You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In 2012, it was estimated that each year, more than 260 million direct resin-based composite (RBC) dental restorations were placed worldwide.1 In 2019 this number will be greater, but the light-curable products (e.g., composites, adhesives, orthodontic and luting resins) that the dentist uses are all "semi-finished" products: their performance and clinical success depend on how well they are light-cured in the tooth. Thus, the dental light-curing unit (LCU) has become an essential piece of equipment in every dental office; however, there is a general lack of understanding about dental LCUs, resulting in many dentists purchasing the cheapest light and not monitoring the performance of the light over time.2-5 After reading this article, the reader should understand that there can be substantial differences in the emission spectra, radiant power, irradiance, and beam profiles of a representative sample of LCUs and what to look for when purchasing a new LCU.
Curing Lights Are Medical Devices
In most countries, dental LCUs are classified as medical devices and therefore should be registered and cleared for use on patients. Nevertheless, the sales of budget-priced unregulated and untested LCUs, especially those available for purchase on Internet sites, have increased substantially. Although it may seem attractive to purchase 10 or more budget LCUs for the same price as a quality LCU, clinicians are strongly advised not to use any unregistered medical device on their patients because such equipment may harm the patient, may result in legal challenges, and may even be an electrical hazard.
The Light From Light-Emitting Diode (LED) Curing Lights
Small, battery-operated, energy-efficient LED curing lights now dominate the market.5,6 They have a range of features and performance; nevertheless, the cost of the unit is one of the first factors that many clinicians consider when purchasing a new LCU. There can be considerable differences between the light outputs from different LCU models that are not readily visible to the purchaser and that are not adequately described by a single irradiance value; the purchaser may also be confused by the terminology used in the advertisements, which may include vague or possibly misleading terms such as intensity, power density, lux, or brightness of the LCU.7
Table 1 lists how light output should be reported from an LCU using the internationally accepted International System of Units (SI) terms of radiant power (mW), spectral radiant power (mW/nm), radiant exitance (mW/cm2), and the irradiance received at a surface (also in mW/cm2). The amount of energy received by the resin (Joules/cm2) is measured by the irradiance (mW/cm2) multiplied by the exposure time (seconds). When these SI terms are used, there is less chance for ambiguity.8
Relationship Between Power, Area, and Irradiance
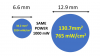
Figure 1 illustrates that by reducing the tip diameter, a high irradiance can be delivered using less power and shows why comparing LCUs on irradiance values alone can be misleading.
Many budget-priced LCUs appear to be equivalent to the LCUs from quality manufacturers because they deliver the same irradiance value, but on closer examination, most budget LCUs have only an effective 6- or 7-mm diameter light tip. The effective light tip diameter is not the external diameter of the head, but is instead the diameter from where useful light is emitted. Most light tips are circular, and the area used to calculate both the radiant exitance and the irradiance (mW/cm2) is derived from πr2. Thus, even small changes in the effective tip diameter will have a substantial effect on the area, the radiant exitance, and the irradiance. For example, reducing the effective tip diameter from 10 to 7 mm will halve the tip area, and thus, the power required to emit the same radiant exitance will be halved.
Effect of Distance
The radiant exitance at the light tip is the same as the irradiance at the light tip, but as the distance from the light tip increases, the irradiance received by the RBC declines. This decline does not follow the inverse-square law, because the light beam from most LCUs is a collimated or focused beam of light. For some LCUs the irradiance value can decline rapidly, whereas for other LCUs, depending on the optical design, the beam may be more collimated and there may be less reduction in the irradiance received. Because the light tip may often be at least 6 to 8 mm away from the resin at the bottom of a proximal box,9 manufacturers should report the irradiance that their light delivers at distances up to 8 mm away from the light tip. It would also be useful to know at what distance from the light tip the irradiance drops to 50% of the irradiance delivered at 0 mm.
Light Tip Diameter and Angle
Do not be confused by LCUs that have large heads, thinking that they will cover a larger area. Since the effective light tip diameter is not the external diameter, but is instead the diameter from where useful light is emitted, if you wish to light-cure an entire restoration with just one exposure, then the effective light tip must cover the entire restoration. Thus, a wide tip (10 to 12 mm internal diameter) is suggested for bulk curing an entire MOD restoration, whereas a narrower tip (6 to 8 mm in diameter) is suggested for curing small increments of RBC, or for Class V restorations that are close to the gingivae. Long light guides with a 40°–50° angle make them difficult to position over posterior restorations.10-12 Light guides that have 80°–90° tips or LCUs that have the LED emitter in a low profile head are preferred.
