You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Setting It Straight – Advanced Orthodontics
Lori Garland Parker, RDAEF, BS, MAOM
Orthodontic treatment involves movement of malpositioned teeth to orthodontically straighten
or correct their positions. In traditional orthodontics, small orthodontic appliances, known as brackets, are connected to exterior surfaces of the patient's teeth, and an archwire is placed in a slot of each bracket to move the teeth. The archwire forms a track that guides movement of the teeth to the desired positions for correct occlusion. End sections of the archwire are placed through appliances known as buccal tubes. The buccal tubes are either bonded or welded to bands and cemented onto the patient's molar teeth (Figure 1).
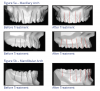
In recent years it has become common practice to bond orthodontic appliances to the labial or lingual surfaces of the tooth, using either direct or indirect methods. Although bands are still used, bonded appliances are becoming more common (Figures 2 and 3).
Andrews' Six Keys to Normal Occlusion
In September of 1972, Lawrence F Andrews published an article in the AJO-DO titled The Six Keys to Normal Occlusion, where he shared his observations of 120 casts of non-orthodontic patients with normal occlusion. His contributions form the essential basis of orthodontic treatment today.
Key I - Molar Relationship
According to Andrews' definition, normal occlusion exists when the mesiobuccal cusp of the maxillary first permanent molar occludes in the groove between the mesial and middle buccal cusps of the mandibular first permanent molar (Figure 4, also known as Class I dental occlusion).
Key II - Crown Angulation (tip)
The gingival portion of the crowns of all teeth is more distal than the incisal or occlusal portion of the crowns. The long axis of all crowns of the teeth (with the exception of the molars) is considered the main mid-development ridge of the facial surfaces of the teeth. The long axis of the crown of the molar teeth is considered to be the buccal groove and its extension to the gingiva (Figure 5a and 5b).
Key III - Crown Inclination (torque)
This refers to the labio-lingual axial inclination of the anterior teeth and bucco-lingual axial inclination of the posterior teeth. This is measured from a perpendicular to the occlusal plane to the crown long axis tangent to the mid-point of the middle of the crown. If the crown is facial to the tangent, it is said to have positive torque. If the crown is lingual to the tangent, it has negative torque. The upper incisors usually have positive torque; the lower incisors usually have slight negative torque. From the upper canine distally, the torque becomes progressively negative. Figure 6 shows crown inclination before and after orthodontic treatment.
Key IV - Rotation
The fourth key to optimal occlusion is absence of tooth rotations (Figures 7a and 7b).
Key V - Tight Contacts
There should be no spaces between the teeth. Contact points should abut unless a discrepancy exists in a mesiodistal crown diameter.
Key VI - Curve of Spee
The depth of the curve of Spee should be fairly flat ranging from 0.5 mm to 1.5 mm at its deepest point. An average curve of Spee is 1 mm. Figure 8 illustrates curves of Spee before and after treatment.
Potential Risks and Limitations of Orthodontic Treatment
As with any medical or dental procedure, there are risks and limitations of orthodontic treatment. Before orthodontic treatment is initiated, the following topics should be discussed with the patient and/or parent.
Decalcification
Decalcification is the white chalky marks on teeth caused from the patient leaving plaque on the teeth for an extended period of time. To prevent decalcification from occurring, good oral hygiene must be performed. Stress the importance of home care at the exam appointment and ensure that the entire dental team supports this philosophy. Monitor toothbrushing at each appointment and keep the patient/parent informed of the status. Chart any pretreatment decalcification, evaluate oral hygiene, and review techniques as needed at each visit.
Root Resorption
When moving teeth orthodontically, it is common to have some shortening of the roots. The orthodontist evaluates the length of the patient's roots at the beginning of treatment and discusses any concerns. (If a precondition is present, it should be discussed and noted in the chart.) The orthodontist typically monitors root length by taking an x-ray every 12 months throughout treatment and provides the patient and parent with updates as needed.
Periodontal Involvement
Successful orthodontic treatment requires a healthy mouth. Periodontal disease involves the loss of gingiva and alveolar bone support, so teeth need to be kept very clean. Emphasize the importance of oral hygiene with the parent/patient and encourage orthodontic patients to continue to see their primary care dentist regularly throughout orthodontic treatment. (If a precondition is present, discuss it with the patient/parent and note it in the chart.) Note any pre-treatment pockets and if necessary, refer the patient to the primary care dentist or periodontist. Prophylaxis is recommended every 6 months unless the patient has a periodontal condition that calls for more frequent hygiene appointments (for example, every 3 months or as recommended).
Temporomandibular Joint (TMJ)
The TMJ is the jaw joint. Ask the patient to report any jaw clicking, popping, or discomfort during pre-treatment or during treatment. TMJ dysfunction may occur before, during, or after treatment. When discovered, a variety of symptoms and treatments should be discussed with the orthodontist and as appropriate, other health-care professionals.
