You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
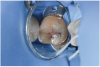
Often patients present for an examination with the clinical finding of an occlusal fissure similar to that shown in Figure 1, yet there is no clinically perceptible “stick” with an explorer. The clinician thus faces the decision of whether occlusal decay exists requiring a restoration or whether the lesion should merely be “watched” to determine if it progresses further. To make the correct decision, an understanding of the detection and classification of pit-and-fissure lesions is needed.
For nearly a century, American dental schools have taught the technique of evaluating fissure caries by the use of an explorer (often sharpened) to probe firmly into the pit or fissure to determine the amount of tugback. Resistance to removal of the explorer, or “finding a stick,” has been considered an indicator of the presence of caries that warrants the surgical intervention of a restoration, and it is a widely used detection method in the United States.1,2 However, a large body of research-based evidence that has advanced the dental industry's understanding of both tooth structure and the caries process in fissure caries has demonstrated that this traditional explorer test is no longer a valid approach.3-6
Why Occlusal Caries Is Underdiagnosed
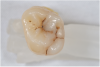
The use of fluoride to prevent dental caries has a long history of success. Enamel exposed to fluoride in water, dentifrice, and foods has been shown to be more resistant to acid attack than enamel not exposed to fluoride.7 Fluoride use is especially beneficial in addressing smooth-surface caries; however, it may complicate the detection of caries in pits and fissures. The breakdown from caries of harder, fluoride-treated enamel around pits may be delayed until long after significant dentinal damage has occurred.7 Occlusal caries may, therefore, be underdiagnosed, facilitating caries progression and further weakening of the tooth. Some fissures may undergo such an extensive progression under such circumstances that the first restoration will risk a pulp exposure (Figure 2).7 A new approach, therefore, needs to be adopted for the diagnosis of occlusal fissure caries that avoids both the underdiagnosis of occlusal caries and the potential pitfall of merely “watching” a carious fissure rather than restoring it.
“Hidden” Caries
Also called “occult caries” or “non-cavitated caries,” “hidden” carious lesions of fluoridated enamel are described as grooves that cannot be probed and, thus, appear to be closed, but may show a radiolucency on a radiograph.8 However, the groove itself represents a developmental defect that functions as a cavitation would on a smooth surface, namely to allow fluid and nutrition to seep down to the bacteria in dentin, where a carious lesion can flourish.
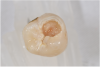
When such a fissure that does not present an explorer “stick” is explored with a small-diameter bur in a procedure called a “caries biopsy,” caries is nearly always found in areas with an underlying discoloration or shadow.9 Any caries discovered can then be excavated where needed. The susceptibility of a fissure to explorer probing for a “stick” is, therefore, irrelevant to the diagnosis of caries within the fissure (Figure 3 and Figure 4).
Deficiencies of Explorer Test
The fact that caries can progress in a groove or pit that is seemingly intact and cannot be penetrated with an explorer makes the explorer test imprecise. The ongoing use of the explorer test and the lack of better caries diagnostic criteria may lead conscientious practitioners to either intervene too soon when little disease exists or avoid exploring or restoring these lesions due to the concern of weakening the tooth by the placement of a large restoration. If diagnosis is delayed inappropriately, more extensive loss of tooth structure, with the accompanying increased risk of insult to the pulp, may then create a requirement for more advanced treatment, which could even involve endodontic therapy.
Further, research has long shown that not only is the explorer “stick” inaccurate, but that attempted or actual penetration of a suspected lesion by an explorer can actually damage tooth structure (Figure 5) and even transmit caries bacteria into it. In fact, sharp explorers have been shown to create defects in completely healthy enamel, which can lead to future caries.10,11 Additionally, probing the microbiomes of fissures from tooth to tooth can carry specific bacterial species from a given fissure to other fissures not previously infected by those bacterial species.12
Interestingly, dentistry's current system of classifying carious lesions, devised by G.V. Black more than a century ago, is based not upon characteristics or severity of the lesion but upon the surface based on the planned treatment.13 As newer options for managing early carious lesions with composite resin have come into widespread use, more precise descriptions of these lesions have become essential and have promoted more conservative restorations. An additional advantage of conservative preparation design when using conventional and flowable composite placement is the allowance for a more detailed approach to caries diagnosis.