Emission Spectrum
The user should ensure that the LCU emits light at the wavelengths required to activate the photoinitiators within the resin being used.13 Previously, a quartz tungsten halogen (QTH) bulb was the most commonly used light source. These QTH units emit a broad spectral emission of violet and blue light that can activate all the photoinitiators that are used in current RBCs. Thus, it was not necessary to know the exact emission spectrum from a QTH light. In sharp contrast, single-peak LED curing lights can only deliver limited spectral coverage and the LED used in these units (Figure 2 A, B, C, and D) was chosen to activate the camphorquinone (CQ) photoinitiator used in most RBCs. This initiator is activated by blue light with a maximum absorption at 468 nm. However, several other photoinitiators that are less yellow and react faster than CQ have been used as an alternative, such as trimethyl benzoyl-diphenylphosphine oxide (TPO) and 1-phenyl-1,2-propanedione (PPD). These initiators are most sensitive to ultraviolet or violet light between 380 and 410 nm, instead of light at 468 nm. Thus, the conventional, single-peak LED curing lights that deliver very little light below 420 nm (Figure 2 A, B, C, and D) will not activate the alternative initiators used in these RBCs, but they will activate the CQ initiator.6,13 Consequently, some LED curing lights, such as the Valo™ (Ultradent, ultradent.com), the Light 405 (GC America, gcamerica.com), Translux 2Wave (Kulzer, kulzer.com), and the Bluephase® G4 (Ivoclar Vivadent, ivoclarvivadent.com), now include additional LED emitters that produce light at lower wavelengths, in the violet range, which makes these LCUs able to activate a broader range of photoinitiators (Figure 2 E, F, G, and H). The number and location of these spectral emission peaks varies between manufacturers, as does each peak's relative contribution to the total power output during light exposure. However, unless the LCU is carefully designed, the addition of a variety of different wavelength LED emitters can negatively affect the uniformity of the light beam from the LCU.14 This lack of light-beam uniformity may then affect both the irradiance and wavelengths received at different locations across the restoration. This will adversely affect the polymerization of the RBC,15,16 the bond strength, the overall strength of the RBC, color stability of the RBC, and wear resistance of the RBC, and it will increase the amount of chemicals leaching from the RBC.7,13,17
The Impact of Light-Beam Uniformity
Beam profiling of light sources using a digital camera is commonly performed to examine the uniformity of light beams and lasers.18 Both 2-dimensional and 3-dimensional images of the irradiance across the tip of the light source have shown that the irradiance from most dental LCUs is not uniform.7,14,19-21 Thus, the single irradiance value and emission spectra that are often quoted to describe the output from the LCU should be interpreted with caution because the reader may think that the single value represents the output across the entire tip of the LCU. Instead, this irradiance value and emission spectrum only reflect an average value that does not take into account any nonuniformity in the light output across the tip of the LCU (Figure 3) nor the effect of distance from the tip of the LCU.
In view of the hot spots of very high irradiance at the light tip, the outputs from three LCUs were rescaled to a maximum of 12,000 mW/cm2 (Figure 4). Although the average tip irradiance values from these three LCUs ranged from 1,815 to 2,231 mW/cm2, it can be seen that there were “hot spots” of high irradiance close to ~ 12,000 mW/cm2 from lights A and B that may cause uneven polymerization across the RBC and may also cause soft tissue burns.13,15,16,21,22 In contrast, light F delivered a more uniform irradiance across the light tip.
To illustrate the effect of the beam profile, Figure 5 superimposed the wide beam profile light (11.6 mm effective tip diameter) and the narrow beam profile (6.6 mm effective tip diameter) of a smaller tip LCU over a central incisor and a molar tooth. The differences in both the width and uniformity of coverage are striking.
Therefore, if you wish to light-cure an entire restoration with just one exposure, then the light tip should be wide enough to cover the restoration; otherwise multiple exposures to the occlusal, lingual, and buccal surfaces are required to fully cover the restoration.
A recent innovation for LCUs is the introduction of a “smart” technology feature on the Bluephase G4 and Powercure lights (Ivoclar Vivadent) to detect if the light tip moves off the restoration, in which case the LCU automatically adds additional exposure time.23 If the LCU moves far enough away from the tooth, the LCU turns off. This feature is similar to the “lane assist” technology in cars and should help to keep the LCU on target, thus producing better RBC restorations.