Non-Vital Teeth
The patient medical history form should include questions on traumas or injuries to the teeth or
face. Previous trauma may cause a tooth to become non-vital. If a precondition is present, discuss with the patient/parent and note it in the chart. Orthodontic treatment can sometimes stimulate an old injury and cause the tooth to become non-vital. Ask the patient to keep the doctor informed of any symptoms associated with traumatized teeth.
Orthodontic Materials
During treatment, different small appliances are used in the mouth. Inform patient/parent of this aspect of treatment and ask that they call if anything becomes loose or is swallowed.
Impaction
Impaction refers to teeth that are having difficulty erupting. The orthodontist should discuss any potential impaction concerns with the patient/parent.
Growth Patterns
Growth patterns can change, and they vary with each individual during and after orthodontic treatment. As these changes are controlled by nature, the orthodontist should explain that the patient's growth must be monitored, and if necessary, treatment adapted accordingly. Note any remarkable family history in the chart.
Treatment Time
Duration of treatment can be estimated based on the type and difficulty of the required treatment. Patient cooperation also plays a role in the length of orthodontic treatment. Emphasize the importance of keeping regular appointments, maintaining proper oral hygiene, and avoiding foods and habits which can cause loose or broken bands, brackets, and wires.
Relapse
Relapse refers to the shifting of teeth following treatment. Stress the importance of retainer wear and follow up appointments.
Early Treatment
As noted in "Wired for Learning - Orthodontic Basics," the American Orthodontic Association recommends that children have their first orthodontic examination by age 7, or earlier if an orthodontic problem is detected by parents, the family dentist, or the child's physician. In some cases, early intervention that utilizes the patient's growth can make corrective treatment faster and easier.
Some young patients can benefit from a two-phase approach to orthodontic correction. Early treatment, sometimes referred to as Phase I, can correct major orthodontic problems early and guide jaw growth. In some cases, such treatment can reduce the need of orthognathic surgery as an adult and/or reduce the time required in traditional orthodontic appliances.
Early treatment can include expansion appliances that widen the arch, making room for the permanent dentition. In other cases, orthopedic appliances can be used to guide jaw growth. Other Phase I treatment reduces crowding or closes anterior spaces. The depth and appropriateness of Phase I treatment varies from patient to patient and according to the treatment philosophies of the orthodontist.
Typically, patients are given a "rest period" between phases, and once the patient has full permanent dentition, Phase II treatment is initiated to fine-tune correction. This approach reduces the time in treatment during the most critical teenage years.
Orthognathic Surgery
Orthognathic surgery combines orthodontic treatment with surgery of the jaw to correct or establish a stable functional balance between the teeth, jaws and facial structures. The goal of maxillofacial surgery is to treat any jaw imbalance and the resulting malocclusion, which could adversely affect the cosmetic (esthetic) appearance as well as the proper functioning of the teeth. To correct musculoskeletal, dento-osseous, and soft tissue deformities of the jaws and associated structures, this approach involves diagnosis, treatment planning, and execution of treatment that combines orthodontics and oral/maxillofacial surgery.
The term "orthognathic" was coined by an oral/maxillofacial surgeon to mean "straight jaws," just as orthodontics means "straight teeth." Prior to that time, the terms "surgical orthodontics" and "facial orthopedics" were used to describe the field.
Orthognathic surgery is appropriate when the jaws do not meet correctly and/or teeth don't seem to fit with the maxillary and mandibular jaws. The teeth are straightened using orthodontics, and corrective jaw surgery repositions the malaligned jaws. This not only improves the facial appearance but also ensures that teeth meet correctly and function properly.
Many different types of abnormalities of the jaw structures can result in facial deformity and malocclusion. These abnormalities in the jaws and facial bones may be congenital (present at birth) or surface during growth and development. They also may be acquired after birth as a result of hereditary, environmental influences, or trauma/illness to the face.
It has been estimated that dentofacial deformities affect up to 20 percent of the population. Any individual with difficulty in the following areas should be evaluated for possible orthognathic surgery:
• Difficulty in chewing, biting or swallowing
• Speech problems
• Chronic jaw or TMJ pain
• Open bite
• Protruding jaw
• Breathing problems
Goals
The specific goal for orthognathic surgery varies from patient to patient, depending on the actual diagnosis. In general, the team will address:
• Function: Restore normal chewing, speech, ocular (eye) function, respiratory function;
• Esthetics: Establish facial harmony and balance;
• Stability: Avoid short- and long-term relapse; and
• Minimizing treatment time: Provide efficient and effective treatment.
Evaluation and Diagnosis
The most important aspect of overall patient management is thorough evaluation and diagnosis. Patient evaluation for orthognathic surgery can be divided into four main areas:
1. Patient concerns or chief complaints
2. Clinical examination
3. Radiographic and imaging analysis (x-rays)
4. Dental model analysis
After an examination by each of the orthognathic surgery team members (dentist, orthodontist, and maxillofacial/oral surgeon), a diagnosis and coordinated treatment plan is prepared. The complete treatment plan usually is implemented in several stages over the course of 1 to 2 years.
