You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Many factors contribute to the long-term crestal bone changes observed around endosseous dental implants. Ketabi et al published a four-part series based on an extensive literature search of articles published up to 2008 in which they presented several factors and their interactions that the authors identified as contributing to crestal bone changes.1-4 These factors were categorized as: surgical and anatomical, patient, biological width, geometry and surfaces, and biomechanical. The four-part series is recommended reading for anyone treating patients with dental implant therapy.
Clinicians can mitigate many of the issues identified above by starting treatment with a solid foundation. This article will examine how implant connection type and location, prosthetic material choice, and component handling all play important roles in establishing and maintaining the necessary soft-tissue seal around the implants and abutments.
Key Factors
Soft-tissue seal-Similar to a natural tooth, the soft-tissue complex around a dental implant consists of sulcular and junctional epithelium and connective tissue, forming a biological width approximately 3 mm in height.5 However, unlike a natural tooth there are no connective tissue fibers imbedding into the dental implant; rather, the connective tissue forms circular bands around the implant. The epithelial cells form a very fragile hemidesmisonal seal to the tissue-compatible implant or abutment surface. Though quite fragile, this seal is critical to prevent bacterial invasion and must always be present.
Implant connection types-Many implant types with different abutment connections have been developed over the years. The predominantly used styles are bone-level implants and one-stage tissue-level implants. Both of these kinds of implants have abutment connections that fall into two categories: buttress connection, which can be external hex or an internal connection in various shapes; and locking-taper conical connection.
Bone-level buttress joint implants-Ericsson et al examined inflammatory reactions in peri-implant soft tissues in a canine model utilizing external hex machined titanium fixtures.6 Their histological analysis of the soft tissues showed there was consistently an inflammatory cell infiltrate at the implant-to-abutment junction, which they labeled the abutment ITC. They found the bone was consistently 1 mm to 1.5 mm below the junction and that approximately 1 mm of normal non-infiltrated connective tissue separated the abutment ITC and bone. They hypothesized that this may explain the bone loss observed around these types of implants during the first year after bridge connection.
This type of response has been observed on bone-level external hex implants for decades and is extensively documented in prospective clinical studies.7-10 This ITC response is not unique to external hex implants, but rather may be observed on all buttress joint type connections placed at bone level, whether the connection is an external hex or some form of internal connection.11 This type of buttress connection has been characterized as having a microgap, which contributes to the ITC observed by Ericsson et al.6
Platform switching was introduced to bone-level implants in an attempt to move the abutment connection and, hence, the microgap away from the outer edge of the implant. These connections have shown some success with the reduction in marginal bone loss being proportional to the size of the platform switch.11,12
Dealing With the Microgap
Two types of dental implants that avoid the ITC response at the implant-to-abutment junction are one-stage implants and locking-taper conical connection implants. With one-stage implants, the implant-to-abutment connection is placed in or above the sulcular epithelium. This allows the junctional epithelium and connective tissue to form the protective seal on the smooth collar of the implant and remain undisturbed during the healing and restorative phases of treatment.
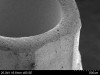
Locking-taper conical connection implants are carefully designed with exacting tolerances to achieve a precise abutment-to-implant interface. The advantages of this type of connection are its strength and sealing properties. Figure 1 and Figure 2 show a cross section of one locking-taper conical connection implant-to-abutment connection at 10X and 1000X magnification, respectively, demonstrating the precise fit. This type of locking taper effectively eliminates the microgap found on buttress joint connections and allows the possibility of achieving a permanent soft-tissue seal on the transmucosal abutment surface.
Care must be taken to preserve the integrity of the fit of the abutment into the locking-taper conical connection. The author has spent considerable time trouble-shooting complaints from clinicians, primarily for screw-loosening issues. His examination of returned abutments with light microscopes and scanning electron microscopes (SEMs) typically reveals a very rough texture on the abutment-engaging surface, which is a result of mishandling by the dental laboratory (Figure 3 and Figure 4).
