You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The United States (U.S.) is rapidly becoming one of the most racially and ethnically diverse nations in the world.1 According to the most recent 2010 U.S. census, minority groups will make up 35% of the American population by the year 2020 and become the majority of the population by the year 2050.2 Both the Institute of Medicine (IOM) and the Health and Human Services Action plan found persistent health care disparities between racial and ethnic minorities.3,4 The U.S. health care workforce has responded by incorporating cross-cultural education and training focusing on attitudes, knowledge, and skills in order to develop cultural competence in health care workers.3,4 Culturally Competent (CC) health care providers are described by the Office of Minority Health (OMH) as respectful and responsive to individual health beliefs, culture and language preferences.5 In addition, future health care providers should be aware of cultural humility, defined as the capacity to identify their predispositions, as a component of lifelong engagement in self-assessment to improve patient and provider relationships.6
A review of current literature for CC among health care providers identified a Systematic Review (SR) by Clifford et al. for culturally competent education (CCE) and training interventions in health and medical curricula.7 Inclusion criteria were articles published from 2006 to 2016, from Australia, Canada, New Zealand or the United States, and the focus of the review was to identify which strategies were effective for improving the cultural competence of university based health professional students in training.7 A total of sixteen studies met the inclusion criteria, 5 of the 16 studies were among medical students, four studies with nursing students, three targeted health sciences, and two each psychology and pharmacy students.7 The SR described three main types of education and training intervention strategies including integration of cultural competency into the curriculum, cultural immersion, and cultural awareness training.7 Results yielded a number of clear recommendations for improving future CC evaluations, however, the quality of evidence was insufficient to provide a strong basis for recommending the inclusion of one specific CCE and training strategy for university based health professionals.7
Similar research conducted by professional education associations to identify information for effective teaching strategies to foster CCE in dental schools is lacking. Outcomes from a survey conducted by the American Dental Education Association (ADEA) in the United States, and Canada found most dental schools include CCE in the first year of dental school, and only a small number continue to integrate CCE through all 4 years.8 The literature provides little direction concerning curriculum change or methodologies necessary to graduate CC dentists.
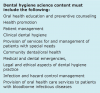
Dental hygiene (DH) literature is also elusive regarding the most effective methods for CCE despite the January 1, 2013 addition of standard 2-15 to the Dental Hygiene (DH) education standards stating that, "dental hygiene graduates must be competent in interpersonal and communication skills to effectively interact with diverse population groups and other members of the health care team."9 Dental hygiene education includes didactic courses providing the theory to prepare students for clinical practice, however students must also be able to apply this theory in practice.10 Ocegueda et al conducted a nationwide survey in 2016 to identify how CCE was being incorporated into the DH curriculum.11 The 19-item questionnaire addressing the curriculum methods, evaluation measures, program goals and employment of CCE was distributed to dental hygiene program directors (n=334) in the U.S.11 Of the 27% who responded, 91% reported they included CCE in the curriculum, and 72% included CCE in DH courses with goals, objectives and outcomes pertaining to cultural competency; lectures or seminars (83.1%) and community outreach (76.4%) were the most common educational methods.11 Fifty four percent of programs had definite learning objectives pertaining to CCE in community programs, but only 42% of the programs evaluated students based on CCE outcomes.11
To gain an understanding of cross-cultural adaptability among DH's and DH students, several studies13-15 have been conducted using the Cross-Cultural Adaptability Inventory (CCAI™) instrument.12 The CCAI™ is a fifty-item standardized instrument that measures four subscales of cross-cultural adaptability: emotional resilience, flexibility/openness, perceptual acuity, and personal autonomy.12 Tavoc et al conducted a study among practicing DH's and DH students (n=278) in Texas to determine if there was a difference between the two populations concerning cross-cultural adaptability.13 Using the CCAI™, Tavoc et al found no statistically significant difference among the groups, though, the authors concluded that DH education may be lacking in cross-cultural adaptability.13 DeWald and Solomon used the CCAI™ to see if there were any changes in DH students' cultural effectiveness by administering the test instrument at the following points in the curriculum: at orientation; at the end of the first year; and at the end of the second year.14 DeWald and Solomon found no significant improvement in cross-cultural effectiveness in their research outcomes.14 Their outcomes were similar in a previous study conducted by Magee et al. who studied randomly selected, culturally diverse DH programs (n=15) and non-culturally diverse programs (n=101) across the US.15 The CCAI™ outcomes found DH students (n=188) from both culturally diverse and non-culturally diverse programs possessed the qualities of personal autonomy and self-identity, necessary for cultural adaptability. However, the overall CCAI™ scores were lower than the norm for both groups.15 The investigator's conclusions suggested further education was needed to improve communication skills, confidence, and critical thinking skills for the treatment of a culturally diverse patient.15