Treatment Process
Any general dental maintenance, prevention, or restoration procedures should be performed prior to orthodontic and surgical intervention. The first stage of orthognathic treatment is the alignment of the teeth into a stable relationship with the underlying jaw by orthodontics. This step, which prepares the dental arches for the surgical repositioning, usually takes the longest amount of time, averaging from a few months to over a year. At this stage, the abnormal bite (malocclusion) may become more noticeable. Once ready for the surgical procedures, the orthodontist and maxillofacial surgeon review photographs, x-rays, and dental models to finalize the surgical plan. The operation may involve a single jaw or both the maxilla and mandible. The surgery also may be combined with other procedures, such as rhinoplasty (nose correction) or genioplasty (chin correction) to improve the general appearance of the face.
The surgical procedure may take two to four hours, depending on the complexity of the case. Most patients are kept in the hospital for two to five days, again depending on the specifics of the procedure and post-operative condition. Most patients return to their normal activities within a week or two of their surgery. The surgeon monitors healing and reviews the changes in the facial structures and occlusion (bite). The orthodontist adjusts the braces to fit the patient's new repositioned jaw. Orthodontic treatment may continue for several months to ensure optimal positioning of the teeth.
Table 2 illustrates situations that lend themselves to orthognathic surgery.
Orthodontic Records
Cone beam 3D dental imaging is becoming more popular to gather information needed to evaluate and diagnose a case. 3D views are used to analyze teeth, roots, TMJ, airway, and sinuses without magnification or distortion. Practice efficiency can be enhanced by capturing a complete workup in less than 10 seconds. This is especially helpful when the practitioner intends to place TADs or when knowing the exact position of teeth is important to determine the best treatment plan. A virtual study model can be utilized to prevent the need for taking study model impressions (Figure 9).
Basic Orthodontic Instrumentation
As with any dental specialty, orthodontics has a series of instruments that makes delivery easier. Table 3 describes common orthodontic instrumentation.
Self-Ligating Orthodontic Brackets
New bracket designs are continually being introduced to entice orthodontists, each promising increased control, easy placement, and an aid to finishing. A popular variation of the traditional bracket is a reduced-friction, ligatureless design that does not require the typical elastic (Figure 10a) or metal tie to engage the archwire into the bracket (Figure 11). Elastic ties can degrade over time, reducing effectiveness (Figure 10b). Instead, this type of bracket contains a clip that opens and closes. When closed, the clip holds the archwire in place. Although the concept of a ligatureless bracket was introduced in 1935 the design essentially laid dormant for the next 40 years or so. Since the 1970s, however, several ligatureless designs have emerged and are becoming a popular choice in orthodontics (Figure 12).
Rapid leveling and alignment of the dentition has been observed in many patients treated with self-ligating appliances. It should be noted that finishing may be more difficult with these brackets than with standard pre-adjusted edgewise brackets.
Advantages of Self-Ligating Brackets
Theses advantages apply to all self-ligating brackets, although different brands can vary in their ability to consistently deliver these benefits in practice.
Secure, full-archwire engagement
Full engagement is a feature of self-ligation. The bracket's clip/slide is either fully shut or it is not; unintentional partial engagement is not possible. Because no elastic ligature is required, ligature decay (Figure 10a and 10b) also is not a problem. However, security of ligation depends on the clip/slide being robust and not inadvertently opening. Until very recently, this requirement for security of performance was not fully met by self-ligation designs. Secure, full-archwire engagement maximizes the potential long range of action of modern wires and minimizes the need to regain control of teeth when full engagement is lost during treatment.
Low friction
During orthodontic tooth movement with the preadjusted edgewise system, friction generated
at the bracket-archwire interface tends to impede the desired movement. The method of ligation is an important contributor to this frictional force. Traditionally, elastic ties have been used to secure the archwire into the slot (Figure 11), which created significant friction. The friction generated by a self-ligating bracket is dramatically lower than for elastomeric rings with conventional brackets. This seems to be an inherent characteristic of self-ligating brackets.
Secure archwire engagement and low friction as a combination
The combination of very low friction and very secure full archwire engagement is likely to be the most beneficial feature of self-ligating brackets. This combination enables a tooth to slide along an archwire with lower and more predictable net forces, and yet under complete control, with almost none of the undesirable rotation of the tooth that can result from deformable modes of ligation (such as elastomeric tie).
Alignment of severely irregular teeth
The combination of low friction and secure full engagement also is particularly useful in the alignment of very irregular teeth and the resolution of severe rotations. In these cases, the capacity of the wire to slide through the brackets of the rotated and adjacent teeth significantly facilitates alignment. Low friction facilitates rapid alignment and more certain space closure; secure bracket engagement permits full engagement with severely displaced teeth without compromising control as the teeth slide teeth along an archwire. Modern archwires substantially enhance our ability to harness these benefits.