It is the author's belief that most restorative doctors neglect to inspect abutments with magnification when they receive them from the dental laboratory. The author has polled more than 4,000 clinicians and staff over the past 3 years during lectures as to whether they, in fact, inspect abutments from the dental laboratory with magnification. Very few have responded in the affirmative. Therefore, they cannot be certain of the quality of the product they are receiving. The abutment shown in Figure 3 and Figure 4 no longer has the tight seal mandatory for the soft-tissue performance of this type of connection and is likely to also experience screw-loosening issues.
The author recommends that clinicians inspect the abutments and frameworks they receive from dental laboratories with at least 10X magnification. Use of a 10X loupe, which can be purchased for around $10, is recommended. The abutment interface must be closely inspected and be in flawless condition, with every machine line visible (Figure 5). Abutments received in an imperfect state should be returned to the dental laboratory.
Component Handling
Rompen et al conducted a soft-tissue healing study in patients using clean and sterile titanium healing abutments placed onto external hex implants. Healing abutments were placed on the implants (at second-stage surgery) and the soft tissues were allowed to heal for 12 weeks. The healing abutments were removed and subsequent analysis of the surfaces with a SEM showed epithelial tissues well adhered to the titanium surface. As a comparison, the authors handled a subset of abutments with their bare fingers during placement onto the implants. Subsequent SEM analysis of these abutments revealed no epithelial cells adhered to the titanium surface. Thus, they demonstrated that it is imperative the components placed onto bone-level dental implants be perfectly clean and sterile to achieve epithelial adhesion.13
When the healing abutments are removed at the time of impression taking, redness and bleeding are often observed in the soft tissue. This may often be misinterpreted as inflammation of the gingival tissue. In fact, it is capillary bleeding that is the result of the epithelial cells being torn apart upon abutment removal. Rompen recommends the healing abutments be placed in sterile saline solution while the impressions are being taken so the epithelial cells have the opportunity to reattach when the healing abutments are replaced.13
The goal with regard to the soft tissue is to establish a good epithelial seal on the healing abutment or temporary abutment as Rompen demonstrated, causing as little tissue disruption as possible during the impression phase and re-establishing the tissue seal on the final abutment. Abrahamsson et al showed in a canine model that if the abutments are removed repeatedly the soft tissue recedes and marginal bone loss occurs.14 Therefore, minimal disruption of this seal is critical. Ideally, it is desirable to place the abutments only one time and never remove them. Placing multi-unit or single-tooth transmucosal abutments in a one-stage procedure or at second-stage uncovering is considered the gold standard for establishing the soft-tissue seal.
When the final abutments are placed onto the implants they must be clean and sterile as well. As stated earlier, the author has presented this information in lecture form to more than 4,000 clinicians and staff over the past several years. During these lectures, attendees were polled as to whether they wash and sterilize the final abutments they receive from dental laboratories before placing them onto the dental implant in the patient. Consistently, only 1% to 2% of the respondents answered in the affirmative. This means that restorative dentists are routinely placing contaminated final abutments onto implants, which Rompen showed is detrimental to achieving the desired soft-tissue adhesion.13 According to the author's polling, restorative dentists respond that they are not being taught this in dental school.
Best practice for the dental office to maximize the probability of achieving a soft-tissue seal on the final abutment is to scrub it with soap and water and a toothbrush and rinse clean. The abutment should then be placed in a sterilization pouch and autoclaved. While dipping abutments into chlorhexidine or flushing the implant gingival socket with chlorhexidine are perceived as antibacterial treatments, two different clinical studies have shown that chlorhexidine can have serious toxic effects on gingival fibroblasts and may negatively affect healing.15,16
Tissue-Compatible Materials
In 1998 Abrahamsson and colleagues presented results of a canine study that examined soft-tissue response to different materials placed as healing abutments on external hex implants.17 They found that titanium and aluminum-oxide abutments allowed the formation of a mucosal attachment consisting of junctional epithelium and connective tissue. However, at sites where gold alloy and porcelain abutments were placed on the implants no mucosal attachment was observed and the soft-tissue margin receded and bone resorption occurred.
