocompromised patients in addition to posing a public health concern.3
While most participants reported performing weekly biological testing to monitor sterilizers, some respondents did not follow this CDC recommendation at all. Similarly, participants stated there were times when both high and low speed handpieces do not go through the proper sterilization process after each patient. Wiping dental handpieces with a disinfectant in between patients is a direct breach of infection control guidelines which could result in disease transmission as was the case for five individuals who became infected with HBV after visiting a portable dental clinic.18 Blood borne disease transmission is a possible consequence of not following CDC guidelines for sterilization and monitoring sterilizer efficacy2,3 due to the long incubation period of some of these pathogens.
Participants in this study reported washing their hands a total of 32 times in a typical 8-hour workday, yet the majority of respondents were unable to correctly identify that hand hygiene was classified by the CDC as the most important measure in preventing the spread of infections among patients and providers.3 This finding leads researchers to hypothesize that while the practice of hand hygiene may be high within DHCPs, the knowledge behind the rationale for the practice is lacking. Lack of knowledge can be associated with poor hand hygiene practices leading to bacterial transmission to patients. This was exemplified in the case of an oral surgery patient who died due to bacterial endocarditis complications traced to the lack of hand hygiene and aseptic technique compliance of a DHCP during the administration of medications.7
Results from this study identified the top three barriers to following the CDC infection control guidelines to be a heavy workload, time restraints, and expense, which were consistent with findings in previous studies.10 Dental health care providers should develop team-based strategies to alleviate these barriers with the goal of protecting their patients as well as themselves. In general, dentists in the US are the direct supervisors of both dental hygienists and dental assistants, and ultimately oversee supply costs and patient load within a dental practice. Targeting more intense infection control instruction strategies toward practice owner employers/supervisors may promote positive change and foster a culture that follows CDC guidance more closely.10
One of the most significant findings in this study was the lack of knowledge regarding respiratory hygiene and cough etiquette in dentistry.2,3 One-third of the respondents were not aware of the CDC guidelines for respiratory hygiene and cough etiquette guidelines for dental health care settings and patients with a visible respiratory infection were provided with a mask while in the reception area only 41% of the time. Varying answers to the respiratory hygiene, cough etiquette, and hand hygiene items revealed areas needing to be further addressed by the dental profession prior to the emergence of the novel respiratory disease, COVID-19.19 More emphasis needs to be placed on the significance and the mitigation of the transmission respiratory diseases in infection control courses for DHCPs.
Although the study attempted to analyze state and regional differences regarding continuing education licensure requirements for infection control, the only state with an adequate sample size was Massachusetts and the only region was the Midwest, which limited the analysis. This area needs further research with a larger sample for each state. Given the gaps in actual versus perceived knowledge regarding infection control guidelines, it may also be prudent to also assess the way continuing education is delivered. Currently the norm is passive lecture with no assessment mechanism. An emerging trend for a variety of professions is for the licensee to develop a comprehensive plan for continuing professional development (CPD) rather than simply listing the number of hours of continuing education.20,21 Continuing professional development plans require the licentiate to demonstrate application of learning, evaluation, and reflection to verify continuing competence within their discipline.20,21
Limitations of this study included convenience sampling, self-report bias, self-selection bias, and misrepresentation of DHCPs who do not participate in social media forums, or who do not have regular access to the Internet, and social desirability. The sample was largely made up of mostly registered dental hygienists and is not representative of the demographic balance of DHCPs. Some states do not require licensure of dental assistants so there could have been a wide range of educational experiences and background for this group; however, they were only a percentage of the sample. More research is needed regarding infection control practices in dental laboratories. In addition, infection control knowledge (perceived and actual), practices and education related to interim and updated CDC and OSHA guidelines post-COVID-19 warrant further investigation. Findings from this study may serve as a baseline for comparison.
Conclusion
Although DHCPs reported familiarity (perceived knowledge) with the CDC Guidelines for Infection Control in Dental Health Care Settings (2003) and the Summary of Infection Prevention Practices (2016), their actual knowledge and practices prior to the COVID-19 pandemic were not consistent with the perceived knowledge. The lack of basic knowledge regarding CDC infection control guidelines in dental health care settings is particularly concerning given the global emergence of the novel COVID-19 virus. Evidence-based infection control protocols will continue to evolve in dentistry and DHCPs must be responsible for incorporating the latest guidance into practice. Results of this study also provides evidence supporting the need for infection control continuing education as a requirement for licensure.
Cristina J. Posada, CDA, RDH, MS is an instructor, Greater Lawrence Technical School, Andover, MA, USA. Linda D. Boyd, RDH, RD, EdD is a professor and the Associate Dean for Graduate Studies; Kristeen R. Perry, RDH, MSDH is an associate professor, MSDH; Jared Vineyard, PhD is an adjunct faculty member; all at the Forsyth School of Dental Hygiene, MCPHS University, Boston, MA, USA.