Desirable Curing Light Characteristics
In conclusion, when choosing a dental LCU, it is recommended that the purchaser select an LCU that has:
| • | been approved by the regulatory authorities for use on dental patients. |
| • | an ergonomic design that fits both large and small hands. |
| • | easily found controls that provide tactile and visual identification of settings. |
| • | a right angle on the curing tip so that the light beam can be perpendicular to the surface being polymerized, such as the occlusal surface of a third molar or the lingual of the mandibular anterior teeth. |
| • | a sealed system that allows easy cleaning and optimum infection control. |
| • | form-fitting infection control barriers that have minimal impact on light transmission. |
| • | a broad emission spectrum that will activate all resin photoinitiator formulations, so that the user does not have to be concerned with what is in the resin being used. |
| • | a choice of corded or non-corded models. |
| • | the ability to set the LCU to allow lower or higher output to adapt to various clinical situations, such as curing through an all-ceramic crown. |
| • | easy charging with long battery life and a low cost to replace the battery. |
| • | a shield on the curing light that blocks stray light and allows the clinician to accurately monitor the position of the light tip over the intended restoration. |
| • | the option to change the diameter of the curing spot from large to small to cover large restorations, crowns, and veneers, or small Class V restorations. |
| • | “smart” light features, similar to lane-assist technology, that sense when the light tip moves away from a tooth, warn the dentist, and automatically increase the exposure time. |
Tips to Enhance Clinical Success
| • | Verify that the LCU will polymerize the resin: When using a new material, review manufacturer's curing instructions and verify polymerization of both a light and dark shade of the RBC using the intended exposure protocol, the thickness of RBC, and the distance that will likely be used. |
| • | In-service training: Periodically review techniques with staff to educate and train on proper light use, cleaning, and maintenance of the LCU. Regardless of the curing light used, the appropriate clinical technique is crucial. Looking away is not recommended when light-curing because the tip may stray off target.24-27 |
| • | Keep the light tip clean. Gently remove any materials cured to the tip of light. Use a protective barrier. Periodically verify the output of the light using a radiometer. |
| • | Controlling heat: Energy (Joules) is the radiant power (Watts) multiplied by time (seconds). Thus, powerful lights with high irradiance can cause significant heating, potentially harming hard and soft tissues if used for too long. Heating can be minimized with a gentle air stream on the tooth and separating each exposure by 3 to 5 seconds for the heat to dissipate.26 |
| • | Eye safety: Blue light can potentially disturb circadian rhythm or accelerate retinal aging, so needless exposure should be minimized28-32 by using an appropriate orange shield or orange glasses so that the operator can safely watch and monitor the position of the curing light.33-35 |
Conclusions
| 1. | There can be considerable differences in the effective tip area, radiant power, radiant exitance, emission spectra, and beam profiles of dental curing lights. |
| 2. | A single irradiance value does not adequately describe the irradiance from most LCUs. Even though the average irradiance across the light tip may be ~ 2,000 mW/cm2, some LCUs may have localized hot spots with very high irradiance values of 12,000 mW/cm2 or more. |
| 3. | Small changes in the tip diameter will produce substantial changes in the calculated irradiance value. |
About the Authors
Richard B. Price is a professor and Director of Digital Dentistry at Dalhousie University, Faculty of Dentistry, Halifax, Nova Scotia, Canada.
Gordon Christensen is chief executive officer of Clinicians Report Foundation, chief executive officer of Practical Courses, and a clinical professor at the University of Utah.
Stella Braga is a doctoral student from the Federal University of Uberlandia, Brazil. She was studying at Dalhousie University, Faculty of Dentistry, Halifax, Nova Scotia, Canada, supported by a grant from grant CAPES - PDSE - 88881.189639/2018-01.
References
1. Heintze SD, Rousson V. Clinical effectiveness of direct class II restorations - a meta-analysis. J Adhes Dent. 2012;14(5):407-431.
2. Kopperud SE, Rukke HV, Kopperud HM, Bruzell EM. Light curing procedures - performance, knowledge level and safety awareness among dentists. J Dent. 2017;58:67-73.
3. Ernst CP, Price RB, Callaway A, et al. Visible light curing devices - irradiance and use in 302 German dental offices. J Adhes Dent. 2018;20(1):41-55.
4. Bansal R, Bansal M, Walia S, et al. Assessment of efficacy and maintenance of light-curing units in dental offices across Punjab: a clinical survey. Indian J Dent Sci. 2019;11(1):42-45.
5. Burke FJT, Wilson NHF, Brunton PA, Creanor S. Contemporary dental practice in the UK. Part 1: demography and practising arrangements in 2015. Br Dent J. 2019;226(1):55-61.
6. Jandt KD, Mills RW. A brief history of LED photopolymerization. Dent Mater. 2013;29(6):605-617.
7. Price RB, Ferracane JL, Shortall AC. Light-curing units: a review of what we need to know. J Dent Res. 2015;94(9):1179-1186.
8. Kirkpatrick SJ. A primer on radiometry. Dent Mater. 2005;21(1):21-26.
9. Price RB, Dérand T, Sedarous M, et al. Effect of distance on the power density from two light guides. J Esthet Dent. 2000;12(6):320-327.