Shortcomings of Radiographs for Evaluating Occlusal Caries
Unlike interproximal lesions, where mineral structure in a single layer of enamel can be reliably detected on a bitewing radiograph,14 occlusal lesions occur between cusps, where thicker, multiple layers of occlusal enamel tend to block radiographic evidence of dentin caries until extensive damage has occurred. Usually, if an occlusal lesion is detected on a bitewing, it is relatively large, while false positives are also common.15-17
Validated Diagnostic Systems
Several decades ago, an international group combined an in-depth review of all of the evidence supporting practices in fissure diagnosis with their own extensive clinical experience to develop a diagnostic algorithm that is based upon visual evaluation. After undergoing clinical validation in multiple countries by numerous investigators, this approach was codified18 and published19 as the International Caries Detection and Assessment System (ICDAS). ICDAS consists of a clinical pathway for evaluation of fissures using a set of visual criteria instead of the traditional explorer “stick.” The original “full code” system identifies six categories of disease that are still used in clinical research. However, after deployment of the system in clinical practice, a simpler “merged codes” classification was developed consisting of only three categories of disease.
ICDAS was first adopted as the standard curriculum in many European20 and then South American21 dental schools. More recently, a consensus meeting of representatives of a majority of North American schools took place, resulting in the development of a similar curriculum framework for caries management that includes ICDAS as the diagnostic model. Following its publication, this framework was reviewed and accepted by most American dental schools and has been published as a curricula framework for North American dental schools.22
The American Dental Association subsequently convened a panel of experts who reviewed the cumulative work done to date and then developed a simplified diagnostic system based on the same clinical approach. The resulting Caries Classification System (CCS)23 consolidates the six categories of disease into three (similar to the ICDAS merged codes system). This system has been published and validated as well, with at least one pilot study showing better clinical concordance and provider acceptance than within the original framework of ICDAS.24 The ICDAS and CCS classifications are summarized in Table 1.
Appropriate Diagnostic Technique in Light of Current Evidence
It has long been observed that subtle changes in the appearance of a fissure correspond to the extent of caries.15,25 Current evidence indicates that the optimal approach to evaluating pit-and-fissure caries is to conduct the evaluation with the teeth clean and with adequate light and magnification, using a ball-ended periodontal probe26 or explorer as required to only evaluate open cavitation or surface roughness rather than probe for lesions. As a baseline reference, Figure 6 and Figure 7 show a sound groove, and Figure 8 through Figure 16 show progression of disease.
To diagnose pit-and-fissure caries, clinically the tooth being assessed should first be wet, and the practitioner evaluates its pits and grooves for any decalcification, which typically presents as a chalky white area that follows the depth of the groove (Figure 10 and Figure 11). This finding with the tooth being wet defines an ICDAS code 2 lesion. Next, the grooves are dried completely using a 5-second air stream, and the clinician notes any areas of chalkiness in the now-dry grooves. Any such area of chalky decalcification noted only after drying would represent an ICDAS code 1 lesion (Figure 8 and Figure 9). Code 1 and/or code 2 lesions are classified as CCS code 1 initial lesion. If no chalkiness is noted in either a wet or dry groove or pit, the tooth structure is classified as sound and documented as ICDAS and CCS code 0 sound structure (Figure 6 and Figure 7). The presence of stain and hypocalcification should be disregarded.
Next, regardless of chalkiness, the clinician examines the dry grooves for the presence of any areas of localized enamel breakdown, or microcavitations, which represents ICDAS code 3 lesions (Figure 12 and Figure 13). Additionally, the presence of an underlying shadow, which indicates dentin caries showing through, is considered an ICDAS code 4 lesion (Figure 14). Either or both of these findings results in a classification of the tooth structure as CCS code 2 moderate.