References
1. Oosthuysen J, Potgieter E, Fossey A. Compliance with infection prevention and control in oral health-care facilities: a global perspective. Int Dent J. 2014 Dec;64(6):297-311.
2. Kohn WG, Collins AS, Cleveland JL, et al. Guidelines for infection control in dental health-care settings-2003. MMWR Recomm Rep 2003;52(RR-17):1-61.
3. Centers for Disease Control and Prevention. Summary of infection prevention practices in dental settings: basic expectations for safe care [Internet]. Atlanta, GA: US Dept of Health and Human Services; 2016 Oct [cited 2020 Aug11]. 44 p. Available from: https://www.cdc.gov/oralhealth/infectioncontrol/pdf/safe-care2.pdf
4. Cleveland JL, Bonito AJ, Corley TJ, et al. Advancing infection control in dental care settings: factors associated with dentists' implementation of guidelines from the Centers for Disease Control and Prevention. J Am Dent Assoc. 2012 Oct;143(10):1127-38.
5. Cleveland JL, Gray SK, Harte JA, et al. Transmission of blood-borne pathogens in US dental health care settings: 2016 update. J Am Dent Assoc. 2016 Sep;147(9):729-38.
6. Southworth PM. Infections and exposures: reported incidents associated with unsuccessful decontamination of reusable surgical instruments. J Hosp Infect. 2014 Nov;88(3):127-31.
7. Ross KM, Mehr JS, Greeley RD, et al. Outbreak of bacterial endocarditis associated with an oral surgery practice: New Jersey public health surveillance, 2013 to 2014. J Am Dent Assoc. 2018 Mar;149(3):191-201.
8. Vázquez-Rodríguez I, Estany-Gestal A, Seoane-Romero J, et al. Quality of cross-infection control in dental laboratories. A critical systematic review. Int J Qual Health Care. 2018 Aug 1;30(7):496-507
9. Laramie AK, Bednarsh H, Isman B, et al.. Use of bloodborne pathogens exposure control plans in private dental practices: results and clinical implications of a national survey. Compend Contin Educ Dent. 2016 Jun;38(6):398-407.
10. Garland KV. A survey of United States dental hygienists' knowledge, attitudes, and practices with infection control guidelines. J Dent Hyg. 2013 Jun;87(3):140-51.
11. Gordon BL, Burke FJ, Bagg J, et al. Systematic review of adherence to infection control guidelines in dentistry. J Dent. 2001 Nov;29(8):509-16.
12. Moradi Khanghahi B, Jamali Z, Pournaghi Azar F, et al. Knowledge, attitude, practice, and status of infection control among Iranian dentists and dental students: a systematic review. J Dent Res Dent Clin Dent Prospects. 2013;7(2):55-60.
13. Oosthuysen J, Potgieter E, Blignaut E. Compliance with infection control recommendations in South African dental practices: a review of studies published between 1990 and 2007. Int Dent J. 2010 Jun;60(3):181-9.
14. World Health Organization. Advocacy, communication and social mobilization for TB control: A guide to developing knowledge, attitude and practice surveys [Internet]. Switzerland: WHO Press; 2008 [cited 2020 Aug 11]. Available from: https://apps.who.int/iris/bitstream/handle/10665/43790/9789241596176_eng.pdf;jsessionid=760057802DE3119F21C7958ED8DADFF3?sequence=1
15. Awang Z, Afthanorhan A, Mamat M. The Likert scale analysis using parametric based structural equation modeling (SEM). Computational Methods Soc Sci. 2016 Jun1;4:13-21.
16. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007 Aug;30(4):459-67.
17. Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations studying hidden populations. Social Problems [Internet]. 1997 May [cited 2020 Aug 11];44(2):174-99. Available from: https://heinonline.org/HOL/P?h=hein.journals/socprob44&i=184
18. Radcliffe RA, Bixler D, Moorman A, et al. Hepatitis B virus transmissions associated with a portable dental clinic, West Virginia, 2009. J Am Dent Assoc. 2013;144(10):1110-8.
19. Ling L, Joynt GM, Lipman J, et al. COVID-19: A critical care perspective informed by lessons learnt from other viral epidemics. Anaesth Crit Care Pain Med. 2020 Feb 20:S2352-5568(20)30029-1
20. Tran D, Tofade T, Thakkar N, Rouse M. US and international health professions' requirements for continuing professional development. Am J Pharm Educ. 2014 Aug 15;78(6):129.
21. Micallef R, Kayyali R. A systematic review of models used and preferences for continuing education and continuing professional development of pharmacists. Pharmacy. 2019 Nov 16; 7(4):154.