10. Christensen GJ. Should your next curing light be an online bargain? Clinicians Report. 2013;6(10):1-6.
11. André CB, Nima G, Sebold M, et al. Stability of the light output, oral cavity tip accessibility in posterior region and emission spectrum of light-curing units. Oper Dent. 2018;43(4):398-407.
12. Soares CJ, Rodrigues MP, Oliveira LRS, et al. An evaluation of the light output from 22 contemporary light curing units. Braz Dent J. 2017;28(3):362-371.
13. Rueggeberg FA, Giannini M, Arrais CAG, Price RBT. Light curing in dentistry and clinical implications: a literature review. Braz Oral Res. 2017;31(suppl 1):e61.
14. Michaud PL, Price RB, Labrie D, et al. Localised irradiance distribution found in dental light curing units. J Dent. 2014;42(2):129-139.
15. Price RB, Labrie D, Rueggeberg FA, et al. Correlation between the beam profile from a curing light and the microhardness of four resins. Dent Mater. 2014;30(12):1345-1357.
16. Issa Y, Watts DC, Boyd D, Price RB. Effect of curing light emission spectrum on the nanohardness and elastic modulus of two bulk-fill resin composites. Dent Mater. 2016;32(4):535-550.
17. Fujioka-Kobayashi M, Miron RJ, Lussi A, et al. Effect of the degree of conversion of resin-based composites on cytotoxicity, cell attachment, and gene expression. Dent Mater. 2019;35(8):1173-1193.
18. Dickey FM, ed. Laser Beam Shaping: Theory and Techniques. 2nd ed. Boca Raton, FL: CRC Press, Taylor & Francis Group; 2014.
19. Harlow JE, Sullivan B, Shortall AC, et al. Characterizing the output settings of dental curing lights. J Dent. 2016;44:20-26.
20. Price RB, Labrie D, Rueggeberg FA, Felix CM. Irradiance differences in the violet (405 nm) and blue (460 nm) spectral ranges among dental light-curing units. J Esthet Restor Dent. 2010;22(6):363-377.
21. Shimokawa CAK, Turbino ML, Giannini M, et al. Effect of light curing units on the polymerization of bulk fill resin-based composites. Dent Mater. 2018;34(8):1211-1221.
22. Maucoski C, Zarpellon DC, Dos Santos FA, et al. Analysis of temperature increase in swine gingiva after exposure to a Polywave® LED light curing unit. Dent Mater. 2017;33(11):1266-1273.
23. Bluephase G4. Ivoclar Vivadent. http://www.ivoclarvivadent.com/en/p/all/bluephase-g4. Accessed May 1, 2019.
24. Samaha S, Bhatt S, Finkelman M, et al. Effect of instruction, light curing unit, and location in the mouth on the energy delivered to simulated restorations. Am J Dent. 2017;30(6):343-349.
25. Federlin M, Price R. Improving light-curing instruction in dental school. J Dent Educ. 2013;77(6):764-772.
26. Zarpellon DC, Runnacles P, Maucoski C, et al. Controlling in vivo, human pulp temperature rise caused by LED curing light exposure. Oper Dent. 2019;44(3):235-241.
27. De Souza GM, El-Badrawy W, Tam LE. Effect of training method on dental students' light-curing performance. J Dent Educ. 2018;82(8):864-871.
28. Vicente-Tejedor J, Marchena M, Ramírez L, et al. Removal of the blue component of light significantly decreases retinal damage after high intensity exposure. PLoS One. 2018;13(3):e0194218.
29. Chaopu Y, Wenqing F, Jiancheng T, et al. Change of blue light hazard and circadian effect of LED backlight displayer with color temperature and age. Opt Express. 2018;26(21):27021-27032.
30. Price RB, Labrie D, Bruzell EM, et al. The dental curing light: a potential health risk. J Occup Environ Hyg. 2016;13(8):639-646.
31. O'Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye (Lond). 2016;30(2):230-233.
32. Bruzell Roll EM, Jacobsen N, Hensten-Pettersen A. Health hazards associated with curing light in the dental clinic. Clin Oral Investig. 2004;8(3):113-117.
33. Soares CJ, Rodrigues MP, Vilela AB, et al. Evaluation of eye protection filters used with broad-spectrum and conventional LED curing lights. Braz Dent J. 2017;28(1):9-15.
34. Bruzell EM, Johnsen B, Aalerud TN, Christensen T. Evaluation of eye protection filters for use with dental curing and bleaching lamps. J Occup Environ Hyg. 2007;4(6):432-439.
35. Berry EA 3rd, Pitts DG, Francisco PR, von der Lehr WN. An evaluation of lenses designed to block light emitted by light-curing units. J Am Dent Assoc. 1986;112(1):70-72.