You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Disclaimer: Participants must always be aware of the hazards of using limited knowledge in integrating new techniques or procedures into their practice. Only sound evidence-based dentistry should be used in patient therapy.
Overview
There are several reasons why today's dental clinician needs to be observant when treating patients who may be using drugs, alcohol or nicotine. Medical emergencies during dental treatments spurred by health or drug interactions would be cause for concern. Long-term health of the oral cavity is another, but perhaps the most important consideration would be the quality of life and health that could be restored after abuse or addiction.
This course will review the various signs, symptoms and aspects that substance use disorders can have on our patients. We will limit our scope to the effects on the oral cavity and we will cover more commonly abused substances. Information will be provided for the clinician to make distinctions, begin safe dialogues, document patient comments and oral findings, and provide resources and follow-up support to patients with substance use disorders.
Focused chairside observation is essential considering that 50% of patients will reveal less about their lifestyles than they should. Unsubstantiated observations should not cause the clinician to assume the patient has a substance use disorder. Instead, careful questioning of the patient may reveal a substance use disorder. At the end of each section, we will review various approaches and acceptable means of guidance that a dental professional might employ with a patient regarding that particular substance. While this course is intended to encourage observation and detection of the signs and symptoms of various substance use disorders, sensitivity for the patient's right to privacy should be respected. Providing gentle educational explanations about a particular oral condition and posing either straightforward or benign questions to the patient about how or why a particular condition might be arising is the best professional action. If dental professionals develop a dialog that promotes trust, we ensure the patient feels safe in our care. Approximately 50% of general dentists provide their patients with nicotine cessation information but fewer get involved with alcohol or other substances. It is important for the dental professional to have broad-based knowledge regarding substance use disorders because a patient suspected of this disorder can be a challenge. Clinically, it is important to avoid drug treatment interactions or behavioral outbursts in the dental office and further support the patient as they attempt to become drug-free. Many times the dental office can serve as a safe and non-threatening source of cessation assistance. Creating referral protocols may help our patients find appropriate professional treatment.
Most scientists consider addiction to be a chronic, relapsing brain disease caused by persistent changes to cerebral structure and function. Using drugs repeatedly over time changes the brain in ways that persist long after the individual stops using. There are implications for oral health professionals in identifying and managing the patient who is abusing substances. Management issues relevant to delivery of oral care include:
| 1. | Identifying potential drug interactions, during oral care, with substances used. |
| 2. | Offering drug abuse cessation information. |
| 3. | Dealing with the erratic behavior of a patient who arrives at the oral care appointment while under the influence of drugs or alcohol.18 |
Introduction
Substance use disorders remain a significant epidemic in present day society. According to the 2013 National Survey on Drug Use and Health, 9.4% of the United States population (24.6 million Americans/age 12+) use illicit drugs. Illicit drugs include marijuana/hashish, cocaine, heroin, hallucinogens, inhalants, or prescription-type psychotherapeutics used for non-medical purposes.37,38
As contemporary dental professionals, it is important we are educated about the effects of commonly used and abused substances including alcohol and nicotine products. We come into contact with patients on a daily basis who range from non-users to addicts. Medical histories may present the opportunity for our patients to reveal their past and present habits regarding drug, nicotine and alcohol use, but up to 50% of patients, when surveyed, say they lie on medical histories due to embarrassment; fear of being judged; losing insurance benefits; or because they believed that information was none of the clinician's business. According to this same medical survey, patients, aged 25 to 34, are more likely to lie to their doctors than patients 55 and older. Specifically, younger patients lie about recreational drug use, sexual history, and smoking habits. Men were found to withhold the truth significantly more than women about how much they drink: 24% vs. 15%.11
The dental setting brings a wide variety of patients for treatment. Drug interactions, systemic reactions and side effects of medications are a few of the considerations we must take seriously as licensed professionals. The effects drugs, alcohol and nicotine have on teeth and the oral cavity is another health and educational matter of concern. Pairing this with the survey results, our patients are not revealing the true scope of substance use, presenting a need for a new communication paradigm where sensitivity and awareness need to be honed.
Overview of Substance Abuse
Types of Substance Users
A dental health care provider will come into contact with several different kinds of users of both legal and illegal substances. It is important to understand the types of users because this foundational information may help gain insight into the patient's lifestyle, then help determine how the dental professional may want to approach oral healthcare recommendations to the patient.
