You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Airborne-particle abrasion is defined in the glossary of prosthodontic terms as "the process of altering the surface of a material through the use of abrasive particles propelled by compressed air or other gasses."1 More casually, this process is known as air abrasion or sandblasting. Most dental laboratories have air-abrasion units that are used to remove investment material, clean out milling residue, roughen the intaglio of crowns, and perform various other procedures associated with laboratory work. The use of intraoral air abrasion has become practical with devices that simultaneously output abrasive particles and water to control the spread of the particles. Several different types of abrasive particles may be used depending on the clinical application for which the intraoral air abrasion is being performed.
This article will describe the armamentarium available for intraoral air abrasion, review the evidence for the use of this modality prior to restorative procedures, and present clinical protocols for employing intraoral air abrasion. Intraoral air abrasion may also be used as a tool for dental prophylaxis, often called air polishing; however, this review will focus on its uses as an adjunct for restorative procedures.
Air-Abrasion Devices
Several commercially available intraoral air-abrasion units can be used without simultaneous water spray. Examples include the MicroEtcher™ IIA (Danville Materials/Zest Dental Solutions, zestdent.com) and the EtchMaster® (Groman Dental, gromandental.com). These systems are effective for roughening and cleaning, although the particle spray tends to be messy for both the patient and the dental operator. If a dental practice is going to make the use of intraoral air abrasion a routine part of restorative procedures, the addition of water spray becomes essential.
Among the intraoral air-abrasion units with water (eg, PrepStart™ H2O, Danville Materials/Zest Dental Solutions; AquaCare, Velopex, velopex.com; RONDOflex™ plus 360, KaVo Kerr, kavo.com; Bioclear Blaster, Bioclear, biocleardental.com), there are differences in the mechanics of the devices that can affect their efficiency in cutting and roughening, such as the mechanism used to mix abrasive particles and air, the air pressure, particle flow rate, and water shrouding flow rate. For example, some devices mix particles and air by creating a vortex within the particle chamber, whereas others use a vibration mechanism.2 Another differentiation is that some intraoral air-abrasion systems are available as standalone devices and others are connected to a dental unit.
After a search of the literature, the authors found no research comparing the effectiveness of air-abrasion particles with and without the use of water. To reiterate, the purpose of the water is to control the spray of the particles.
Standalone Devices
The advantage of a standalone device is that it usually offers more versatility in its functions, such as the ability to adjust the air pressure, particle flow rate, and water shrouding flow rate. Two widely used models, the PrepStart H2O and the AquaCare, contain a reservoir for storage of the air-abrasion particles and fluid and require only a connection from an air line. Both devices contain a foot pedal that is used to activate the air abrasion. The devices differ in that the former unit contains one reservoir, into which the aluminum-oxide, or alumina, abrasive particle of choice may be inserted. The latter device has individual canisters for each type of air-abrasion medium that can be interchanged as needed. As for infection control, these devices have removable handpieces that may be sterilized in an autoclave. The PrepStart H2O utilizes a water reservoir that is filled by the user, so the waterlines must be flushed with a disinfectant solution at the end of each day. The AquaCare device is used with an accompanying fluid component that contains ethanol to sterilize the fluid lines within the device.
Devices Connected to a Dental Unit
Devices that are connected to a dental unit have the benefits of requiring a smaller footprint in the dental operatory and easier mobility between operatories. Examples of these devices include the RONDOflex plus 360 and the Bioclear Blaster. These instruments have canisters that can be filled with the abrasive particles of choice. Water and air from the dental unit are used to run the device. The devices either have removable tips that may be autoclaved or the entire device may be autoclaved.
Abrasive Particles
Several different types of abrasive particles are available for intraoral air abrasion that vary based on their abrasivity. Aluminum oxide (alumina) is the main type of particle used to roughen and "cut" tooth structure. Other, less abrasive particles have been used to clean biofilm or stain from the surface of a tooth prior to bonding.
Aluminum Oxide
Aluminum oxide is a ceramic particle that is the most abrasive particle used intraorally. These particles are irregularly shaped, which means that the rough edges on the particles may be abrasive. The density of alumina is 3.95 g/cm2. The particles can be obtained with an average particle diameter ranging from around 30 µm to 90 µm, with the larger particles (90 µm) being more abrasive.3 These particles are used for the creation of dental preparations, to either cut tooth structure or remove unwanted artifacts within a tooth preparation. Additionally, these particles may be used for roughening dental materials, such as metals,4 ceramics,5 and composite resins.6
Glass
Different forms of glass also have been examined for their capability of removing or roughening tooth structure. Glass bead particles are spherical and have a lower density than aluminum oxide. Typically obtained in particles sizes between 50 µm and 90 µm, glass beads are less abrasive than aluminum oxide on intact dentin and enamel.3 Practically, glass beads are not used for tooth preparation but are indicated for certain cleaning procedures in which surface damage should be minimized, such as removal of cement from temporary restorations or plaque from dentures. Glass bead particles may also be used for cleaning metal instruments.