Less chairside assistance and faster ligation/archwire removal
The original motive in developing earlier self-ligating brackets was to speed ligation. Time saved depends on the bracket and the experience of the operator.
Disadvantages of Self-Ligating Brackets
As with any new system, operators experience a learning curve with a different bracket design and movement system. Self-ligating brackets require a different mind set in bracket placement, archwire selection, and finishing techniques.
Bracket Placement
Proper placement of the orthodontic brackets and bands is essential to achieving optimum treatment results within the projected treatment time. Accurate bracket placement has long been recognized in orthodontics as the single most critical determinant of efficient tooth movement. Until the late 1970s, orthodontists placed nonprescription brackets on the teeth, and archwires were carefully fabricated by the orthodontist for each patient. The development of straightwire appliances greatly reduced the amount of archwire bends required. However, the bracket prescriptions are based on averages, so many patients still require archwire adjustments to finish the case.
No matter what type of bracket is used or where it is placed, a bracket must stay attached to the tooth to do its job. Therefore, precise chairside technique is critical for success.
Dimensions Of Bracket Slots
The archwire fits into a slot machined into the orthodontic bracket. The two most common dimensions of traditional orthodontic bracket slots are 0.018-inch and 0.022-inch. Separated by four thousandths of an inch, these sizes present a somewhat unusual description in a metric modern world, where the scientific community measures in millimeters and micrometers. The size indicates the largest round, square, or rectangular archwire that can be used. Smaller wires have more "play" in the slot as compared to a full-size archwire (Figure 13).
The 0.022-inch slot was the first to be introduced, and it suited the gold wires that were commonly used in the early 1900s.
Bonding Using Light-Cure Adhesive
The most common adhesive system today is the light-cure system where resin is placed on the
tooth and a paste placed on the bracket. A rapid polymerization of the bonding material occurs when visible light is applied. The bonding material is cured under brackets by direct illumination from different sides as well as by transillumination when tooth structure transmits visible light. In recent years, alternatives to conventional halogen lights offering reduced curing time have emerged. Light-emitting diodes (LEDs), and plasma arc lights are becoming more popular; however, studies have shown that there is no statistical difference in the quality of bond strength.
Advantages of light cure materials include:
• Good bond strength,
• Ample working time (depending on ambient light situation), and
• Fast curing time, especially for re-bonds.
Disadvantages of light cure materials include:
• Longer curing time compared to chemical cure systems on full-mouth bondings, and
• Care is required when working in ambient light, and a curing light is required.
The basic steps involved are summarized in Table 4.
Advances in Bonding Brackets
Indirect Bonding
Indirect bonding is a method of placing brackets on dental models in the laboratory (Figures 14 and 15), then making a transfer tray that is used to bond the brackets onto the patient's teeth, an entire arch at a time (Figures 16 and 17). Because this approach
offers improved access and time availability in the laboratory, it has been suggested that this technique may allow more precise bracket location.
Advantages of indirect bonding include:
• Increased accuracy of bracket placement (working on a model, there are no lips or cheeks to obscure the operator's view),
• Less repositioning needed,
• Major reduction of doctor time,
• Ergonomically healthier,
• Better staff utilization,
• Shorter chair time,
• Increased patient comfort due to shorter appointment,
• No bands (and in turn, reduced band inventory, no band spaces, and better gingival heath),
• Potentially shorter treatment time, and
• Bracket failure rates comparable to that of conventional direct bonding.
Disadvantages of indirect bonding include:
• Technique sensitivity,
• Additional staff training required,
• Additional cost of materials, and
• Cannot be used for patients with mixed dentition (unless completed in-house with 2-day turnaround or less).
Banding
Bands can tolerate more force than brackets and as such, are most commonly used in the posterior, where most chewing occurs, however most practitioners are bonding all teeth. In today's orthodontic practices, typically only appliances such as Rapid Palatal Expanders and Herbst utilize bands.
When bands are needed, band selection requires the ability to visualize the size and shape of a tooth. Once the appropriate size band is determined, a final adaptation of the band to the patient's tooth is necessary (Figure 18).
There must be enough space between the teeth to fit the band. If the contacts are tight, separators are typically placed for one week to slowly make just enough space for a band to slide between the contacts. If the contacts are too tight, proper size determination may be difficult and the procedure may be unnecessarily uncomfortable for the patient and the operator.
Archwires
Technological advances in archwires also have graced the profession over the years. The gold and nickel silver wires of Angle's era were augmented by stainless steel in the 1950s. Soon to follow was Elgiloy™ wire, which mimics some of the properties of gold wire at a fraction of the cost and without some of the drawbacks that came with stainless steel. Next to emerge, Australian "wildcat wire™" provided greater resiliency than previously existing wires. Beginning in the 1980s, a continual progression of "Space Age" wires have been developed through the NASA space program. These resilient metal wires are more flexible and retain their pre-formed shape.