The Social User. The first type is the social user. The social user can take or leave a substance and does not make it a focal point in his or her life. The social user never puts themselves or others in harm's way while using a substance and shows no repetitive pattern. The social user does not use to excess.
The Substance Abuser. This type of drug abuser can stop using a substance and return to a somewhat normal life. The substance abuser may also be a "binge user," a person who uses to excess at times, but rarely shows a daily pattern of abuse. Although they may not use a drug on a daily basis, they are still susceptible to issues of a drug abuser.
The Addict. The addict is our third and most serious form of substance abuser. Addiction can be defined as a chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences.15 It is common for people who fit the profile of an addict to use different substances. An addict may abuse alcohol one decade and then move on to prescription medication. The behavior of moving from one addictive substance to another is called transference.
Stages of Substance Abuse
| • | Experimentation |
| • | Regular to Risky Use |
| • | Dependence |
| • | Addiction |
Experimentation, regular to risky use, dependence and addiction are the stages of substance abuse. These behaviors can be addressed and treated at any stage, despite popular myths that people must hit bottom before they can benefit from help. One role of a dental professional is to recognize symptoms and behaviors that could indicate a substance abuse pattern.
Experimentation. Substance use starts with a voluntary use of alcohol or other drugs. The user may be trying to erase an emotional problem but often there are other causes. An older person may self-medicate through alcohol consumption to cope with depression after losing a spouse. A teenager, angry about a parental divorce, may start smoking marijuana or huffing inhalants. Experimentation may also include a husband taking his wife's prescription painkiller to cope with recurring back pain.
Regular to Risky Use. The transition from regular to risky use and why it happens differs for every individual. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) estimates nearly one-third of Americans engage in risky drinking patterns. As a result, what constitutes "risky behavior" can be difficult to define. If a person's behavior worries those close to them, the behavior and suspicions should be addressed. There are groups and interventions that may reduce, stop or derail the progression to dependence. Partnership for Drug-Free Kids and Intervention Now provide information for interventions.
Dependence. In 1990, alcoholism and other chemical dependencies were described by the American Society of Addiction Medicine (ASAM) as primary, chronic, relapsing diseases with genetic, psychosocial, and environmental factors influencing their development and manifestations.1,19 Alcohol or drug dependence follows risky behavior. At this stage, alcohol or other drug use may not be compulsive or out of control. Many dependent people are able to work, maintain family relationships and friendships, and limit the use of alcohol or other drugs to certain time periods, such as weekends or evenings. However, it is also difficult for the impaired individual (and for others) to recognize the affects their substance use may be having on themselves, friends, coworkers and family members. Characteristics of dependence include:
| • | Repeated use of alcohol or other drugs leading to failure to fulfill major responsibilities related to work, family, school or other roles. |
| • | Repeatedly drinking or using drugs in situations that are physically hazardous, such as driving operating heavy machinery when intoxicated. |
| • | Repeated legal, familial and relationship problems surrounding the substance. |
Psychological dependence is a behavioral pattern characterized by drug craving, out of control drug usage, overwhelming desire to obtain a drug supply, drug use causing personal and legal problems, denial about the personal drug use, and continuing to use the drug despite personal and legal difficulties.
Physical dependence is an adaptive state, occurring after prolonged use of a drug, in which discontinuation of the drug causes physical symptoms that are relieved by re-administering the same drug or a pharmacologically related drug.
Both types of dependence can lead to compulsive patterns of drug use where the user's lifestyle is focused on taking the drug.18
Addiction. Addiction is a medical condition involving serious psychological and physical changes from repeated heavy use of a substance. The symptoms of addiction are uncontrollable drug craving, seeking, and use that persists even in the face of negative consequences. It is a progressive illness that worsens over time if left untreated. Using drugs repeatedly over time changes brain structure and function in long lasting ways that can persist after drug use is stopped. The amount of a drug necessary to cause this change is different for everyone. It is postulated, however, that after a certain amount of the drug is consumed, the brain essentially switches from a normal state to an addicted state as if a switch in the brain was flipped.15
The American Society of Addiction Medicine (ASAM) defines the ABCDE of addiction.1
| A. | Inability to consistently Abstain |
| B. | Impairment in Behavioral control |
| C. | Craving or increased ‘hunger' for drugs or rewarding experiences |
| D. | Diminished recognition of significant problems with one's behaviors and interpersonal relationships; and |
| E. | A dysfunctional Emotional response |
Causative Factors or Etiology
The difference in susceptibility to addiction is considered to be related to genetic influences. Very few people are able to return to occasional use after becoming addicted. Patients with a substance use disorder often begin taking a substance to achieve a desirable pharmacologic effect. When the drug use is continued to relieve personal problems or used as a coping mechanism, dependence may develop. When the individual becomes dependent on the drug, a genetically associated psychological mechanism leads to an alteration of the brain function. This is a feature of central nervous system (CNS) drugs that leads to addiction.