Finally, if enamel is lost and carious dentin is visible, the tooth structure is classified as CCS code 3 advanced. The ICDAS system describes extent of the lesion by percentage of involved tooth surface. If less than half of the surface is involved, the lesion is an ICDAS code 5 lesion (Figure 15); when more than half of the surface is involved, the lesion is classified as an ICDAS code 6 lesion (Figure 16).
The case presented in Figure 17 and Figure 18 demonstrates significant pit-and-fissure caries that can be readily identified even though no clinical explorer “stick” was found.
Role of Caries Risk Assessment
Unlike previous classification systems, which were focused on the planned restoration, ICDAS and CCS classifications describe the current level of carious presentation. However, a crucial additional dimension—caries risk—should be evaluated before a treatment decision is made. Validated caries risk assessment instruments are available to provide this essential context for the clinical presentation.27-30
Caries is a disease of the whole mouth that is influenced by various factors, including diet, specifically the frequency of simple carbohydrate intake; salivary flow, with special attention given to medications that restrict flow; and, to a lesser extent, oral hygiene. As manifestations of this whole-mouth disease, carious lesions must therefore be considered within the context of overall caries risk. From this perspective, it stands to reason that treatment of, for example, an early lesion in a 60-year-old patient with no other active carious lesions, no salivary restriction, and low frequency of carbohydrate intake will require a different approach than an identical lesion in a 16-year-old patient who consumes sugary sports drinks four times per day and has several other active lesions.31,32
Summary
Evidence has accumulated showing that occlusal caries is frequently underdiagnosed and consequently progresses unimpeded toward the pulp, and that the use of an explorer to detect caries is both unreliable and potentially damaging. As a result, clinicians may benefit from adopting either of the two validated visual detection and classification systems for pit-and-fissure caries into their routine practice in conjunction with a validated caries risk assessment instrument. By adopting this approach, clinicians may reduce the amount of occlusal caries they either miss or dismiss as not significant enough to require restoration, thereby increasing opportunities to intervene at an earlier stage of the disease process and preserve more tooth structure.
About the Authors
Jan K. Mitchell, DDS, MEd
Associate Professor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
Martha G. Brackett, DDS, MSD
Professor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
Van B. Haywood, DMD
Professor
Department of Restorative Sciences
Dental College of Georgia at Augusta University
Augusta, Georgia
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Hamilton JC. Should a dental explorer be used to probe suspected carious lesions? Yes–an explorer is a time-tested tool for caries detection. J Am Dent Assoc. 2005;136(11):1526-1530.
2. Gordan VV, Riley JL 3rd, Carvalho RM, et al. Methods used by Dental Practice-based Research Network (DPBRN) dentists to diagnose dental caries. Oper Dent. 2011;36(1):2-11.
3. Lussi A. Validity of diagnostic and treatment decisions of fissure caries. Caries Res. 1991;25(4):296-303.
4. Lussi A. Comparison of different methods for the diagnosis of fissure caries without cavitation. Caries Res. 1993;27(5):409-416.
5. Penning C, van Amerongen JP, Seef RE, ten Cate JM. Validity of probing for fissure caries diagnosis. Caries Res. 1992;26(6):445-449.
6. McComb D, Tam LE. Diagnosis of occlusal caries: Part I. Conventional methods. J Can Dent Assoc. 2001;67(8):454-457.
7. Ricketts D, Kidd E, Weerheijm K, de Soet H. Hidden caries: what is it? Does it exist? Does it matter? Int Dent J. 1997;47(5):259-265.
8. Zadik Y, Bechor R. Hidden occlusal caries: challenge for the dentist. N Y State Dent J. 2008;74(4):46-50.
9. Committee ICDAS-IC. Rationale and Evidence for the International Caries Detection and Assessment System (ICDAS II). Indianapolis, IN: Indiana University; 2007.