In 2008 Welander et al found stable tissue around titanium and zirconia abutments and an apical shift of the tissue with gold alloy abutments placed into locking-taper conical connection implants.18
In a prospective 4-year study Vigolo et al compared the soft and hard tissues around gold abutments and titanium abutments on external hex implants.19 They concluded the soft- and hard-tissue response to the materials was the same; however, the mean bone loss for both groups was 0.4 mm below the bottom of the implant collar, basically to the first thread as commonly seen on this type of implant. No conclusion of tissue compatibility of gold alloy can be drawn from this study.
Polyetheretherketone (PEEK) polymer is widely used as a material for both temporary and healing abutments, and these are sold by many dental implant manufacturers. However, no studies demonstrate the tissue compatibility as discussed above. Schupbach and Rompen have each independently examined PEEK healing abutments removed from patients utilizing SEM, and each showed similar results. Figure 6 and Figure 7 (provided by Dr. Schupbach) show the junctional epithelium adhered to a retrieved PEEK healing abutment. These are the only two such investigations to date, and both are very small; there are no published studies to reference. However, though data is admittedly limited and more investigation of this material is needed, it appears PEEK also supports soft-tissue adhesion.
Materials that do and do not support soft-tissue adhesion are listed in Table 1. Only the tissue-compatible materials shown should be used as an abutment material for locking-taper conical connection implants. Use of non-compatible materials will result in the formation of a pocket around the abutment. Apical bone migration is likely to occur as the body strives to form the soft-tissue seal on the surface of the dental implant.
Any of the materials listed in Table 1 may be used directly on top of one-stage implants and on top of transmucosal abutments. As noted earlier, the soft-tissue adhesion forms to the smooth collar of these implants and abutments, and these restorative materials are placed in or above the sulcular epithelium, where they do not disrupt the soft-tissue seal.
Engaging Vs Non-Engaging Abutments
As mentioned previously, the advantage of the locking-taper conical connection implant design is the tight seal formed between the implant and abutment. This is commonly used with single-tooth restorations. When placing a prosthesis on multiple implants, multi-unit transmucosal abutments must first be placed into the locking-taper conical connection implants to seal the implant-to-abutment junction as well. Several types of locking-taper conical connection implants have a provision on the top surface of the implant to allow a non-engaging prosthesis to be directly affixed to the implant (Figure 8). This kind of prosthesis is appealing to restorative dentists because of the simplicity of using a single, larger screw and the relatively lower cost of componentry. However, due to the likelihood of formation of an ITC at the implant-to-prosthesis junction and subsequent anticipated marginal bone loss, this technique should be avoided. When a non-engaging implant-level prosthesis is the desired restorative solution on multiple implants, one-stage tissue-level implants are a more suitable solution.
Applications
Locking-taper conical connection implants have demonstrated very good bone-level maintenance20,21 and are the optimal choice for use in the esthetic region. One-stage implants in esthetic applications may show grey through thin tissue and can be difficult to work with if the soft tissue recedes and exposes the implant collar. In posterior applications where the size of the restoration typically is much larger than the small size of the conical connection, a one-stage implant, which has a larger connection size, may be preferred.
In applications such as bar overdentures, either locking-taper conical connection implants or one-stage implants may be used according to clinician preference. When locking-taper conical connection implants are chosen, multi-unit transmucosal abutments must be used to obtain the seal to the implant. One-stage implants are placed with the smooth collar in the soft tissue, and frameworks may be affixed directly to the implant. This saves considerable cost in componentry.
Conclusion
A main objective of implant treatment is to establish and maintain a soft-tissue seal. The key factors are implant connection type, connection location, proven biocompatible materials, and, of course, adequate attached keratinized tissue surrounding the implants and abutments. With locking-taper conical connection implants the seal can be obtained on the transmucosal abutment, while with one-stage implants the seal is obtained on the smooth collar of the implant.
Only titanium or zirconia materials should be used for final abutments with locking-taper conical connection implants. PEEK abutments may also be used for temporary restorations. The restorative dentist must inspect, wash, and sterilize the abutments prior to placing them on the implants. Lastly, gold and porcelain restorative materials may be used on top of transmucosal abutments or directly on top of one-stage implants.
