You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Current estimates of obstructive sleep apnea (OSA) cases in the United States (U.S.) adult population range between 4% to 9%, however between 70% to 90% of adults remain undiagnosed.1-2 Repetitive episodes of total or partial collapse of the upper airway during sleep characterizes OSA leading to sleep disruption and decreased oxygen levels or hypoxia.3 Inflammation, oxidative stress and increased sympathetic activity precipitated by the sleep fragmentation and hypoxia are some of the mechanisms that link OSA to several medical comorbidities affecting patients' oral and systemic health.4 A strong association exists between OSA and cardiovascular diseases including hypertension, heart failure, arrhythmias, and stroke.5,6 Some studies also implicate a potential association between OSA and periodontal disease.5,7 Inflammatory cytokines such as TNF-α, IL-1β and acute phase C-reactive protein are increased in OSA patients8,9 and in patients with periodontitis.10,11
Several anatomical risk factors are associated with OSA including a large neck circumference, small size and a retruded position of the mandible (retrognathia), enlarged tongue, tonsillar hypertrophy, class II malocclusion and extension of the soft palate behind the tongue.3 Snoring, general fatigue, and excessive daytime sleepiness (EDS) are common symptoms of OSA. Because symptoms such as fatigue and EDS are also common to other chronic diseases, OSA is often not diagnosed as readily as its comorbidities such as diabetes or cardiovascular diseases.3 Obesity is a major risk factor for OSA. It often leads to enlargement of the soft tissue in the upper airway and the tongue.12,13 Ideal screening includes identifying the anatomical risk factors, clinical symptoms that patients experience and implementing validated screening tools followed by appropriate referral to a physician for further evaluation.4
Currently, there are several validated OSA screening tools available for health professionals such as the Epworth Sleepiness Scale, Berlin Questionnaire, and STOP Questionnaire.14-16 Each evaluates a different aspect or risk factor of OSA. Perhaps the most widely used tool is the STOP-BANG questionnaire, which takes into account the patient's medical conditions and symptoms.15 Mallampati scoring of oropharynx (length of soft palate) is an important part of assessment of the potential for soft tissue obstruction during intraoral examination which has been shown to predict both the presence and severity of OSA.17 Patients at risk for OSA are usually referred by their primary care providers although some otolaryngologists, cardiologists and neurologists specialize in sleep medicine. A definitive diagnosis is obtained by conducting polysomnography (i.e., sleep study) in consultation with a sleep medicine physician.8
Continuous positive airway pressure (CPAP) is the most effective treatment for moderate to severe OSA. The CPAP machine provides a continuous stream of air under high pressure that prevents the upper airway from collapsing.3 The American Academy of Sleep Medicine recommends oral appliances (OA) for patients who are intolerant of CPAP (25% to 58%) or for those who prefer an alternate treatment option.18 The OA advances the tongue and the mandible forward, increasing the upper airway diameter and reducing the upper airway collapse.19-21
Dental professionals have the potential to recognize the signs and symptoms of sleep apnea and refer patients for a medical consultation.4 Dental hygienists spend the most time with patients and have the potential to provide an appropriate setting to conduct OSA screenings. While the potential for this practice has been previously proposed,4 no published studies have reported the level of knowledge and attitudes about the importance of identifying OSA among dental hygienists. Practice modifications adopted by busy clinicians require both a positive attitude toward the need, and adequate knowledge base in the subject matter to implement and sustain a change.22 The primary aim of this study was to assess the current OSA knowledge and attitudes of Minnesota dental hygienists and to identify the screening tools currently used to identify patients at high risk of OSA in dental practices. In addition, the study results can inform the need for continuing education on OSA, dental hygiene program curriculum changes, and implementing OSA screening protocols into dental hygiene clinical practice.
Methods
The study population consisted of a simple random sample of the 5,625 licensed dental hygienists in the state of Minnesota; those who were no longer in clinical practice or who obtained licensure within the last year were excluded from the study. An initial sample size of 750 participants was based on an average of an approximate 50% response rate, a sample size used in recent survey studies with dental hygienists and budgetary restrictions.23-25 However, since this was a descriptive study, no minimum sample was required to meet statistical test criteria.