Genetic factors significantly contribute, approximately 50%, to the likelihood that an individual will develop an addiction. Environmental factors, cultural influences and resilient behaviors learned by the individual impact the extent to which genetic factors exert their influence.1
Other factors that may contribute to the genetic expression of addiction include:1
| • | Cognitive and affective distortions, which impair perceptions and compromise the ability to deal with feelings |
| • | Disruption of healthy social supports and problems in interpersonal relationships |
| • | Exposure to trauma or stressors that overwhelm an individual's coping abilities |
| • | Distortion in meaning, purpose and values that guide attitudes, thinking and behavior |
| • | Distortions in a person's connection with self, with others and with the transcendent (also referred to as God or the Higher Power) |
| • | The presence of co-occurring psychiatric disorders |
Nicotine Use & Addiction
The U.S. Surgeon General's Report on Smoking and Health (1960s) was one of the first public documents linking smoking to increased risk of cardiac and vascular disease. More recent research ties tobacco use to cancers of the mouth, pharynx, esophagus, lung, pancreas, and bladder. Additional health risks include diabetes; respiratory disorders; premature, low birth-weight infants or spontaneous abortions and periodontal disease. More recently, we have learned that those exposed to secondary smoke from tobacco products are at greater risk for these same conditions (Figure 1).
According to the 2013 National Survey on Drug Use and Health, an estimated 66.9 million Americans (25.5% of the population) aged 12 or older reported current use of tobacco. Specifically, 55.8 million (21.3% of the population) are cigarette smokers, 12.4 million (4.7%) smoke cigars, 8.8 million (3.4%) use smokeless tobacco, and 2.3 million (0.9%) smoke pipes, confirming tobacco is still one of the most widely abused substances in the United States.32,38
Forms of Nicotine Delivery
The following common forms of nicotine delivery will be discussed:
| • | Cigarettes |
| • | Cigars |
| • | Chewing Tobacco/Snuff |
| • | Electronic Nicotine Delivery Systems |
Cigarettes
There are more than 4,000 chemicals found in the smoke of tobacco products. The cigarette is a very efficient and highly engineered drug delivery system. By inhaling tobacco smoke, the average smoker takes in 1-2 milligrams of nicotine (the chemical that causes addiction) per cigarette. Thus, a person who smokes about 1 1⁄2 packs (30 cigarettes) daily takes at least 300 mg "hits" of nicotine to the brain each day. Immediately after exposure to nicotine, there is a "kick" caused in part by the drug's stimulation of the adrenal glands and the resulting discharge of epinephrine (adrenaline). The rush of adrenaline stimulates the body and causes an increase in blood pressure, respiration, and heart rate.
Smokers have access to numerous media and educational messages, which state that tobacco products are unhealthy. Many nicotine-addicted patients want to quit or have attempted to quit. Why is it so hard to quit a habit a person knows may kill them? As with many addictive drugs, it is believed that nicotine affects the release of dopamine into the brain. Dopamine fuels sensations of pleasure and relaxation. Over time, nicotine becomes something a person's body needs. In other words, after using nicotine for an extended period, the body becomes addicted to the substance. Both mind and body feel a need for the drug and its continued use. Cigarette smoking produces a rapid distribution of nicotine to the brain, peaking within 10 seconds of inhalation. However, the acute effects dissipate quickly, as does the feeling of euphoria, which causes the smoker to continue dosing to maintain the drug's pleasurable effects and prevent withdrawal.