Three alloys are most commonly used on orthodontic archwires today, each with its own advantages and disadvantages.
Nickel Titanium
Nickel titanium (NiTi) wires are very flexible but cannot be deformed. The alloy has "memory," meaning that it wants to return to its original shape. This wire is most commonly used in the initial alignment phase of orthodontic treatment.
Advantages:
• The small, round diameter wires can be "bent," but not deformed, so they can be placed in each bracket even when the brackets do not align.
• As the wire returns to its original shape, it moves the teeth in that direction via the bracket tie (or closed slot in a self-ligating bracket).
Disadvantages:
• These wires cannot be bent unless they are heated, at which time they become "dead soft" and cannot move teeth.
• Nickel Titanium is brittle. Archwires of this material break if repeatedly flexed.
Copper Nickel Titanium
The addition of copper to the nickel-titanium mix gives a wire the advantage of changing properties with changes in temperatures. This type of archwire is most commonly used in the initial alignment phase.
Advantages
• Chilling the archwire can simplify ligation. Using "endo ice" spray, an ice cube, or even cold air from the air syringe temporarily "dead softens" the archwire, allowing the operator to passively place it in each bracket while tying it in place.
• As the wire warms with exposure to body temperature, it exerts more and more force, thus moving the teeth like the traditional NiTi archwire.
Disadvantages
• These archwires cannot be bent unless heated, and then the material becomes "dead soft" and will not move teeth.
• Copper-nickel-titanium is a brittle alloy. These wires break if repeatedly flexed (Figure 19).
Stainless Steel
This alloy has tremendous strength and the capacity to exert or resist great forces.
Advantages
• When used to close spaces between teeth, stainless-steel wires resist the tipping forces of chain, allowing tooth roots to move together in a more parallel fashion.
• A large-diameter stainless steel wire can allow the full expression of the bracket prescription
and tip/torque roots into their ideal positions.
• Because stainless steel can accept a bend, these wires can be used to "detail" a case, that is, they can be bent to allow specific movements of specific teeth to improve their position.
Disadvantages
• Stainless steel can be distorted (for example, if the patient bites on something too hard,
it can permanently deform the archwire).
• Stainless steel also is not very flexible. The bracket slots must be closely aligned for it to thread into position, depending upon the size of the archwire.
Temporary Anchorage Devices (TADs)
Newton's Law tells us that for every action, there is an equal and opposite reaction. In orthodontics, in order to move misaligned teeth, other teeth are used as an anchor to push or pull against. This can sometimes cause undesired side effects. In cases where anchorage is needed without the equal and opposite movement, TADs can be used. Temporary anchorage devices, or TADs, are small anchors usually made of titanium or other biocompatible metal,
which are temporarily fixed to the bone to serve as anchorage. For example, a TAD (also called a mini screw) may be used when the orthodontist wants to move a group of teeth distally to close an extraction space. Without a TAD or extra oral device such as a headgear, the posterior teeth are pulled against the anterior teeth, causing the unwanted movement of the posteriors moving forward while the anteriors are moving back. With a TAD, the spaces can be closed with no forward movement of the posterior segment (Figure 20).
Accelerated Orthodontic Devices
Accelerated orthodontic devices are removable and non-invasive appliances which generate high frequency vibrations to the teeth and surrounding bone. This vibration is said to enhance the movements directed by the orthodontist, allowing for faster tooth movement. The patient typically wears the appliances for 5 to 20 minutes per day depending on the device (Figures 21 and 22).
Computer Technology In Orthodontics
Evolving technology and integration of digital solutions in orthodontics has transformed diagnosis and treatment planning for many orthodontists from a traditional two-dimensional (2D) approach into an advanced three-dimensional (3D) process.
3D Scanning
The opportunity to replace impressions with a comfortable intra-oral scan is great news for patients and orthodontic teams. The clinician captures the dentition with a scanner wand to create a 3D digital representation. In many cases, a full mouth scan can be completed in less than 3 minutes, creating a digital model. Increased accuracy, time efficiency and lowered cost of intraoral scanners have contributed to their growing popularity in orthodontic offices. Studies have shown that the accuracy of intraoral scans is equal or better compared with conventional impressions. With traditional models, problems are sometimes found after pour up. With modern digital scanning software, the operator is notified in actual time if the scan is not sufficient. The software confirms accuracy while the patient is in the chair, so there is no need for a patient to return due to inaccuracies (Figure 23).
Digital Models
Digital study models offer a reliable alternative to traditional plaster models. Beginning with the ease of scanning the patient's dentition rather than impressions, the advantages also include easy and fast electronic transfer of data, immediate access, and no physical model storage requirement. Storing digital models in "the cloud" prevents the need for large digital storage. Digital models can be easily integrated into the office practice management system and the clinician can simulate various treatment plans, specify bracket placement, and prepare cases for indirect bonding or other appliances. CBCT and digital models can also be merged to help treatment planning of orthognathic cases and determine proper placement of temporary anchorage devices (TADs). If a physical model of the dentition is required for the manufacture of an orthodontic appliance or other use, digital models can be 3D printed from a STL file (Figure 24).