Bioactive glass also has been investigated for its use as an air-abrasion particle in an effort to take advantage of its antibacterial properties and remineralization potential. It was reported to be less abrasive than aluminum oxide.2 In practice, bioactive glasses may be used as abrasive particles that can occlude dentin tubules to help prevent sensitivity.7
Cleaning Particles
Several types of particles exist purely for cleaning purposes, such as sodium bicarbonate, glycine, calcium sodium phosphosilicate, calcium carbonate, and aluminum trihydroxide.8 A laboratory study determined that air abrasion with each of these particles except for glycine was abrasive enough to alter the surface of resin composite and glass ionomer.9 Moreover, each of the three latter particles-calcium sodium phosphosilicate, calcium carbonate, and aluminum trihydroxide-was capable of altering the surface of enamel.9 Despite this abrasive potential, all of these types of particles are typically less abrasive than alumina abrasive particles.8 Within the realm of restorative dentistry, these particles may all be used for the removal of plaque prior to placement of a dental restoration.
Evidence for Air Abrasion's Effect on Bonding
The effect of air abrasion on the bond to enamel and dentin has been reported previously with mixed results. The results are dependent on the type of adhesive used, whether self-etch or etch-and-rinse.
Previous Studies
Studies regarding shear bond strength after air abrasion on enamel or dentin are contradictory. Some studies had positive results. Mujdeci and Goka reported that air abrasion (25-µm alumina at 120 psi) increased bond strength to enamel and dentin with a total-etch system.10 de Souza-Zaroni et al reported that air abrasion (27.5-µm alumina at 60 psi) increased bond strength to enamel with a self-etch system but had no positive effect on enamel with an etch-and-rinse system.11
On the other hand, other studies have reported that air abrasion reduced bond strength. Nikaido et al found that air abrasion (at 41.8 psi) with 50-µm glass beads significantly decreased the bond strengths to enamel and dentin (etch-and-rinse system), whereas air abrasion with 50-µm alumina decreased adhesion to enamel but did not affect dentin (etch-and-rinse system).12 The scanning electron microscope (SEM) photographs suggested that possible weakened tooth structure after air abrasion could result in adverse bonding strength. Roeder et al reported that when air abrasion (alumina at 120 psi) was used in place of phosphoric etching, a lower bond to enamel and dentin was achieved.13
Furthermore, some studies found there was no difference in bond strength to resin composite on either enamel or dentin after alumina air abrasion. Los and Barkmeier showed no effect on the bond to dentin with a self-etch system after air abrasion at 60 psi with 50-µm alumina or 20-µm to 40-µm hydroxyapatite.14 Similarly, Roeder et al reported that air abrasion (27-µm and 50-µm alumina at 120 psi) did not affect the bond to enamel and dentin with an etch-and-rinse system.13
Laboratory Research
A study was undertaken for this review to examine the effect of air abrasion on the bond to enamel (etch-and-rinse only) and dentin (self-etch and etch-and-rinse). Following Institutional Review Board approval, freshly extracted human teeth were ground to expose flat enamel (n = 20) or dentin (n = 40) and wet-polished to 320-grit silicon paper.
Half of the specimens (n = 10 enamel, n = 20 dentin) were treated with an intraoral air-abrasion unit (PrepStart H2O) for 10 seconds with 50-µm alumina particles (Aluminum Oxide 50 Micron, Danville Materials/Zest Dental Solutions) at 60-psi pressure. The specimens were then rinsed with copious water spray. All of the enamel specimens (n = 20) were etched with 37% phosphoric acid (Scotchbond™ Universal Etchant, 3M Oral Care, 3m.com) for 30 seconds. The dentin specimens were tested in either an etch-and-rinse or self-etch mode. The dentin specimens in the etch-and-rinse group (n = 20) were etched with 37% phosphoric acid for 15 seconds prior to bonding. The dentin specimens in the self-etch group (n = 20) received no etching prior to application of the bonding agent. All specimens etched with phosphoric acid were rinsed for 10 seconds with an air-water spray.
The bonding agent (Prelude One™, Danville Materials/Zest Dental Solutions) was applied to all specimens (both the etch-and-rinse and self-etch groups) following the manufacturer's directions and light-cured using an LED curing light (Elipar™ S10, 3M Oral Care) with output >800 mW/cm2. A cylinder (2.35-mm diameter) of composite (Prestige™, Danville Materials/Zest Dental Solutions) was placed against the tooth surface and cured for 20 seconds from all directions.