Outcomes of numerous studies7,8,11,13-15 highlight the issues associated with the lack of guidelines for integration and evaluation of outcomes for CCE for health professionals. Although CCE is being integrated into health professions education, there is a lack of agreement regarding the most effective methods. Determining how to successfully integrate CCE in dental hygiene education is essential to satisfy the intent of CODA and to address the reality of oral health disparities. The purpose of this study was to explore how senior dental hygiene students' perceptions and experiences of cultural preparedness were influenced by treating a culturally diverse patient.
Methods
The study was granted approved status by the Massachusetts College of Pharmacy and Health Sciences (MCPHS) University Institutional Review Board (IRB081815D). A qualitative phenomenological study design was used and a purposive sample of senior dental hygiene students. The phenomenological design was chosen to in order to build broader themes and generate a theory inter-connecting the themes using an inductive process.16 Semi-structured focus groups were chosen to obtain a holistic perspective on ways to integrate CCE into the dental hygiene curriculum.
Participants
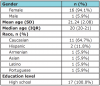
Senior dental hygiene students (DHS) in their second semester of clinical instruction in the MCPHS Bachelor of Science program were invited to participate in the study. An invitation to participate letter explaining the purpose of the voluntary study was distributed to the DHS. Students received the letter during a didactic course addressing cultural diversity while providing opportunities for enrichment rotations in community settings as part of the CODA Standard 2-8d (Figure 1).9 Inclusion criteria required that participants be available for both focus groups and provide treatment for a culturally diverse refugee patient. Exclusion criteria included being unable to attend the two focus groups or having had previous experiences treating a culturally diverse patient from a refugee population. After receiving and signing the informed consent, participants were asked to respond to the following demographic questions: sex, age, race, education (Table I).
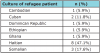
The patients came from a local community outreach program working with refugees entering the U.S. (Table II). The organization provides English language classes, General Educational Development (GED) classes, skills and resources needed to find employment as well as medical and dental care. As many of the refugees have had no previous access to dental services or coverage for the cost of care, the dental hygiene program has partnered with the local community program to provide preventative dental hygiene services. Many of the community sites do not have interpreters available thus requiring students to develop various methods and skills for communicating with the refugee patient population.
Instrument
Semi-structured interview questions were piloted among a focus group of DHSs prior to this study and served as the primary instrument for data collection (Table III). The focus group sessions occurred at two different times based on student clinical schedules and took place before and after the treatment of a refugee patient. There were two separate focus groups each consisting of (n=9) DHSs. The Principal Investigator (PI) conducted the focus groups with the assistance of a note taker to write down the responses of the students. The note taker was also able to capture any information that was difficult to transcribe on the recording device, for example, students talking over each other, or at the same time. Non-verbal data was not collected during the focus groups. The data reached saturation during the second focus group, when no new insights or perspectives from the participants were captured in the responses.16 To ensure credibility and transferability, the PI used a digital audio recording device, in addition to an independent note taker to transcribe the response data during the focus groups. Demographic statistics were calculated including frequency percentiles, means, and summary statistics. All statistical analyses were performed with data analysis software (STATA®, StataCorp LLC; version 11.2). Qualitative data was analyzed through thoughtful engagement of the transcripts, followed by assigning labels to understand the student's perceptions of the experience. Student's meanings of these experiences were implicit and a thematic analysis of the data was performed to fully understand the lived perceptions. Emergent themes were abstracted, and representative quotes were extracted for each collective theme.16 The PI used peer debriefing17 by having a colleague not associated with the research, explore and review the design process, data collection and analysis to ensure the information gathered was valid and to enhance the credibility of the research.