3D Printing
3D printing is a process of making three dimensional solid objects from a digital file. The 3D printing process begins with a 3D model, virtually designed or obtained through scanning the patient's dentition. The software divides a 3D model into hundreds or thousands of horizontal layers and is called slicing. The creation of a 3D printed model is achieved by laying down successive layers of material until the object is created. Each of these layers can be seen as a thinly sliced horizontal cross-section of the eventual object. The printer quickly creates accurate, smooth orthodontic models and allows users to automate their entire workflow from a digital file to model fabrication - significantly accelerating production times and increasing capacity (Figure 25). Elimination of traditional impressions and pouring models enhance practice efficiency, patient and staff satisfaction for a fully integrated digital and streamlined workflow.
Advantages of digital model printing:
• Digitizes orthodontic workflow from 3D file
to model or appliance fabrication
• Eliminates discomfort and inconvenience of physical impressions
• Can send file while patient is in the chair, eliminating multiple additional in-office steps
• Eliminates mess of pouring impressions
Disadvantages:
• High initial cost of the unit
• 3D software and scanner required
• Possible ongoing higher cost of materials as compared to plaster
• Additional counter space required
3D model files can be sent to a laboratory immediately after scanning and a 3D model printed
or appliance fabricated.
Traditional workflow for creating a lab appliance
1. Impression
2. Pour up model
3. Pack up and send to lab
4. Lab fabricates appliance
5. Send appliance back to office
6. Deliver appliance to patient
Digital workflow for creating a lab appliance
1. Digital Scan and send file to a lab in seconds
2. 3D printing and/or appliance fabrication at outside or in-office lab
3. Send appliance back to office if off site
4. Deliver appliance to patient
As costs continue to decrease and the speed of the process accelerates, more orthodontic laboratories and individual orthodontic offices are investing in this state-of-the-art technology, as workflows are much more efficient, justifying the initial and on-going financial investment.
Digital Bracket Removal
Traditionally at the end of treatment, the patient's orthodontic appliances were removed and an impression taken to fabricate a retainer. The patient would return several days later to get their retainers. Another advancement in technology today is software which allows practices and labs to digitally remove brackets from STL files. The software can carve, build, smooth and create margins to refine the tooth surface. Once the brackets are digitally removed, retainers can be made so the patient can receive retainers the same day as the appliances are removed saving a trip to the office.
Robots in Orthodontics
Intraoral scanning and the use of robots to fabricate patient-specific archwires is now being introduced to the orthodontic profession (Figure 26). The scanner is an intraoral three-dimensional (3D) imaging device based on white light and active triangulation. The software allows for interactive 3D viewing of the malocclusion and a fine tuning of diagnostic set-ups to customize occlusion goals. The robot customizes the patient's archwires per the orthodontist's virtual treatment plan.
Patient-Specific Brackets
Another new technology for orthodontics is patient-specific bracket design and fabrication using CAD-CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology. A three-dimensional model of the patient's malocclusion is produced, and software is used to indicate where the orthodontist wants the teeth to be positioned. Brackets are then manufactured to the patient's specific prescription needs. Research in this area has progressed over the past 10 years, fine-tuning the technique in preparation for the mass market.
Computer-Aided Bracket Placement
To enhance the accuracy of bracket placement, a company has designed a bracket placement wand that includes a miniature video camera. The camera transmits real-time images from the patient's mouth to the screen (Figure 27), and when the software detects a match between the projected image and the clinician-prescribed position (Figure 28), an audio-visual signal is delivered so the doctor can accurately bond the appliance.
Completely Customized Lingual Orthodontic Brackets
A lingual orthodontic technique is available in which the brackets are completely customized and fabricated one at a time with each patient's unique prescription built into the bracket. All the archwires required for the patient's treatment are bent by a robot and are included as part of the system.
Sequential Plastic Aligners
Sequential Plastic Aligners (Figure 29) are a series of clear, precision polymer aligners that incrementally straighten teeth. At each stage, tooth movement is controlled and predetermined for that particular stage. The number of aligners vary depending on the complexity of the treatment and doctor preference and orthodontic goals. Aligners were first introduced to the profession in the late 1990's by Align Technology, Inc. (San Jose, CA) and are still the largest company providing clear aligners. Align Technology also developed advanced 3D tools to simulate tooth movement in progressive stages of correction, along with iTero, a 3D intraoral scanner. This allowed for a seamless system to communicate with the company in order to efficiently fabricate the aligners. However, expiring patents now allow other companies to compete with Invisalign in this orthodontic market. Due to competition, marketing and increased patient interest, aligner therapy is becoming a popular mode of orthodontic treatment.