Specimens were stored wet at 37ºC for 24 hours and then thermocycled (5ºC and 55ºC, 15-second dwell time, 10,000 cycles). The specimens were subjected to shear-force loading until failure using a universal testing machine (Instron® 5565, Instron, instron.us) at the crosshead speed of 1 mm per minute. Representative specimens were then viewed using SEM.
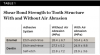
The shear bond strength for each group is presented in Table 1. The effects of air abrasion on shear bond strength for both enamel and dentin were compared separately. A t-test found no difference in bond strength with air abrasion on enamel (P = .437), and a one-way ANOVA found no difference on dentin (P = .515).
The SEMs showed that air abrasion and phosphoric acid applied texture to enamel (Figure 1 through Figure 3) and that when enamel was etched with phosphoric acid after air abrasion, the coarser texture from air abrasion could still be seen through the etch pattern (Figure 4 and Figure 5). This same trend was also observed in dentin (Figure 6 through Figure 10). Despite the increased surface texture (or roughness) created through air abrasion, the results of the shear bond testing indicate that cleaning enamel or dentin with alumina particle air abrasion at a relatively low pressure (60 psi) provides no negative or positive effect on bond strength. Possibly, air abrasion of enamel with a self-etch system would have improved bond strength similar to the study by de Souza-Zaroni et al.11
Clinical Applications
Cavity Preparation
Clinical advantages of performing cavity preparations using intraoral air abrasion instead of a rotary cutting bur include what has been described as a more conservative preparation due to the abrasive particles being able to remove tooth structure in smaller increments than even the smallest burs and the potential to selectively remove only carious or otherwise unwanted tooth structure.15 However, several studies have examined the ability of air abrasion to selectively remove carious dentin while leaving sound dentin and enamel unaffected, and even with varying the types of abrasive particles and air pressure, air abrasion could not selectively remove carious dentin.3,16,17 Additionally, one study determined that air abrasion with alumina was more effective at removing sound tooth structure than carious tooth structure.16
The use of air abrasion to "cut" a preparation takes longer than using a rotary cutting instrument; however, there are various parameters that can affect the cutting efficiency with air abrasion. The air pressure of the device has been shown to linearly increase cutting rate up to 100 psi.18 The recommended air pressure for cutting tooth structure for the air-abrasion unit used in the present study is 100 psi; therefore, the operator should ensure that the air pressure exiting the air line is sufficient to achieve this pressure.
The particle flow rate also can affect cutting efficiency, but it needs to be adjusted based on the air pressure. The abrasive particles require a certain speed in order to cut. If the particle flow rate is increased without sufficient air pressure, the volume of particles will not be sufficiently propelled and the additional particles will only contribute to excess dust.19 Ensuring that a sufficient amount of abrasive particles are in the device's canister prior to and during use is also important, as this will affect the particle flow rate.20
Finally, the angle at which the tip is held relative to the surface being abraded and the distance of the tip from the surface being abraded both will affect cutting efficiency. Holding the nozzle at 60 degrees to the surface being abraded will allow efficient v-shaped cutting, and maintaining a 5-mm distance from the nozzle to the enamel surface has been shown to produce the most efficient cutting.18
Another benefit of intraoral air abrasion is patient comfort. A clinical trial compared the preparation of fissure caries (at the depth of the dentinoenamel junction) in premolars of the same patient with air abrasion and a rotary cutting handpiece. No anesthesia was used. The patients reported a significantly lower perception of pain with air abrasion, and all patients preferred the treatment with air abrasion.19
Preparation Cleaning
Air abrasion with alumina also can be used as an adjunctive procedure for cleaning tooth preparations prior to bonding. As mentioned previously, the results of testing the effects of air abrasion on dentin and enamel prior to bonding are varied.10-14 Additionally, air abrasion for selective caries removal seems to be ineffective. 3,16,17
With these limitations acknowledged, visual inspection of tooth preparations after air abrasion reveals that this modality is effective in removing remnant restorative materials, stains, and temporary cement, leaving a clean, matte surface for bonding (Figure 11 through Figure 14). Air abrasion also can smooth the internal aspects of a cavity preparation to help enable better adaptation of the restorative material (Figure 15 and Figure 16). The technique-sensitive nature of adhesive bonding may justify this extra procedure to ensure a clean, smooth preparation.
Biofilm Removal
Air abrasion with aluminum trihydroxide has been used as an adjunctive for tooth preparation to remove plaque, light calculus, undermined enamel, poorly bonded resins or liners, and soft-tissue tags prior to bonding. The rationale of biofilm removal before bonding is to remove any impediments to effective etching of enamel that may lead to reduced bond strength and microgaps that could contribute to future stain and leakage. Because biofilm can be difficult to visualize, a one-time application of a two-tone disclosing solution to dried teeth may help reveal biofilm and provide a visual cue for effective removal (Figure 17 through Figure 19). Some cleaning particles other than glycine or sodium bicarbonate can alter the enamel surface; therefore, reapplication of disclosing solution should be avoided as this may lead to risk of undesired staining of tooth structure.
