You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Despite the high risk of dental hygiene professionals developing work-related musculoskeletal disorders (WMSDs),1-5 incongruities exist between the clinicians' perceived and actual postures while providing patient care. Most surveyed dental professionals reported experiencing musculoskeletal pain despite being aware of neutral ergonomic positions.2 Areas frequently associated with reported pain among dental hygienists include the neck, back, shoulders, and hands/wrists.1,6-9 The typical work schedule for the typical dental hygienist in clinical practice, which includes the delivery of dental hygiene care for 45-60 minutes for up to 8 patients a day, 7-8 hours a day, 3-4 days a week, has been associated with reported moderate to severe pain.8 Musculoskeletal pain has been reported to begin within the first six to ten years of clinical practice, although some clinicians may experience pain sooner.10, 11 As WMSDs progress, many dental hygienists seek therapy for pain, take time-off, and may become unable to practice clinically.
The postures of dental hygienists are dependent upon the clock-positioning of the patient in relation to the operator, which is defined in the textbooks used in entry-level dental hygiene programs.12,13 With the patient's head at 12:00 o'clock, right-handed operators provide treatment from the 8:00 o'clock to 1:00 o'clock position whereas left-handed operators provide treatment from the 4:00 o'clock to 11:00 o'clock position.12,13 Although most dental hygienists prefer and utilize a seated position from the rear or 11:00-1:00 o'clock positions when delivering dental hygiene care, these positions may actually be contributing to the development of musculoskeletal disorders.14-16
The availability of personal equipment, such as stools and magnification loupes, can impact the postures of dental operators. Stool choice may also influence the development of musculoskeletal pain since dental hygienists provide care in seated and static positions. The use of saddle seats have been shown to promote neutral positions with the anterior tilt of the lower lumbar spine, which allows for the relaxation of this region of the spine.17Although dental hygienists may consider utilizing saddle seats in clinical practice settings, they are not routinely provided in most dental offices due to the additional cost of the specialized seat and the prevalence of their use by dental hygienists is unknown. The use of magnification loupes has been increasing among dental hygienists for many reasons. The current trend in dental hygiene programs is to require the purchase and use of magnification loupes by dental hygiene students early in their education.18 However, there is a disparity in which more dental hygiene students own magnification loupes than the dental hygiene faculty members.18,19 As more dental hygiene students are required to purchase and use magnification loupes, future dental hygiene educators will have regularly utilized and experienced the associated benefits of these devices. Dental hygienists have reported experiencing reduced musculoskeletal pain and perceived improved accuracy with the use of magnification loupes.20
The transition from an academic clinical environment with long appointment times to private practice settings with shorter appointment times may also affect the development of musculoskeletal pain. From informal faculty observations in student clinic settings, dental hygiene students tend to accommodate their patients at the expense of their personal postures. During the development of indirect vision skills, dental hygiene students may often overcome feelings of frustration by compromising their postures to use direct vision. Habits formed in the student clinical environment may later translate into professional practice and the progression of musculoskeletal pain.
Although clinicians may be aware of general principles of ergonomics, a disconnection exists in the application of ergonomic recommendations.21 Because dental hygienists typically work independently in a clinical setting, the individual clinician has the responsibility of self-identifying and self-correcting postural problems. Self-assessment involves the accurate judgment of an individual's performance using detailed criteria and corresponding with a validated measure of one's performance.22 Accurate self-assessments are especially necessary for independently practicing clinicians. When postures extend beyond acceptable criteria, dental hygienists may unknowingly incur detrimental effects that may lead to WMSDs. Without intervention, the lack of awareness of postural problems may lead to the progression of musculoskeletal pain.
Feedback using self-assessment and photography has been previously shown to improve ergonomic scores and the accuracy of ergonomic self-assessment among dental and dental hygiene students over a four-week period.23,24 However, it remains unknown whether this intervention would be effective with practicing clinicians. The purpose of this study was to determine the regions at greatest risk for developing musculoskeletal strain and to evaluate the effect of an interventional training involving photography and self-assessment on posture and the accuracy of ergonomic self-assessments among dental hygiene students (DHS) and registered dental hygienists (RDH).