Data collection instrument
The Obstructive Sleep Apnea Knowledge and Attitude (OSAKA) questionnaire had been developed to measure OSA knowledge and attitudes among physicians; the instrument was modified for use in this study.26 Following permission from the OSAKA designer, the items were adapted for administration to dental hygienists with minimal changes reflecting clinical practice settings (e.g., "cardiology" was changed to "dental hygiene"). The final version of the 40 item survey included 18 OSA knowledge items divided into four subcategories described as prevalence, diagnosis, risk factors, and treatment.26 Response choices were true (scored as 1 point), and false or don't know (scored as 0 points) with a total possible score of 18 points. Five attitudinal items were subcategorized into two areas: importance of OSA as a disorder, and confidence in identifying and managing OSA patients.
Responses were selected from a 5-point Likert scale ranging from "not important or confident" to "extremely important or confident." Self-assessed knowledge of OSA consisted of one question ranked on a scale of 0 (no knowledge) to 10 (very knowledgeable). Additional questions assessed OSA curricular content in dental hygiene undergraduate programs, and completion of post-graduate OSA continuing education courses. Routine clinical screening practices assessed were the inclusion of an OSA item on medical history forms, performing extra- and intraoral examinations, and checking blood pressures (BP). An inventory of one or more currently used OSA protocols included the Mallampati Classification27, Berlin questionnaire14, STOP questionnaire, STOP- BANG questionnaire15, and the Epworth Sleepiness Scale.16 Demographic variables included age, practice setting (general or specialty), and undergraduate degree type (bachelor or associate).
Content validity of the modified survey was evaluated by OSA experts associated with the University of Minnesota School of Dentistry and recommended changes were incorporated into a second version. The survey was then piloted among ten dental hygienists who met the inclusion criteria for study participation. Further changes were reviewed by the study team and incorporated into the final survey.
Procedures
The paper survey was mailed to 750 randomly selected dental hygienists and included a cover letter and stamped addressed return envelope. Subjects were asked to return the survey within two weeks of receipt. Each mailing list name and address was numbered with a corresponding code indicated on the survey allowing for a targeted second mailing to non-respondents two weeks after the initial mailing. The study was submitted to the University of Minnesota Institutional Review Board and deemed exempt.
Data analysis
Descriptive statistics including means and standard deviations for continuous measures; counts and percentages for categorical measures, were used to summarize item responses (SAS V9.3; SAS Institute Inc., Cary, NC). Internal consistency of the modified survey instrument attitude items was calculated to determine Cronbach's alpha. Pearson's correlation was used to test the correlation between self-assessed knowledge and total knowledge scores. Total knowledge scores and attitude scores were treated as dependent variables with one-way ANOVA for age categories, t-tests for degree type, and Pearson's correlation coefficient to determine an association with years in practice. The alpha level for all statistical tests was established at 0.05.
Results
Surveys were completed and returned by 230 respondents (n=230) included in the initial mailing of 750 (n=750) dental hygienists. Thirty-three surveys were excluded from analysis because respondents did not meet study inclusion criteria (i.e., they were no longer in clinical practice). The final sample consisted of 197 surveys (n=197) or 26% of the sample.
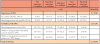
Respondents ranged in age from 19 to 70 years. Mean (SD) years in practice was 19.9 (12.0) and 93.9% practiced primarily in a general dentistry setting. The mean (SD) weekly hours practiced was 29.7 (8.3), and the majority of subjects (59.6%) earned an associate level degree upon completion of their dental hygiene program. Because a substantial number of respondents did not indicate their degree type (8.3%), results were reported with an additional category titled "non-specified." This variable was not included in additional analyses. Respondents' mean (SD) self-rated level of OSA knowledge was 3.5 (3.3) out of 5. Respondents' total knowledge mean score was 9.5 out of 18; itemized results are reported in Table I. Applying Pearson's product-moment coefficient of correlation, a moderate and statistically significant correlation (r=0.46, p<0.001) was found between the respondents' perceived self-assessed knowledge and their total knowledge scores.
Response frequencies to the five OSA attitudinal questions are shown in Table II. Subcategory mean scores (SD) for the "importance of OSA" was 3.7 (0.8) out of 5 and "confidence of identifying OSA risk factors" was slightly lower at 2.8 (1.0) out of 5. The mean (SD) for all items was 3.2 (0.8).
Because the instrument used to collect data was altered for use in this study, both the internal validity and correlation between items was tested replicating the same procedures conducted by Schotland et al26 as part of initial survey development. Cronbach's alpha was established at 0.81 indicating a good level of internal consistency. Correlations between each item ranged from none to high, with several results yielding statistically significant associations (Table III).