Using a precise three-dimensional analysis of the patient's teeth and adjacent tissue, personalized aligners are crafted for each patient. Each aligner is worn for one to two weeks, and can be removed to eat, brush, and floss. During wear, the patient's teeth are gently moved to their ideal position. Commonly, clear attachments are bonded in strategic locations on specific teeth to aid in tooth movement. Clear buttons may also be bonded directly on the teeth or appliance to allow elastics to be worn. The length of treatment depends on the patient's treatment plan.
3D Printing and In-Office Aligners
With the high cost of Invisalign and other similar products, orthodontists are evaluating clear aligner options. Now that in-house 3D printing is available, fewer practices are sending STL files to outside labs for model printing and choosing to make their aligners in-house. What was once a 10-day to 2-week process can now be achieved in less than a day.
An intra-oral scan is taken and imported into treatment planning software. The doctor then stages the sequence of 3D models showing the progressively corrected alignment of the teeth. The file is exported for each stage to the 3D printer and a printed model is made. A thermoforming machine is then used to fabricate each aligner. The challenge for this option
is that additional space is needed for the equipment and typically more staff is needed so the cost benefit needs to be calculated.
In the near future, software enhancements will allow the fabrication of aligners without the need to print models first, saving valuable time and money.
Direct-to-Consumer Aligners
SmileDirectClub, LLC is one of many companies who are marketing directly to the consumer with the goal of lower treatment cost and to bypass the need for visits to the orthodontist.
Patients can either book a 3D image SmileShops, which are located around the country, or have an at-home kit mailed. A dentist or orthodontist will review the records and arrange to have aligners made. This option is typically used for more simple cases such as a minor diastema, yet, without full orthodontic records and orthodontic exam, less than ideal results are common and can lead to potentially irreversible and expensive damage such as tooth and gum loss, changed bites, and other issues, some of which may not arise immediately. With no orthodontic x-rays, evaluation of dental health or supervision, this mode of treatment is very risky and may not live up to the company's claims.
Since July of 2019, The American Association of Orthodontists ("AAO") has serious concerns about direct-to-consumer orthodontics when it sees over 935 "Customer Complaints" on the Better Business Bureau's website for SmileDirectClub, LLC.
See the Consumer Alert from the AAO:
https://www.aaoinfo.org/_/online-orthodontic-companies/
State Dental Practice Acts
Most state dental practice acts define conditions under which a dental auxiliary may perform specific duties. Several orthodontic procedures in many states can be delegated to dental assistants, for example, placement or removal of archwires, preparation for bonding brackets, fitting orthodontic bands, and in some cases, bonding of orthodontic appliances. Laws vary from state to state, ranging from delegation of nearly all reversible procedures to minimal delegation. For more information on individual state laws, contact the State Board of Dental Examiners for the state of interest.
Facts about State Dental Practice Acts
They establish eligibility and criteria for licensure and identify grounds for suspension or revocation of license.
• State dental practice acts are implemented for the protection of the public.
• They establish education, credentialing, and licensure requirements for any dental auxiliaries recognized in the state practice act. These requirements may address:
- o continuing education,
- o the use of ionizing radiation, and
- o infection control regulations.
• State practice acts establish the State Board of Dental Examiners (State Board of Dentistry).
• The acts control assignment of duties in a given state. - o Open provision allows a dentist to delegate any function within the scope of the auxiliary's competence.
- o List of permitted functions uses an itemized list of approved duties for auxiliaries.
Common terms used in dental practice acts include:
• Patient of record - One who has been examined and diagnosed by a licensed dentist and whose treatment has been planned by that dentist.
• Assignment/delegation - The dentist appointing a dental auxiliary to perform a specific procedure on a designated patient of record. The dentist need not be physically present in the office or in the treatment room at the time the procedure is being performed.
• Direct supervision - The dentist has designated a patient of record upon whom services are to be performed by an auxiliary while the dentist is in the office. The dentist has described the procedure to be performed, examines the patient before prescribing the procedures, and examines the patient again when the procedure is completed.
• General supervision - The dentist has authorized and delegated specific procedures that may be performed by a qualified dental auxiliary for a patient of record. The dentist need not be physically present in the office at the time the procedures are being performed.As noted above, the laws, licensure, and delegation requirements vary significantly from state to state. For more information on individual state laws, contact the State Board of Dental Examiners for the state of interest.
Summary
During the last decade, the specialty of orthodontics has undergone a technological revolution. New materials and techniques have been developed that can make braces less noticeable, improve patient comfort, and in some cases, reduce treatment time and help control costs. Like any area of health care, orthodontic theories and techniques are constantly being improved. In today's health-conscious society, where physical appearance is important, advancements in care continue to popularize orthodontics.
GLOSSARY
Abut - adjacent to.
Active triangulation - technique that allows for precise three-dimensional scans without the need for a fixed point of reference.