Methods
This randomized control study was approved by The Ohio State University Biomedical Institutional Review Board, (2017H0343, 2018H0157). A convenience sample of 29 junior-year dental hygiene students (DHS) enrolled during autumn 2017 in The Ohio State University baccalaureate dental hygiene program and 20 registered dental hygienists (RDH) employed during the summer 2018 at The Ohio State University College of Dentistry were recruited to participate. The DHS and RDH participants were assigned into one of two groups (control and training) using random sampling program in SPSS Version 25 (IBM, Chicago, IL, USA). Two faculty raters and two key personnel were recruited from The Ohio State University, Division of Dental Hygiene to participate as evaluators in this study. After explaining the rationale and the research study design, all participants signed written informed consent forms prior to starting the study.
Sample
Dental hygiene student participants were enrolled in a preclinical dental hygiene course and received one hour of didactic instruction on ergonomics at the beginning of the term. During the four-week study, all DHS participants practiced implementing all the pre-clinical exercises which included posterior area specific curettes, ultrasonic scalers, universal scalers, and intra- and extra-oral examinations in all areas of the mouth. The RDH participants were employed on a part-time or full-time basis as professors, clinical instructors, or dental hygiene practitioners. During the four-week study, all RDH participants performed their usual patient care procedures. The use of magnification loupes, with or without coaxial illumination, and saddle seats was not required for participation in the study.
Instrument
A modified-dental operator posture assessment instrument (M-DOPAI) with 12 components was utilized for the self-assessments and rater evaluations (Table I). This instrument was modeled after the Branson et al. Posture Assessment Instrument (PAI) consisting of 10 components, which was tested for validity and reliability for imaged and real-time postures,25 and the Maillet et al. Posture Assessment Criteria (PAC), which added two components involving the upper arms.26 The criteria for the components were detailed within the M-DOPAI. Each component score had one of three categories: acceptable (1 point), compromised (2 points), or harmful (3 points). Eight of the 12 components included a harmful category. The total scores ranged from 12 to 32 with the lower scores being more acceptable. Thus, the most ideal postures scored 12 points whereas the most harmful postures scored 32 points. Figure 1 provides images of front and profile views representing a typical seated posture.
Procedure
The study occurred over the course of four weeks; the flow is illustrated in Figure 2. During week one, all participants were photographed twice in their respective clinical settings, without sound or flash (front and profile views) and all participants independently completed a pre-test ergonomic self-evaluation using the M-DOPAI without viewing the photographs or receiving any feedback. In order to generate valid self-assessments, each participant was provided with general instructions to read through each of the 12 components of the M-DOPAI and was asked to self-assess their postures using the criteria (score of 1 representing the best and a score of 3 representing the worst).
During weeks two and three, participants in the control group independently completed weekly ergonomic self-assessments without viewing photographs or receiving feedback from the principal investigator. Participants in the training group had two additional photographs without sound and flash taken weekly (front and profile views) and completed a weekly ergonomic self-assessment with the principal investigator using the photographs during each of the two weeks. The principal investigator facilitated the self-assessments by guiding the participant through each of the twelve components. The principal investigator would either agree with the participant's self-assessment or guided the participant to re-evaluate their assessment.
All images were captured, without sound or flash, and displayed for the participants' self-assessments using tablet technology (Galaxy Note 10.1, Samsung, Ridgefield Park, NJ, USA). At week four, all participants were photographed the final two times (front and profile views), without sound or flash, and independently completed a post-test ergonomic self-assessment without viewing the photographs or receiving any feedback from the principal investigator. Participants were provided with the same general instructions, as provided during the pre-test.
The participants' pre-test (week one) and post-test (week four) photographs were each evaluated for an ergonomic score using the consensus of two faculty and two key personnel raters. The agreement of three of the four raters provided consensus of the scores and defined the gold standard for the data analysis. The four raters received group didactic instruction from the principal investigator on ideal neutral ergonomic positioning12,13 and the recognition of any deviations from neutral positioning. The raters were also provided with a detailed orientation to each of the 12 components of the M-DOPAI and a practice application of the M-DOPAI to an imaged posture. Raters independently evaluated the photographs and the scores were compared to generate consensus scores achieved with the agreement among three of the four raters.