About the Author
Steve Hurson
Chief Scientist (Retired), Nobel Biocare
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Katabi M, Pilliar R, Deporter D. Factors driving peri-implant crestal bone loss - literature review and discussion: part 1 of 4. JIACD. 2009;1(2):19-28.
2. Katabi M, Pilliar R, Deporter D. Factors driving peri-implant crestal bone loss - literature review and discussion: part 2 of 4. JIACD. 2009;1(3):63-71.
3. Katabi M, Pilliar R, Deporter D. Factors driving peri-implant crestal bone loss - literature review and discussion: part 3 of 4. JIACD. 2009;1(9):65-71.
4. Katabi M, Pilliar R, Deporter D. Factors driving peri-implant crestal bone loss - literature review and discussion: part 4 of 4. JIACD. 2010;2(2):83-88.
5. Berglundh T, Lindhe J, Ericsson I, et al. The soft tissue barrier at implants and teeth. Clin Oral Implants Res. 1991;2(2):81-90.
6. Ericsson I, Persson LG, Berglundh T, et al. Different types of inflammatory reactions in peri-implant soft tissues. J Clin Periodontol. 1995;22(3):255-261.
7. Lekholm U, Adell R, Lindhe J, et al. Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg. 1986;15(1):53-61.
8. Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1(1):11-25.
9. Apse P, Zarb GA, Schmitt A, Lewis DW. The longitudinal effectiveness of osseointegrated dental implants. The Toronto Study: peri-implant mucosal response. Int J Periodontics Restorative Dent. 1991;11(2):94-111.
10. Leonhardt A, Gröndahl K, Bergström C, Lekholm U. Long-term follow-up of osseointegrated titanium implants using clinical, radiographic and microbiological parameters. Clin Oral Implants Res. 2002;13(2):127-132.
11. Canullo L, Fedele GR, Iannello G, Jepsen S. Platform switching and marginal bone-level alterations: the results of a randomized-controlled trial. Clin Oral Impl Res. 2010;21(1):115-121.
12. Trammell K, Geurs N, O'Neal S, et al. A prospective, randomized, controlled comparison of platform-switched and matched-abutments implants in short span partial denture situations. Int J Periodontics Restorative Dent. 2009;29(6):598-605.
13. Rompen E. How to optimize transmucosal health and maintain tissues in the posterior region. Paper presented at: Europerio Conference, June 2015; London.
14. Abrahamsson I, Berglundh T, Lindhe J. The mucosal barrier following abutment dis/reconnection. An experimental study in dogs. J Clin Periodontol. 1997;24(8):568-572.
15. Wyganowska-Swiatkowska M, Kotwicka M, Urbaniak P, et al. Clinical implications of the growth-suppressive effects of chlorhexidine at low and high concentrations on human gingival fibroblasts and changes in morphology. Int J Mol Med. 2016;37(6):1594-1600.
16. Marioth AJ, Rumpf DA. Chlorhexidine-induced changes to human gingival fibroblast collagen and non-collagen protein production. J Periodontol. 1999;70(12):1443-1448.
17. Abrahamsson I, Berglundh T, Glantz PO, Linde J. The mucosal attachment at different abutments. An experimental study in dogs. J Clin Periodontol. 1998;25(9):721-727.
18. Welander M, Abrahamsson I, Berglundh T. The mucosal barrier at implant abutments of different materials. Clin Oral Implants Res. 2008;19(7):635-641.
19. Vigolo P, Givani A, Majzoub Z, Cordioli G. A 4-year prospective study to assess peri-implant hard and soft tissues adjacent to titanium versus gold-alloy abutments in cemented single implant crowns. J Prosthodont. 2006;15(4):250-256.
20. Kolinski M, Cherry J, McAllister B, et al. Evaluation of a variable-thread tapered implant in extraction sites with immediate temporization: a 3-year multicenter clinical study. J Periodontol. 2014;85(3):386-394.
21. Laurell L, Lundgren D. Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Relat Res. 2011;13(1):19-28.