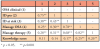
Results of the inferential statistical analyses comparing the dependent variables of total knowledge scores and attitude to age, degree type and years in practice are displayed in Table IV. No statistically significant differences were found.
The majority of respondents reported that they routinely conducted extra- and intraoral examinations (89.3%), but fewer than half (41.6%) regularly checked patients' blood pressure. Less than half reported inclusion of an OSA item on their practice's medical history form (39.6%). Only ten (9.6%) of the respondents used an established OSA screening tool with half reporting use of the STOP-BANG tool, either exclusively or in addition to, another method.
Discussion
Previous studies have established the potential for dental hygienists to screen patients for OSA risk factors in clinical practice settings. However, there is a gap in the literature regarding the actual OSA knowledge, attitudes and screening practices of dental hygienists. As no dental hygiene comparatives were available, results of physicians completing the OSAKA knowledge and attitudes items were reviewed. Comparisons of studies assessing the OSA knowledge of cardiologists, internists and family practitioners showed that these health care providers consistently scored higher than dental hygienists (76%, 79% and 78%, respectively, vs. 54%).26,28 Mixed comparisons were found between this study and others when comparing OSA knowledge with clinician age, practice type or specialty, and years in practice. This study, similar to a report of cardiologists, found no differences in OSA knowledge or attitudes by age, years in practice or practice type. However, Schotland et al26 found a statistically significant inverse relationship among internists and family practitioners by age; lower knowledge scores and less confidence in diagnosing OSA were associated with increased age. These differences may be due to practice specialization with cardiologists and dental hygienists being less likely to routinely screen for OSA as compared to primary care family practitioners and internists.
Attitudinal comparisons found that fewer dental hygienists than cardiologists reported OSA as either a "very important" or "extremely important" clinical disorder (59% vs. 78%, respectively).28 Fewer than one-fourth (24% of dental hygienists), compared to over two-thirds (68% of physicians), were confident in their ability to identify patients with OSA.28 Twenty-four percent of dental hygienists compared to 18% of cardiologists were "very confident" or "extremely confident" in their ability to manage (dental or general) concerns of OSA patients. Twenty-seven percent of dental hygienists were "very confident" or "extremely confident" in their ability to manage dental concerns related to OSA on CPAP therapy compared to 10% of cardiologists' general ability to manage these patients.
It should be noted that the last two attitudinal survey questions for dental hygienists specific to patient management and CPAP therapy were modified to indicate dental concerns as opposed to general patient management in the original OSAKA survey for physicians. Results of correlation analyses between attitudes toward OSA and knowledge scores were similar for both dental hygienists (r=0.23; p=0.001) and cardiologists (r=0.29; p=0.004).28 It is of interest that both clinician groups with attitudes identifying OSA as important also had higher OSA knowledge scores.
Fewer than half of all respondents routinely collect clinical information critical to diagnosing OSA. Approximately one-third of dental hygienists reported that the medical history forms used in their practices include questions specific to OSA or its symptoms. Furthermore, only 41.6% responded that blood pressure screenings were performed during routine dental hygiene care appointments. This result was surprising as clinical practice guidelines recommend blood pressure screenings at all dental hygiene care appointments.29 It is well established that many OSA patients also exhibit high blood pressure,30-34 and current evidence suggests improved blood pressures with OSA treatment.34
A majority of respondents (89.3%) indicated that they completed or assisted in examinations that evaluate extra- and intraoral structures during routine dental hygiene appointments. While the current emphasis of this procedure is on oropharyngeal cancer detection, educating dental hygienists on anatomical variations indicative of OSA could seamlessly include a practical addition to this routine assessment.
The use of established OSA screening protocols or other tools used in dental practices was very low in this study population (9.6%). The small number of respondents (n=10) makes it difficult to determine the utility of available instruments, and further inquiry is needed to determine an appropriate tool for use in the dental setting.
Study limitations include a low response rate despite two mailings including prepaid envelopes. Contributing factors may include lack of an incentive to complete the survey, limited familiarity or interest in the subject matter, or lack of time. Therefore, results may not be representative of dental hygienists as a whole. However, the significance of this study is that the dental hygienist respondents consider OSA to be an important disorder; although their confidence in identifying and managing dental concerns of OSA patients is lower than attitudes regarding its importance. Further, dental hygienists' perception of their OSA knowledge coincides with their actual OSA knowledge. As it is well established that attitudes preclude the acquisition of knowledge and subsequent behavioral change,22 results from this study support increasing educational opportunities on OSA for dental hygiene students and practicing clinicians.