Data analysis
Data were analyzed using SPSS Version 25 (IBM, Chicago, IL, USA). Descriptive statistics and one-way ANOVA were used to evaluate the variances between the sample groups. The accuracy of self-assessments was calculated with the comparison of self-assessment scores and rater scores, serving as the gold standard, at the following timepoints: pre-training (week one) and post-training (week four). Inter-rater reliability levels were calculated using Cohen's Kappa coefficient because it analyzed data in nominal scale and accounted for agreement due to chance.27-29 Kappa scores ranged from less than 0 (no agreement) to 1 (perfect agreement). Slight agreement values ranged from 0.00-0.20, fair agreement values ranged from 0.21-0.40, moderate agreement values ranged from 0.41-0.60, full agreement valued ranged from 0.61-0.80, and perfect agreement values were greater than 0.81.27-29 Variances between the sample groups were evaluated using mixed-design ANOVA. Significance levels were set at p-values <0.05.
Results
A total of 49 participants completed the study: 29 dental hygiene student (DHS) participants (14 in the control group and 15 in the training group) and 20 registered dental hygienist (RDH) participants (10 in the control group and 10 in the training group). All DHS participants were female and there were no significant differences in the two groups regarding mean years of age (M=21.4, sd=3.6). Nineteen of the RDH participants were female and there were no significant differences in the two groups regarding mean age (M=45.22, sd=11.69), hours worked per week (M=25.03, sd=14.85), or number of years in clinical practice (M=20.66, sd=12.65).
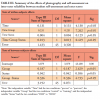
The first aim was to determine the regions, identified by the raters, most at-risk for musculoskeletal strain among DHS and RDH. The top three regions identified as most at-risk by the raters were the head-front to back (DHS- M=1.84, sd=.696, RDH- M=1.85, sd=.533), upper arms-elbows (DHS- M=1.71, sd=.562, RDH- M=1.70, sd=.468), and upper arm- parallel (DHS- M=1.64, sd=.742, RDH- M=1.55, sd=.677). One-way ANOVA was used to determine significant differences in the mean scores for the body regions between DHS and RDH groups. The scores for the RDHs were significantly higher in the areas of trunk (rotation) (F(1,96)=4.746, p<.05), head (rotation) (F(1,96)=4.194, p<.05), and shoulders (leveled) (F(1,96)=4.617, p<.05) than the DHS group. The scores for the DHS were significantly higher in the area of wrists (flexed/extended) (F(1,96)=3.884, p<.01) than the RDHs. Rater comparisons of areas most at risk for musculoskeletal strain for DHS and RDHs is shown in Table I.
The second aim was to determine the regions, identified through the self-assessments, most at-risk for musculoskeletal strain among DHS and RDHs. The top three self-assessed regions that were identified as most at-risk were the head-side to side (M=1.80, ssd=.456), head-front to back (M=1.57, sd=.540), and trunk-side to side (M=1.57, sd=.540). The top three rater-evaluated regions identified as most at-risk were head-front to back (M=2.12, sd=.600), upper arms-elbows (M=1.86, sd=.612), and upper arms- parallel (M=1.69, sd=.822). One-way ANOVA was used to determine significant differences in the mean scores for the body regions between self-assessment and rater evaluations. Self-assessments scores were significantly higher in the regions of trunk (front to back) (F(1,96)=18.062, p<.001), trunk (side to side) (F(1,96)=18.935, p<.001), trunk (rotation) (F(1,96)=6.114, p<.01), head (side to side) (F(1,96)=27.881, p<.001), head (rotation) (F(1,96)=20.915, p<.001), shoulders (leveled) (F(1,96)=7.291, p<.01), and wrists (F(1,96)=5.476, p<.05) than the rater-evaluation scores. However, the rater-evaluation scores were significantly higher in the regions of head (front to back) (F(1,96)=22.841, p<.001) and upper arms (elbows) (F(1,96)=6.861, p<.01). The comparisons of areas at risk for musculoskeletal strain between participants' self-assessments and rater evaluations is shown in Table II.