A-lastic - small round elastic tie used to hold the archwire into the bracket slot; also known as "O" ring, "O" tie, elastomeric tie, or ligation module.
Alloy - two or more metals mixed together to form a new metal.
Buccal tube - small metal part welded onto the outside of a molar band or bracket; it contains slots to hold archwires, lip bumpers, facebows, and other auxiliaries.
Classification (dental) - system of classifying the relationship of the upper teeth to the lower teeth.
Classification (skeletal) - system of classifying the position of the maxilla in relation to that of the mandible (this system does not reference the teeth).
Clear Aligner Therapy - orthodontic treatment consisting of a series of customized clear removable appliances made from thermoplastic material that gradually move teeth by applying gentle, consistent pressure to a patient's teeth.
3D Printing - a process of making three dimensional solid objects from a digital file.
Dentofacial - involving the teeth and face.
Digital Models - Electronic study casts made from an intraoral scan that can be saved and viewed three-dimensionally on a computer.
Gnathic - pertaining to the jaws.
Keys to Occlusion - characteristics shared by individuals with both optimal occlusion and balanced faces, as identified by Dr. Lawrence F. Andrews.
Maxillofacial- pertaining to the jaws and the face, particularly with reference to specialized surgery of this region.
Ortho- prefix meaning straight or correct.
Orthognathic surgery- procedure combining orthodontic treatment with surgery of the jaw to correct or establish a stable functional balance between the teeth, jaws, and facial structures.
Root resorption- shortening of the roots; resorption of cementum and underlying root dentin.
Spee, curve of- curvature of the occlusal plane of the teeth.
Tangent- line or plane that touches a given curve or solid at a single point.
Torque- movement of the crown of a tooth in one direction and its root in the opposite direction.
Transillumination- the shining of a light through a tooth.
White light - non-invasive light that can be used repeatedly without adverse effects on patients during bonding procedures.
REFERENCES
Andrews LF. The six keys to normal occlusion. Am J Orthodon 1972;62:296-309.
Craniofacial Anomalies Center at Stanford University. Orthognathic (maxillofacial) surgery. Available at http://craniofacial.stanford.edu. Accessed December 2005.
Swartz M. Titanium archwires - understanding their unique properties to maximize their potential. Presented at: American Association of Orthodontists 105th Annual Session; May 24, 2005; San Francisco, CA.
American Association of Oral and Maxillofacial Surgeons. Oral and Maxillofacial Surgery Terminology. Available at http://www.aaoms.org/MediaKit/pdf/terminology.pdf. Accessed December 2005.
Cash AC, Good SA, Curtis RV, McDonald F. An evaluation of slot size in orthodontic brackets-are standards as expected? Angle Orthodon 2004;74(4):450-453. Available at http://www.angle.org/anglonline/?request=get-document&issn=0003-3219&volume=074&issue=04&page=0450. Accessed December 2005.
American Association of Orthodontists. Available at http://www.braces.org. Accessed December 2005.
Lawrence F. Andrews Foundation for Orthodontic Education and Research. History. Available at http://www.andrewsfoundation.org/. Accessed December 2005.
Toledano M, Osorio R, Osorio E, Romeo A, de la Higuera B, García-Godoy F. Bond Strength of Orthodontic Brackets Using Different Light and Self-Curing Cements. Angle Orthodon 2003;73(1):56-63. Available at http://www.angle.org/anglonline/?request=get-document&issn=0003-3219&volume=073&issue=01&page=0056. Accessed December 2005.
http://www.med-college.hu/de/downloads/Andrews_1972_The_six_keys_to_normal_occlusion.pdf
http://www.i-cat.com/products/i-cat-for-orthodontics
http://www.intechopen.com/books/issues-in-contemporary-orthodontics/3d-scanning-imaging-and-printing-in-orthodontics
(1)Flügge TV, Schlager S, Nelson K, Nahles S, Metzger MC. Precision of intraoral digital dental impressions with iTero and extraoral digitization with the iTero and a model scanner. Am J Orthod Dentofacial Orthop 2013;144: 471-8.
https://www.semortho.com/article/S1073-8746(04)00034-9/fulltext
https://www.aaoinfo.org/_online-orothodonic-companies/
https://easyrxcloud.com/news/easyrx-announces-digital-bracket-removal-software/
ABOUT THE AUTHOR
Lori Garland Parker, RDAEF, BS, MAOM
Lori Garland Parker is a clinical consultant and co-founder of Consulting Network, a leading orthodontic management and training organization. She coaches orthodontic practices on maximizing the talents of the clinical team, implementing systems to enhance clinical efficiency and productivity along with continuity of care, and teaches communication skills and patient motivation. She also designed and teaches the "Train the Trainer" program, lectures extensively in the U.S. and abroad, and has written a line of customizable procedure manuals to support successful new employee integration into the practice. Lori holds a Bachelor's in Business and a Master's in Organizational Management. She is also an RDAEF in California.