A majority of the 70 to 90% of Americans with OSA remain undiagnosed indicating the need for new screening and referral strategies.4 As the health care paradigm shifts towards interprofessional practice, the potential role of dental hygienists to screen for OSA is timely. Standardized OSA screening can be integrated seamlessly into clinical practice as dental hygienists often conduct routine medical history reviews, head and neck examinations, intraoral examinations and blood pressure screenings. The time spent to administer a brief questionnaire, elicit a conversation regarding OSA symptoms, and provide a dentist's referral for assessment by a physician is reasonable, especially when considering the potential benefits to patients. Dental hygienists are likely to have more time for the initial screening of patients with the dentist confirming positive responses. Preparing clinicians will require incorporating OSA into dental hygiene curricula and offering continuing education courses for practicing professionals. The long-term goal of this line of research is to improve the recognition of OSA signs and symptoms along with referrals to physicians for further evaluation and management.
Conclusion
The attitudes of Minnesota dental hygienists regarding the importance of OSA as a chronic disorder are higher than their knowledge of OSA. Currently, dental hygienists are underutilized for performing OSA screening in the dental practice setting. Results from this study support the practical aspects of incorporating OSA into the knowledge base of dental hygiene practice to improve the screening and referral of patients presenting with OSA symptoms.
About the Authors
Yvette G. Reibel, MSDH, is an assistant clinical professor in the Division of Dental Hygiene, Department of Primary Dental Care, University of Minnesota School of Dentistry; Snigdha Pusalavidyasagar MD, FAASM, is an assistant professor of medicine, Division of Pulmonary, Critical Care, Allergy and Sleep Medicine, University of Minnesota Medical School; Priscilla M. Flynn, RDH, DrPH is an associate professor in the Division of Dental Hygiene, Department of Primary Dental Care, University of Minnesota School of Dentistry; all at the University of Minnesota, Minneapolis, MN.
Yvette Reibel, MSDH was the 2018 winner of the graduate ADHA/Sigma Phi Alpha Journalism Award sponsored by Johnson & Johnson Consumer Inc.
Corresponding author: Yvette G. Reibel, RDH, MSDH; wlod0003@umn.edu
References
1. Finkel KJ, Searleman AC, Tymkew H, et al. Prevalance of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009 Aug; 10(7):753-8.
2. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 1997 Sep; 20(9):705-6.
3. An S, Ranson C. Obstructive sleep apnea for the dental hygienist: Overview and parameters for interprofessional practice. Can J Dent Hyg. 2011;45(4):238-53.
4. Kornegay EC, Brame JL. Obstructive sleep apnea and the role of dental hygienists. J Dent Hyg. 2015 Oct;89(5):286-92.
5. Ahmad NE, Sanders AE, Sheats R, et al. Obstructive sleep apnea in association with periodontitis: a case-control study. J Dent Hyg. 2013 Aug; 87(4):188-99.
6. Minichbauer BC, Sheats RD, Wilder RS, et al. Sleep medicine content in dental hygiene education. J Dent Ed. 2015 May; 79(5):484-92.
7. Gunaratnam K, Taylor B, Curtis B, et al. Obstructive sleep apnoea and periodontitis: A novel association. Sleep Breath. 2009 Aug;13(3):233-9.
8. Shamsuzzaman AS, Winnicki M, Lanfranchi P, et al. Elevated C-reactive protein in patients with obstructive sleep apnea. Circulation. 2002 May;105(21):2462-4.
9. Bravo Mde L, Serpero LD, Barceló A, Barbé F, et al. Inflammatory proteins in patients with obstructive sleep apnea with and without daytime sleepiness. Sleep Breath. 2007 Sep11(3):177-85.
10. Iacopino AM. Periodontitis and diabetes interrelationships: role of inflammation. Ann Periodontol. 2001 Dec;6(1):125-37.
11. Loos BG. Systemic markers of inflammation in periodontitis. J Periodontol. 2005 Nov; 76(Suppl. 11): 2106-15.
12. Nashi N, Kang S, Barkdull GC, et al. Lingual fat at autopsy. Laryngoscope. 2007 Aug; 117(8):1467-73.
13. Shigeta Y, Ogawa T, Ando E, et al. Influence of tongue/mandible volume ration on oropharyngeal airway in Japanese male patients with obstructive sleep apnea. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011 Feb;111(2):239-43.