The third aim was to determine the effect of feedback involving photography and self-assessment on the accuracy of ergonomic self-assessments among DHS and RDH shown in Table III. A 2x2x2 mixed-design ANOVA was calculated to examine the effects of the group (control group and training group), status (DHS and RDH) and time (pre-test and post-test) on reliability (Cohen's Kappa coefficient between self-assessment and rater-evaluations). Significant interactions were found with time (pre-test and post-test) x group (control group and training group) (F(1,45)=7.262, p<0.01). A main effect for group (control group and training group) was found to be significant (F(1,45)=4.733, p<0.05). Post hoc analysis using one-way ANOVA revealed a significant increase in agreement with the training group at the posttest (F(1,48)=4.866, p<0.05). The training caused a significant increase in agreement in the training groups comprised of DHS and RDH participants compared to the control groups comprised of DHS and RDH participants.
Discussion
The purpose of this study was to determine the most at-risk regions for developing musculoskeletal strain and to evaluate the effect of training involving photography and self-assessment on the postures and the accuracy of ergonomic self-assessments among DHS and RDHs. The top at-risk regions for musculoskeletal strain, as identified by the raters, were the head and upper arms. The top regions at-risk for musculoskeletal strain, as identified through self-assessments, were the head and trunk. The training with feedback using photography improved ergonomic scores and the accuracy of the ergonomic self-assessments in the experimental group.
Over time, static postures in compromised positions may lead to musculoskeletal disorders.30 Based upon the rater evaluations, the most compromised regions identified by both students and practicing clinicians were the forward flexion of the head and the forward placement and abduction of the upper arms. However, RDHs were more likely to further compromise their postures with the rotation of the head/neck, rotation of the trunk, and unleveled shoulders than the DHS. Static and compromised repeated positioning of these regions has been identified as a contributor to the development of musculoskeletal disorders.9,31
The physical demands of providing dental hygiene care may cause dental hygiene students and practicing clinicians to compromise their personal postures for better visualization or to prevent the disruption of patient comfort.10 The participants in this study may have been aware of this reality based on the comparisons between self-assessments and rater evaluations. Both the DHS and RDHs self-rated their trunk, head, and shoulder positions as more severely compromised than the rater evaluations. This is contrary to the tendency of students to positively overestimate self-assessment scores, which may impact learning or the improvement of skills.32 In general, both dental hygiene students and registered dental hygienists have a more negative perception of their postures than the reality of their actual positioning.
A paradox exists in which dental hygiene clinicians possess an awareness of their possible compromised postures but lack either the motivation to improve postures or an understanding of how to maintain visualization. The use of magnification loupes or having ergonomics education may account for a decreased likelihood of reporting musculoskeletal problems.7 The major impetus for improving postures is usually pain.33 However, chronically compromised postures increase the risk of and contribute to the initiation of musculoskeletal disorders. Evidence has shown that musculoskeletal disorders for dental hygienists may begin as early as during their entry-level clinical programs.4,34 After entry into clinical practice, dental professionals remain at higher risk for developing work-related musculoskeletal disorders, so any improvement in ergonomic scores may benefit their well-being and career longevity.6,35-7 This provides support for conducting periodic ergonomic self-assessments using quick, objective, and easily-accessible methods such as photography-assisted self-reflection.
Ergonomics training combined with captured photographs has been shown to be a feasible and practical method to improve self-awareness and postures among dental and dental hygiene students.23, 24 Discussions during the training sessions promoted the students' development to become autonomous, self-regulated, and com-petent student clinicians.32 Tendencies among students to overestimate their abilities may hinder the acquisition of knowledge and reduce the ability to improve their work habits.38 The end goal is to develop the automatic reflective practice in self-correction from the continual practice of self-assessment.39 The formation of these habits and the progression of ergonomic self-assessment skills can be promoted throughout their clinical experience as students and later on as practicing dental hygienists.