Nicotine withdrawal symptoms include irritability, craving, depression, anxiety, cognitive and attention deficit, sleep disturbances, and increased appetite. These symptoms may begin within a few hours after the last cigarette, quickly driving people back to tobacco use. Symptoms peak within the first few days of smoking cessation and usually subside within a few weeks. For some people, however, symptoms may persist for months. Of the 35 million smokers who desire to quit smoking each year, more than 85% of those who attempt cessation relapse, most within 1 week.
Withdrawal is difficult due to the many physical and behavioral effects related to smoking. Symptoms of withdrawal can be severe. For some smokers, the feel, smell, and sight of a cigarette and the ritual of obtaining, handling, lighting, and smoking the cigarette are all associated with the pleasurable effects of smoking and can make cravings worse. Nicotine replacement therapies such as gum, patches, and inhalers may help alleviate the pharmacological aspects of withdrawal, however, cravings often persist. Behavioral therapies can help smokers identify environmental triggers of craving so they can employ strategies to prevent or circumvent these symptoms and urges.32
Cigars
In 2013, 4.7% of the American population smoked cigars. Cigars are addictive even if the smoke is not being inhaled. High levels of nicotine can still be absorbed into the body. A cigar smoker can get nicotine by two routes: by inhalation into the lungs and by absorption through the oral mucosa. Either way, the smoker becomes addicted to nicotine. A single cigar can potentially provide as much nicotine as a pack of cigarettes.
Most cigars are composed primarily of a single type of tobacco (air-cured and fermented), with a tobacco wrapper. Cigar smoke is possibly more toxic than cigarette smoke. Cigar smoke has a higher level of cancer-causing substances which originate from the fermentation process of the cigar manufacturing. Nitrosamines are found at higher levels in cigar smoke than in cigarette smoke. Cigar wrappers also have higher concentrations of toxins when compared to cigarettes. Furthermore, many cigars are larger resulting in a longer smoking time and higher exposure to many toxic substances including carbon monoxide, hydrocarbons, ammonia, and cadmium.
Cigar smoking has been linked to cancer of the oral cavity, larynx, esophagus, and lung. It may also cause cancer of the pancreas. Although cigar smokers have lower rates of lung cancer, coronary heart disease, and lung disease than cigarette smokers, they have higher rates of these diseases than those who do not smoke cigars. All cigar and cigarette smokers, whether or not they inhale, directly expose their lips, mouth, tongue, throat, larynx and lungs to smoke and its toxic, cancer-causing chemicals. In addition, when saliva containing the chemicals in tobacco smoke is swallowed, the esophagus is exposed to carcinogens. These exposures most likely account for the similar oral and esophageal cancer risks seen among cigar and cigarette smokers.24
Oral Implications of Cigarettes & Cigar Use/Abuse
Various oral conditions result from chronic smoking. Among them are:
Black Hairy Tongue: Elongated; black, brown, yellow or white papillae form in response to the solid and gaseous wastes of tobacco being trapped on the tongue's surface. Slowed cell sloughing adds to this syndrome. Food and bacteria may be trapped in the papillae and cause halitosis.
Stain & Calculus: While saliva flow is generally reduced in chronic smokers, the act of smoking stimulates serous saliva flow. This can increase calculus production. Stain is generally present. The combination of stain and calculus may compromise the periodontal health of most smokers.
Gingival and Periodontal Diseases: Conditions such as necrotizing ulcerative gingivitis (NUG) is prevalent in smokers. Scientific evidence clearly shows smokers have more severe periodontal diseases than do non-smokers. Continued smoking is likely to compromise the success of periodontal therapy. More refractory periodontal patients are smokers (90%) when compared to the general population (25%).
Additional Oral Changes: Smokers may also experience candidiasis, nicotine stomatitis, smoker's keratosis, pigmentation changes, and xerostomia (Figure 2).
Root Canals: 28-year study showed cigarette smokers are 70% more likely to need root canal therapy than non-smokers. Smoking impairs the body's response to infection, exacerbates bone loss throughout the skeleton, induces a chronic systemic inflammatory response, and causes vascular problems. Any of these pathways can potentially affect the health of the tooth pulp and surrounding bone tissue.21
Sinusitis: The incidence of acute or chronic inflammation of the nasal lining of both the maxillary and frontal sinuses occurs 75% more often among smokers than non-smokers. This may be attributed to the chemical compounds in the tobacco.