14. Enciso R, Clark G. Comparing the Berlin and the ARES questionnaire to identify patients with obstructive sleep apnea in a dental setting. Sleep Breath. 2011 Jan; 15(1):83-9.
15. Chung F, Yang Y, Liao P. Predictive performance of the STOP-BANG score for identifying obstructive sleep apnea in obese patients. Obese Surg. 2013 Dec; 23(12):2050-7.
16. Karim, A. Emerging applications: Screening OSA by modified pictorial Epsworth Sleepiness Scale in Indian subjects. Indian J Tuberc. 2015 Oct; 62(4): 222-5.
17. Nuckton TJ, Glidden DV, Browner WS, et al. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006 Jul; 29(7):903-8.
18. Ramar, K, Dort, LC, Katz, SG, et al. Clinical practice guidelines for the treatment of obstructive sleep apnea and snoring with oral appliance therapy: an update for 2015. J Clin Sleep Med. 2015 Jul;11(7):773-827.
19. Sutherland K, Chan AS, Cistulli PA. Three-dimensional assessment of anatomical balance and oral appliance treatment outcome in obstructive sleep apnoea. Sleep Breath. 2016 Sep;20(3):903-10.
20. Gakwaya S, Melo-Silva CA, Borel JC, et al. Impact of stepwise mandibular advancement on upper airway mechanics in obstructive sleep apnea using phrenic nerve magnetic stimulation. Respir Physiol Neurobiol. 2014 Jan1;190:131-6.
21. Sasao Y, Nohara K, Okuno K, et al. Videoendoscopic diagnosis for predicting the response to oral appliance therapy in severe obstructive sleep apnea. Sleep Breath. 2014 Dec;18(4):809-15.
22. Francisco EM, Johnson TL, Freudenthal JJ, Louis G. Dental hygienists' knowledge, attitudes and practice behaviors regarding caries risk assessment and management. J Dent Hyg. 2013 Dec; 87(6): 353-61.
23. Chhokar S, Laughter L, Rowe D. Perceptions of registered dental hygienists in alternative practice regarding silver diamine fluoride. J Dent Hyg. Aug 2017;91(4)53-60.
24. Barao D, Essex G, Lazar A, Rowe D. Detection of early-stage oral cancer lesions: a survey of California dental hygienists. J Dent Hyg. Dec 2016;90(6):346-53.
25. Bradshaw B, Bruhn A, Newcomb T, et al. Disaster preparedness and response: a survey of US dental hygienists. J Dent Hyg. Oct 2016:90(5):313-22.
26. Schotland HM, Jeffe DB. Development of the obstructive sleep apnea knowledge and attitudes (OSAKA) questionnaire. Sleep Medicine. 2003 Sep;4(5):443-50.
27. Kandray DP, Juruaz D, Yacovone M, Chang, GA. Inter-rater reliability of the Mallampati classification for patients in a dental hygiene clinic. J Dent Hyg. 2013 Jun; 87(3):134-6.
28. Southwell C, Moallem, M, Auckley, D. Cardiologist's knowledge and attitudes about obstructive sleep apnea: a survey study. Sleep Breath. 2008 Nov;12(4):295-302.
29. American Dental Hygienists' Association. Standards for clinical dental hygiene practice [Internet]. Chicago: American Dental Hygienists' Association. 2016 [cited 2019 April 26]. Available from: https://www.adha.org/resources-docs/2016-Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf
30. Koren D, Chirinos JA, Katz LE, et al. Interrelationships between obesity, obstructive sleep apnea syndrome and cardiovascular risk in obese adolescents. Int J Obes (Lond). 2015 Jul;39:1086-93.
31. Logan AG, Tkacova R, Perlikowski SM, et al. Refractory hypertension and sleep apnoea: effect of CPAP on blood pressure and baroreflex. Euro Resp J. 2003 Feb;21(2):241-7.
32. Pamidi S, Tasali E. Obstructive sleep apnea and type 2 diabetes: is there a link? Front Neurol. 2012 Aug 13;3:126.
33. Loke YK, Brown JW, Kwok CS, et al. Association of obstructive sleep apnea with risk of serious cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012 Sep 1;5(5):720-8
34. Furukawa T, Suzuki M, Funatogawa I, et al. Screening method for severe sleep-disordered breathing in hypertensive patients without daytime sleepiness. J Cardiol. 2009 Feb;53(1):79-85.