The present study corroborates evidence reporting that students with self-assessment training (training group) tend to yield more accurate self-assessments of their performance.38 Comparing the agreement between clinician and rater scores, the accuracy of the training groups' ergonomic self-assessment scores improved significantly from week one to week four. The method utilized in the present study combined the independent completion of a self-assessment by the clinician along with formative feedback from the principal investigator. During the self-assessment session, the principal investigator engaged all participants with reflective Socratic questioning (i.e. What do you think about the front to back position of your head?) to provoke the participant to critically think and identify discrepancies in their evaluations. With increasing awareness of a problem, the likelihood of making adjustments to remedy those problems increases. When students overestimate their abilities, this may hinder the acquisition of knowledge or the improvement of their skills.32
Limitations of this study included the use of convenience samples at a single research site, the use of still imaged postures, and the raters' subjective evaluations of angulation of the imaged postures using objective criteria. The DHS had program requirements to purchase and use magnification loupes, and this may have contributed to increased forward flexion, depending on the angle of declination or the mounting of the lenses. Future research studies should include the use of larger sample sizes to increase the generalizability of the results, the use of technology to improve the objective measurement of postures and long-term effects of ergonomics training with photography.
Conclusion
The head and upper arms were identified as the top regions at-risk for musculoskeletal strain based on calibrated rater evaluations of the participant photographs. However, the head and trunk were self-assessed as the top regions at-risk for musculoskeletal strain by dental hygiene students and partitioners. Training involving self-assessment strategies utilizing photographs resulted in improvements in ergonomic scores and the accuracy of ergonomic self-assessments in students and practicing clinicians after four weeks. Improved postures and reduced risks for musculoskeletal disorders may be sustained using photography and periodic ergonomic self-assessments.
Brian B. Partido, RDH, MSDH, PhD is the Executive Director of Dental Programs, Seattle Central College, Seattle, WA, USA; Rebecca Henderson, RDH, MSDH is an assistant professor-clinical, Division of Dental Hygiene, College of Dentistry, The Ohio State University, Columbus OH, USA.
Corresponding author: Brian B. Partido, RDH, MSDH, PhD; brian.partido@seattlecolleges.edu
References
1. Akesson I, Johnsson B, Rylander L, et al. Musculoskeletal disorders among female dental personnel--clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health. 1999 Sep;72(6):395-403.
2. Gopinadh A, Devi KN, Chiramana S, et al. Ergonomics and musculoskeletal disorder: as an occupational hazard in dentistry. J Contemp Dent Pract. 2013 Mar;14(2):299-303.
3. Hayes M, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009 Aug;7(3):159-65.
4. Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg. 2009 Aug;7(3):176-81.
5. Lalumandier JA, McPhee SD, Parrott CB, et al. Musculoskeletal pain: prevalence, prevention, and differences among dental office personnel. Gen Dent. 2001 Mar-Apr;49(2):160-6.
6. Hayes MJ, Osmotherly PG, Taylor JA, et al. The effect of loupes on neck pain and disability among dental hygienists. Work. 2016 Feb;53(4):755-62.
7. Hayes MJ, Taylor JA, Smith DR. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2012 Nov;10(4):265-9.
8. Humann P, Rowe DJ. Relationship of musculoskeletal disorder pain to patterns of clinical care in California dental hygienists. J Dent Hyg. 2015 Oct;89(5):305-12.
9. Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work. 2010 May;35(4):419-29.
10. Barry RM, Spolarich AE, Weber M, et al. Impact of operator positioning on musculoskeletal disorders and work habits among Mississippi dental hygienists. J Dent Hyg. 2017 Dec;91(6):6-14.
11. Crawford L, Gutierrez G, Harber P. Work environment and occupational health of dental hygienists: a qualitative assessment. J Occup Environ Med. 2005 Jun;47(6):623-32.
12. Kagan J. Chap 24 Ergonomics. In: Henry RK, Goldie MP, editors. Dental Hygiene Application to Clinical Practice. Philadelphia, PA: F. A. Davis Company; 2016. p. 394-407.
13. Nield-Gehrig J. Chap 1 Principles of Positioning. In: Nield-Gehrig J, editor. Fundamentals of periodontal instrumentation and advanced root instrumentation. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2017. p. 9-48.
14. Anton D, Rosecrance J, Merlino L, et al. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002 Sep;42(3):248-57.
15. Liss GM, Jesin E, Kusiak RA, et al. Musculoskeletal problems among Ontario dental hygienists. Am J Ind Med. 1995 Oct;28(4):521-40.
16. Sunell S, Maschak L. Positioning for clinical dental hygiene care. Preventing back, neck and shoulder pain. Probe. 1996 Nov-Dec;30(6):216-9.