Results
Upon completion of the recruitment process, 18 dental hygiene students (DHSs) met the inclusion criteria (n=18). Participant demographics included that the majority were Caucasian (64.7%) females (94.1%), with a mean age of 21 years and high school was the highest level of education completed (100%). One student participant was eliminated from the data interpretation due their inability to treat a patient. The majority (47.1%) of the refugee patients identified themselves as being Haitian (Table II). The four emergent themes and representative quotes and are shown in Table IV.
Pre-treatment Questions/Responses
Awareness of Other Cultures. Prior to providing care for the patient, the most common theme reported for the meaning of being culturally competent, was having an awareness of other cultures, "Being culturally aware, not just of your own culture but those around you. We could be of the same race but our religious beliefs can be different." "Just being sensitive."
Open-Minded and Non-Judgmental. A majority of the participants reported that a clinician should prepare themselves to treat a culturally diverse patient by remembering to be open-minded and non-judgmental throughout the visit. Most students concurred that it was going to be a challenging experience and shared, "Don't get frustrated, it's not going to be easy" and "Keep an open mind" and, "[Remember to] ... not get overwhelmed."
Didactic Coursework and Extramural Experiences. Didactic coursework and extramural experiences were the most comment themes regarding preparation. All of the participants reported feeling as though their didactic courses and extramural experiences in dental hygiene had prepared them to treat a culturally diverse patient. "Review the lectures from DHY classes...[this can be a main resource to utilize in order to make the appointment go more smoothly]." "I think classes prepared us very well [for treating this type of patient]." "Classes and extramural rotations are making me feel more comfortable." All the students agreed with this participant, "I think we all feel prepared to tackle the battle."
Language and Culture. Language and culture were equally reported as possible obstacles or barriers in the treatment of a culturally diverse patient. One participant stated, "Language will be a barrier...how do we get them to understand?" Another shared, "Male and female roles in other cultures may be different and might be hard to get through." Many students expressed the importance of appointment preparation and the use of pictures, models and props throughout the visit in order to meet the challenges of communication in a different language. One participant reported, "If you don't know how to explain [something that comes up in the process of care] you can pull up the model [or diagrams] and use them." Another student stated while others concurred, "Use more visuals or models such as the typodont, throughout the appointment... [to be communicative throughout the visit]." (this was just to help with communication)
Post-treatment Responses
Unmet Patient Needs. The most common theme identified regarding successful treatment was the students' inability to address their patients' needs. One participant said, "The patient started crying, I felt so bad." Another student reported, "My patient was from Iraq andnever saw a dentist. We attempted to do a full mouth series on him, but he couldn't do it." One participant felt it was successful but, "At the second appointment, the patient waited 20 minutes until someone else who spoke her language could explain the treatment plan to her...[I felt bad cause she couldn't understand]."
Underestimated Potential Barriers and Knowledge. Following the initiation of treatment, the most common theme was that the potential barriers and knowledge associated with cultural diversity to have successful treatment had been underestimated by the students. Participants agreed with one student who shared, "There was a knowledge barrier on my part throughout the entire visit." All participants expressed feeling that they did not have enough knowledge and education on cultural diversity to carry out a successful visit. "We didn't have enough prior knowledge of what we were going to see or what to expect [with this specific type of patient]." Most of the participants reported they went into the experience over confident in regards to their ability to treat a culturally diverse patient. All participants concurred, "We over-anticipated how prepared we were." Most agreed, "I felt less prepared after the experience... [because I didn't know how much the process of care is affected with this type of patient]." Everyone reported the clinical experience was a better learning experience than learning about culture in a didactic setting. The opportunity to apply and use critical thinking skills was valued by all the student participants, "...seeing certain things in clinic [such as cultural oral habits] with the ... diverse refugee patient helped me more than just [learning] it in class."