Ability to Heal: Nicotine is a vasoconstrictor and reduces blood flow to the tissues, causing delayed wound healing, especially in the mouth where smoke lingers. Dry sockets are four times more prevalent among smokers. Typically, dry sockets occur when the addicted smoker returns to their habit too soon after an oral surgery, disrupting the delicate clot in a postoperative extraction socket.
Leukoplakia: A precancerous lesion of the oral soft tissue that consists of a white patch or plaque that cannot be scraped off (Figure 3). It is often associated with tobacco use. It can persist in an area with no pain or irritation. These areas can develop into more serious lesions and should be examined carefully during a meticulous oral evaluation. Some leukoplakia will regress if tobacco use is discontinued.
Squamous Cell Carcinoma: This is the most common oral cancer linked to cigarette smokers and can occur anywhere in the mouth. It is most commonly found on the lateral borders of the tongue, the ventral surface of the tongue or floor of the mouth. Squamous cell carcinoma has a favorable prognosis if it is detected within two years of onset. If not detected early, approximately 50% will die as a direct result of the cancer or complications (Figure 4).
Other Cancers: Cigarette smoking harms nearly every organ in the body. It has been conclusively linked to cancers of the mouth, pharynx, larynx, esophagus, lung, stomach, pancreas, cervix, kidney, and bladder, as well as acute myeloid leukemia. Tobacco related cancer accounts for about one-third of all cancer deaths. The overall rates of death from cancer are twice as high among smokers as non-smokers, with heavy smokers having rates that are four times greater than those of non-smokers. Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 90% of all cases of lung cancer, the number one cause of cancer deaths among both men and women.
Chewing Tobacco/Snuff
Chewing tobacco, (dip, snus or snuff) is ground up tobacco, placed and held in the vestibule and chewed, not smoked. Nicotine is absorbed through the oral mucosa and into the bloodstream. Because of this rapid absorption, it is much harder for the snuff chewer to quit when compared to the smoker.
There are several forms:
| • | Chewing tobacco consists of loose tobacco leaves, sweetened and packaged in pouches. It is also called chew or chaw. A "wad" of the tobacco is placed between the cheek and gum to hold it in place, sometimes for hours at a time. Usually the tobacco juices are spit out, but in the more addicted, there is a tendency to swallow some of the juices. |
| • | Plug. This is chewing tobacco that has been pressed into a brick shape, often with the help of syrup, such as molasses, which also sweetens the tobacco. A piece is cut off or bitten off of the plug and held it between the cheek and gum. Tobacco juices are spit out. |
| • | Twist. This is flavored chewing tobacco that has been braided and twisted into rope-like strands. Twist is held between the cheek and gum, tobacco juices are expectorated as nicotine is absorbed. |
| • | Snuff. This is finely ground or shredded tobacco leaves. It is available in dry or moist forms and is packaged in tins or tea bag-like pouches. A pinch of snuff is placed between the lower lip and gum or cheek and gum. Dry forms of snuff can be sniffed into the nose. Using snuff is also called dipping. |
| • | Snus. Snus (pronounced snoos) is a newer smokeless, spitless tobacco product that originated in Sweden. It comes in a pouch that is placed between the upper lip and gum. It is left in place for less time, about a half-hour without having to spit, then is discarded. |
| • | Dissolvable tobacco products. These are pieces of compressed powdered tobacco, similar to small hard candies. They dissolve in the mouth, requiring no spitting of tobacco juices. They are sometimes called tobacco lozenge, but they are not the same as the nicotine lozenges or gum used to help one quit smoking.13 |
In 2013, 3.4% of Americans used chewing tobacco regularly. In 2015, nearly 2 of every 100 middle school students (1.8%) and 6 of every 100 high school students (6.0%) reported current use of smokeless tobacco.8,40
Oral Implications of Chewing Tobacco Use/Abuse
The use of smokeless tobacco products poses oral health risks. The more common manifestations are discussed below:
Leukoplakia: These can lead to aggressive oral cancers if left unchecked. The lesion pictured below (Figure 5) is a very early lesion with a rather thin coating of leukoplakia which should resolve with cessation of snuff use.