17. Plessas A, Delgado MB. The role of ergonomic saddle seats and magnification loupes in the prevention of musculoskeletal disorders. A systematic review. Int J Dent Hyg. 2018 Nov;16(4):430-40.
18. Kissell D, Partido BB, Moore W. Magnification and coaxial illumination in dental hygiene education: experience and attitudes of clinical educators. J Dent Hyg. 2019 Feb;93(1):7-15.
19. Kissell D, Partido BB, Moore W. Experience and attitudes regarding requirements for magnification and coaxial illumination among dental hygiene students. J Dent Hyg. 2019 Aug;93(4):24-32.
20. Arnett MC, Gwozdek AE, Ahmed S, et al. Assessing the use of loupes and lights in dental hygiene educational programs. J Dent Hyg. 2017 Dec;91(6):15-20.
21. Garbin AJ, Garbin CA, Diniz DG, et al. Dental students' knowledge of ergonomic postural requirements and their application during clinical care. Eur J Dent Educ. 2011 Feb;15(1):31-5.
22. Burk T, Orellana M. Assessment of graduate orthodontic programs in North America. J Dent Educ. 2013 Apr;77(4):463-75.
23. Partido BB. Dental hygiene students' self-assessment of ergonomics utilizing photography. J Dent Educ. 2017 Oct;81(10):1194-202.
24. Partido BB, Wright BM. Self-assessment of ergonomics amongst dental students utilising photography: RCT. Eur J Dent Educ. 2018 Nov;22(4):223-33.
25. Branson BG, Williams KB, Bray KK, et al. Validity and reliability of a dental operator posture assessment instrument (PAI). J Dent Hyg. 2002 Fall;76(4):255-61.
26. Maillet JP, Millar AM, Burke JM, et al. Effect of magnification loupes on dental hygiene student posture. J Dent Educ. 2008 Jan;72(1):33-44.
27. Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005 Mar;85(3):257-68.
28. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med. 2012 Oct;22(3):276-82.
29. Guggenmoos-Holzmann I. The meaning of kappa: probabilistic concepts of reliability and validity revisited. J Clin Epidem. 1996 Jul;49(7):775-82.
30. Anghel M, Argeanu V, Talpo-Niculescu C, et al. Musculoskeletal disorders (MSDS)- consequences of prolonged static postures. J Exp Med Surg Res. 2007 Sep;14(4):167-72.
31. De Sio S, Traversini V, Rinaldo F, et al. Ergonomic risk and preventive measures of musculoskeletal disorders in the dentistry environment: an umbrella review. PeerJ. 2018 Jan;6:e4154.
32. Gadbury-Amyot CC, Woldt JL, Siruta-Austin KJ. Self-assessment: A review of the literature and pedagogical strategies for its promotion in dental education. J Dent Hyg. 2015 Dec;89(6):357-64.
33. Warren N. Causes of musculoskeletal disorders in dental hygienists and dental hygiene students: a study of combined biomechanical and psychosocial risk factors. Work. 2010 May;35(4):441-54.
34. Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders in a 3 year longitudinal cohort of dental hygiene students. J Dent Hyg. 2014 Feb;88(1):36-41.
35. Hayes MJ, Osmotherly PG, Taylor JA, et al. The effect of wearing loupes on upper extremity musculoskeletal disorders among dental hygienists. Int J Dent Hyg. 2014 Aug;12(3):174-9.
36. Howarth SJ, Grondin DE, La Delfa NJ, et al. Working position influences the biomechanical demands on the lower back during dental hygiene. Ergon. 2016 Apr;59(4):545-55.
37. La Delfa NJ, Grondin DE, Cox J, et al. The biomechanical demands of manual scaling on the shoulders & neck of dental hygienists. Ergon. 2017 Apr;61(1):127-37.
38. Mould MR, Bray KK, Gadbury-Amyot CC. Student self-assessment in dental hygiene education: a cornerstone of critical thinking and problem-solving. J Dent Educ. 2011 Aug;75(8):1061-72.
39. Bowers JA, Wilson JE. Graduates' perceptions of self-assessment training in clinical dental hygiene education. J Dent Educ. 2002 Oct;66(10):1146-53.