Education. The most common theme identified in regards to being better prepared was the need for more education to increase their cultural knowledge and more exposure to culturally diverse patients. All of the participants agreed that they would like, "... specific lectures and classes on diverse cultures... [to better prepare them of what they are going to see in clinic]." The students recommended that having more didactic courses specifically focused on cultural diversity might increase their knowledge, "We need specific lectures to give us insight and views on specific cultures." Respondents also reported that they would gain more in clinical settings than inside the classroom, "We would learn more clinically with these types of patients, not in classroom." It was evident the students felt the opportunity to treat more culturally diverse patients was vital to successful patient care outcomes.
Clinical Experience with Diverse Cultures. All participants reported that this enrichment clinical experience was valuable, and that they felt that by becoming more educated in diverse cultures they would increase their confidence and become better prepared to care for culturally diverse patient populations. All the students agreed with the statement, "[We] have gotten a lot stronger after this [clinical] experience." They felt that the treatment of a culturally diverse patient was a great learning experience and added to their clinical development, "I would be so nervous in the real world if I hadn't had this experience [in a school setting first]." Providing preventive care to a culturally diverse patient helped all the participants recognize the importance of cultural awareness and the need to become competent in caring for a person from a culture that is different from one's own. Participants commented on the diversity of the U.S. and how vital it was to become comfortable in treating various cultures. All DHSs agreed that "We really need to know how to work with patients of different cultures," and "We need all the culturally diverse patients we can get now in school to be that more prepared in the real world." Participants also agreed that it is important to be challenged while still in school and recognized the value in making mistakes in the school setting in order to successfully prepare for the future. One participant stated and most others agreed, "I now feel more accepting, more open-minded and more culturally competent from this experience." All participants agreed this was a valuable learning experience to have as dental hygiene student.
Discussion
The purpose of this qualitative study was to explore the before and after perceptions and lived experiences of senior dental hygiene students after providing care for a culturally diverse patient from a refugee population. Guided by semi-structured questions in focus groups, students shared their knowledge, thoughts, feelings, and beliefs about treating a patient from a diverse culture. The questions encouraged DHSs to think critically about the meaning of cultural competence, their educational background and experiences with a culturally diverse patient. Before providing dental hygiene care, DHSs felt confident that their previous coursework along with various learning resources had prepared them to treat a culturally diverse patient. Following the dental hygiene care appointment, the students were not confident in their ability to provide care because they were more aware of the obstacles and challenges that interfered with meeting patient needs. They realized the depth of education that is needed, as well as the value of experiential learning. These findings correspond to previous research using the CCAI™ suggesting that more education is needed to improve communication skills, confidence, and critical thinking skills for the treatment of a culturally diverse patient.12-15 Although students were previously exposed to a curriculum accounting for patients with special needs, and had participated in community dental/oral health programs, once they were faced with the challenges presented by a patient from a different culture, they felt unprepared. However, students also felt their knowledge and abilities had increased after a single patient experience. Additionally, they felt the clinical immersion was a great learning experience, and actually supported their development in becoming more educated about different cultures. In contrast to previous research,7,8,11,13-15 this study used a phenomenological design to capture the voices and lived experiences of the participants. Limitations of this qualitative study included the small sample from a single educational program. Also, the students were novice clinicians, and no translators were provided. The data consisted of self-reported versions of students' own lived perceptions and experiences on cultural preparedness and may create bias limiting the study findings. There is also the possibility that the students did not understand the questions being asked or felt emotionally influenced by others throughout the course of the focus group questions and responses.
Conclusion
Dental hygiene education should include opportunities for students to apply what is learned in the classroom in a clinical setting. Exposing dental hygiene students to culturally diverse patients in a clinical setting can serve as an effective method for increasing cultural awareness and ultimately address oral health disparities. While this qualitative study makes a novel contribution to the literature, further research among larger groups, in multiple settings should be conducted to better understand how to improve and implement cultural education for future oral health care providers.