10. Kuhnisch J, Dietz W, Stosser L, et al. Effects of dental probing on occlusal surfaces—a scanning electron microscopy evaluation. Caries Res. 2007;41(1):43-48.
11. Ekstrand K, Qvist V, Thylstrup A. Light microscope study of the effect of probing in occlusal surfaces. Caries Res. 1987;21(4):368-374.
12. Loesche WJ, Svanberg ML, Pape HR. Intraoral transmission of Streptococcus mutans by a dental explorer. J Dent Res. 1979;58(8):1765-1770.
13. Black GV. Operative Dentistry. Chicago, IL: Medico-Dental Publishing Company; 1908.
14. Kidd EA, Pitts NB. A reappraisal of the value of the bitewing radiograph in the diagnosis of posterior approximal caries. Br Dent J. 1990;169(7):195-200.
15. Ekstrand KR, Kuzmina I, Bjorndal L, Thylstrup A. Relationship between external and histologic features of progressive stages of caries in the occlusal fossa. Caries Res. 1995;29(4):243-250.
16. Espelid I, Tveit AB, Fjelltveit A. Variations among dentists in radiographic detection of occlusal caries. Caries Res. 1994;28(3):169-175.
17. Rudolphy MP, van Amerongen JP, Penning C, ten Cate JM. Validity of bite-wings for diagnosis of secondary caries in teeth with occlusal amalgam restorations in vitro. Caries Res. 1993;27(4):312-316.
18. International Caries Detection and Assessment System Coordinating Committee. Criteria manual: International Caries Detection and Assessment System (ICDAS II). icdas.org. 2005.
19. Ismail AI, Sohn W, Tellez M, et al. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007;35(3):170-178.
20. Schulte AG, Pitts NB, Huysmans MC, et al. European Core Curriculum in Cariology for undergraduate dental students. Eur J Dent Educ. 2011;15(suppl 1):9-17.
21. Martignon S, Gomez J, Tellez M, et al. Current cariology education in dental schools in Spanish-speaking Latin American countries. J Dent Educ. 2013;77(10):1330-1337.
22. Fontana M, Guzman-Armstrong S, Schenkel AB, et al. Development of a core curriculum framework in cariology for U.S. dental schools. J Dent Educ. 2016;80(6):705-720.
23. Young DA, Novy BB, Zeller GG, et al. The American Dental Association Caries Classification System for clinical practice: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2015;146(2):79-86.
24. Thompson VP, Schenkel AB, Penugonda B, et al. A pilot study of dentists' assessment of caries detection and staging systems applied to early caries: PEARL Network findings. Gen Dent. 2016;64(3):20-27.
25. Ekstrand KR, Ricketts DN, Kidd EA. Reproducibility and accuracy of three methods for assessment of demineralization depth of the occlusal surface: an in vitro examination. Caries Res. 1997;31(3):224-231.
26. Mattos-Silveira J, Oliveira MM, Matos R, et al. Do the ball-ended probe cause less damage than sharp explorers? An ultrastructural analysis. BMC Oral Health. 2016;16:39.
27. Young DA, Featherstone JD. Caries management by risk assessment. Community Dent Oral Epidemiol. 2013;41(1):e53-e63.
28. Domejean S, White JM, Featherstone JD. Validation of the CDA CAMBRA caries risk assessment—a six-year retrospective study. J Calif Dent Assoc. 2011;39(10):709-715.
29. Featherstone J, Domejean S, Jenson L, et al. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35(10):703-707,710-713.
30. American Dental Association. Caries Risk Assessment Form (Age >6). http://www.ada.org/~/media/ADA/Science%20and%20Research/Files/topic_caries_over6.ashx. Accessed December 14, 2017.
31. Young D, Ricks CS, Featherstone JD, et al. Changing the face and practice of dentistry: a 10-year plan. J Calif Dent Assoc. 2011;39(10):746-751.
32. Hurlbutt M, Young DA. A best practices approach to caries management. J Evid Based Dent Pract. 2014;14(suppl):77-86.