Summary
Air abrasion can be a means of cavity preparation or an adjunctive procedure for tooth preparation with adhesive dental restorations. Although the evidence for air abrasion as a method to improve the retention to dentin and enamel is mixed, air abrasion can be visually confirmed to clean and smooth preparations prior to bonding, without anesthesia in some cases. When using air abrasion for restorative dentistry, the abrasive particles and device parameters should be optimized for the procedure at hand.
About the Authors
Chan-Te Huang, DDS
Chief Resident, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama; Attending Faculty, Chang Gung Memorial Hospital, Keelung, Taiwan
Jihyon Kim, DDS
Private Practice, Bellevue, Washington
Celin Arce, DDS, MS
Assistant Professor, University of Alabama at Birmingham School of Dentistry, Birmingham Alabama
Nathaniel C. Lawson, DMD, PhD
Assistant Professor, University of Alabama at Birmingham School of Dentistry, Birmingham, Alabama
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. The glossary of prosthodontic terms: ninth edition. J Prosthet Dent. 2017;117(5S):e1-e105.
2. Milly H, Austin RS, Thompson I, Banerjee A. In vitro effect of air-abrasion operating parameters on dynamic cutting characteristics of alumina and bio-active glass powders. Oper Dent. 2014;39(1):81-89.
3. Horiguchi S, Yamada T, Inokoshi S, Tagami J. Selective caries removal with air abrasion. Oper Dent. 1998;23(5):236-243.
4. Kern M, Thompson VP. Sandblasting and silica-coating of dental alloys: volume loss, morphology and changes in the surface composition. Dent Mater. 1993;9(3):151-161.
5. Inokoshi M, De Munck J, Minakuchi S, Van Meerbeek B. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res. 2014;93(4):
329-334.
6. Spitznagel FA, Horvath SD, Guess PC, Blatz MB. Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J Esthet Restor Dent. 2014;26(6):382-393.
7. Sauro S, Watson TF, Thompson I. Dentine desensitization induced by prophylactic and air-polishing procedures: an in vitro dentine permeability and confocal microscopy study. J Dent. 2010;38(5):411-422.
8. Graumann SJ, Sensat ML, Stoltenberg JL. Air polishing: a review of current literature. J Dent Hyg. 2013;87(4):173-180.
9. Barnes CM, Covey D, Watanabe H, et al. An in vitro comparison of the effects of various air polishing powders on enamel and selected esthetic restorative materials. J Clin Dent. 2014;25(4):76-87.
10. Mujdeci A, Gokay O. The effect of airborne-particle abrasion on the shear bond strength of four restorative materials to enamel and dentin. J Prosthet Dent. 2004;92(3):245-249.
11. de Souza-Zaroni WC, Delfino CS, Ciccone-Nogueira JC, et al. Effect of cavity preparation method on microtensile bond strength of a self-etching primer vs phosphoric acid etchant to enamel. J Mater Sci Mater Med. 2007;18(10):2003-2009.
12. Nikaido T, Kataumi M, Burrow MF, et al. Bond strengths of resin to enamel and dentin treated with low-pressure air abrasion. Oper Dent. 1996;21(5):218-224.
13. Roeder LB, Berry EA 3rd, You C, Powers JM. Bond strength of composite to air-abraded enamel and dentin. Oper Dent. 1995;20(5):186-190.
14. Los SA, Barkmeier WW. Effects of dentin air abrasion with aluminum oxide and hydroxyapatite on adhesive bond strength. Oper Dent. 1994;19(5):169-175.
15. Malterud MI. Air abrasion: the new renaissance with an H2O twist. Dent Today. 2010;29(10):146-149.
16. Paolinelis G, Watson TF, Banerjee A. Microhardness as a predictor of sound and carious dentine removal using alumina air abrasion. Caries Res. 2006;40(4):292-295.
17. Motisuki C, Lima LM, Bronzi ES, et al. The effectiveness of alumina powder on carious dentin removal. Oper Dent. 2006;31(3):371-376.
18. Paolinelis G, Banerjee A, Watson TF. An in-vitro investigation of the effects of variable operating parameters on alumina air-abrasion cutting characteristics. Oper Dent. 2009;34(1):87-92.
19. Malmström HS, Chaves Y, Moss ME. Patient preference: conventional rotary handpieces or air abrasion for cavity preparation. Oper Dent. 2003;28(6):667-671.
20. Banerjee A, Uddin M, Paolinelis G, Watson TF. An investigation of the effect of powder reservoir volume on the consistency of alumina powder flow rates in dental air-abrasion devices. J Dent. 2008;36(3):224-227.