About the Authors
Bianca M. Capozzi, RDH, MSDH is a member of the adjunct faculty at the Forsyth School of Dental Hygiene; Lori J. Giblin-Scanlon, RDH, MS is an associate professor and associate dean of clinical sciences at the Forsyth School of Dental Hygiene; Lori Rainchuso, RDH, DHSc is an associate professor in the Doctor of Health Sciences Program; all at MCPHS University, Boston, MA
Corresponding author: Lori J. Giblin-Scanlon, RDH, MS; lori.giblin1@mcphs.edu
References
1. Institute of Medicine. In the nation's compelling interest: Ensuring diversity in the health care workforce. Washington, DC: The National Academies Press 2004.1-202.
2. Population Division US Census Bureau. Population estimates: Race/ethnicity [Internet]. Suitland (MD): United States Census Bureau; 2010 [cited 2017 Jul 14] Available from http://www.census.gov/popest/.
3. Institute of Medicine. Unequal treatment: What health care providers need to know about racial and ethnic disparities in health care [Internet]. Washington DC: National Academy of Medicine; 2002 [cited 2018 Feb 20] Available from https://www.nap.edu/resource/10260/disparities_providers.pdf
4. Department of Health and Human Services. Oral health in America: A report of the surgeon general. Rockville, MD: National Institutes of Health. [Internet] 2000 [cited 2017 July 18]. Available from https://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Documents/hck1ocv.@www.surgeon.fullrpt.pdf
5. Office of Mortality and Minority Health. What is cultural and linguistic competency? [Internet]. Washington DC:US Department of Health and Human Services; 2017 [modified 2017 Feb 9; cited 2017 July 18] Available from https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=1&lvlid=6.
6. National Partnership for Action. HHS action plan to reduce racial and ethnic health disparities: A nation free of disparities in health and health care [Internet]. Washington DC: US Department of Health and Human Services; 2017 [modified 2015 Nov; cited 2017 July 18] Available from https://minorityhealth.hhs.gov/assets/pdf/FINAL_HHS_Action_Plan_Progress_Report_11_2_2015.pdf.
7. Clifford A, Mc Calman J, Jongen C, Bainbridge R. Cultural competency training and education in the university- based professional training of health professionals: Characteristics, quality, and outcomes of evaluations. Divers Equal Health Care. May 2017;14(3):136-47.
8. Behar-Horenstein LS, Warren RC, Dodd VJ, Catalanotto FA. Addressing oral health disparities via educational foci on cultural competence. Am J Public Health. 2017 May;107(S1): S18-23.
9. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs [Internet]. Chicago (IL): American Dental Association 2017[modified 2013 Jan 1; cited 2017 July 18] Available from http://www.ada.org/~/media/CODA/Files/dh.ashx.
10. Wilkinson DM, Smallidge D, Boyd LD, Giblin L. Students' perceptions of teaching methods that bridge theory to practice in dental hygiene education. J Dent Hyg. Oct 2015;89(5):330.
11. Ocegueda DR, Van Ness CJ, Hanson CL, Holt LA. Cultural competency in dental hygiene curricula. J Dent Hyg. 2016 Jun;90 Suppl 1:5-14.
12. Kelley C, Meyers J. Cross-cultural adaptability inventory manual. Minneapolis, MN: NCS Pearson-Inc. 1995. 81p.
13. Tavoc T, Newsom R, DeWald JP. Cross-cultural adaptability of Texas dental hygienists and dental hygiene students: A preliminary study. J Dent Educ. 2009 May;73(5):563-70.
14. DeWald JP, Solomon ES. Use of the cross-cultural adaptability inventory to measure cultural competence in a dental hygiene program. J Dent Hyg. 2009 Summer;83(3):106-10.
15. Magee KW, Darby ML, Connolly IM, Thomson E. Cultural adaptability of dental hygiene students in the united states: A pilot study. J Dent Hyg. 2004 Winter;78(1):22-9.
16. Creswell JW, Plano Clark VL., ed. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage Publications; 2007. p. 248-249.