Verrucous Carcinoma: The longer snuff is used, the thicker and whiter the leukoplakia becomes and the more likely the lesion is to transform into an aggressive form of squamous cell carcinoma known as verrucous carcinoma. In most cases, cessation of the habit prior to the development of the cancer results in the disappearance of the lesion and a return to normal mucosa.35
Periodontal Disease: When tobacco products are held in the mouth, patients may have less time to perform daily oral hygiene, allowing bacteria to flourish. Typically, bleeding is an indicator of gingival inflammation. With nicotine use and abuse, vasoconstriction in oral tissues can lead to reduced bleeding upon probing which may give a false clinical indication. Keep this in mind while probing the sulcus of smokers.
Dental Caries: If the user chooses a tobacco product flavored or sweetened with a fermentable carbohydrate, there is an increase in caries, especially near the placement site.
Gingival Recession: Due to the irritating nature of the tobacco itself as well as the toxic chemicals released, there is a higher incidence of recession, especially adjacent to the placement site (Figure 6).
Other Implications
Smokeless tobacco contains approximately 28 carcinogens. It has been linked to reproductive health problems including reduced sperm count and abnormal sperm cells. Women who use smokeless tobacco during pregnancy are at an increased risk for preeclampsia, a condition that may include high blood pressure, fluid retention, and swelling; premature birth, and low birth weight babies.
Electronic Nicotine Delivery Systems
Electronic nicotine delivery systems (ENDS) heat a liquid, which typically contains nicotine, to an aerosol that is inhaled.16 ENDS include vaporizers, vape pens, hookah pens, e-pipes and e-cigarettes. The increase in use of ENDS by youth is more rapid than in adults. National surveys indicate that 5% of adults use ENDS compared to 16% of high school students. Of further concern are reports that the use of ENDS among high school students in 2011 was 1.5% but increased to 16% by 2015.16 These data demonstrating an increase in ENDS use is partially the result of the user's belief that these products are less harmful than other tobacco products. The CDC has issued statements that these products are not less harmful. Evidence to support ENDS as a tobacco cessation aid is limited and of low quality. As a result, ENDS are not an FDA-approved cessation aid.
Oral Implications of ENDS Use
There is still little documented evidence regarding the oral effects of ENDS use. Some studies show patients report mouth irritation; sore throat and dry mouth; and mouth ulcers. It is well documented that smoking, tobacco and nicotine have many health risks. More research is needed and the dental professional should be aware of emerging research.
Dental Clinician/Patient Communication Regarding Nicotine Use
Patients look to dental professionals for cessation assistance, but their addiction and enjoyment of tobacco far outweigh the best intentions of a caring clinician. We must be mindful that our efforts to educate do not come across as judgment or lecture. We must consider any existing oral conditions that may cause harm to the patient. For suggestions on how to approach your patients who smoke about smoking cessation options, the following websites may provide helpful information:
| • | FDA.gov |
| • | CDC.gov |
| • | Smokefree.gov |
Preventive oral cancer screenings are an annual standard of care. Documentation of such exams should also be standard procedure in all hygiene recare protocols. Use of early detection oral cancer techniques and products may be helpful. They include: visible light fluorescent wands that excite certain atypical compounds in the tissues, toluidine blue staining, vital staining, and DNA-evaluation and saliva-based oral cancer diagnosis. Brush and scalpel biopsies are the most effective.23
Smoking will reduce both mucous and serous saliva production. With compromised salivary flow and the effects of nicotine on the body, calcium uptake to teeth via saliva may also be inhibited in both smokers and chewing tobacco users. Educating the patient about the benefits of in-office and home therapeutic doses of calcium-phosphate fluoride varnishes and toothpastes will help to protect tobacco users and abusers from new or recurrent decay. A caries assessment evaluation is now considered the standard of care by the American Dental Association and should be incorporated into dental appointment protocols for patients with substance use disorders. (Figure 7). Assessing the patient's lifestyle and habits with regard to their risk for decay and need for therapeutic doses of calcium phosphate fluoride varnishes and toothpastes is essential. There are various sources of additional information on varnish and toothpastes protocols for review.
It is important for the clinician to have resources for patients interested in smoking cessation. Since smoking and tobacco use affects so many patients' health worldwide, a failure to suggest smoking cessation options and opportunities may not only affect your patients' oral health, but may affect their lifespan as well. The US Preventive Services Task Force recommends the Five A's and Refer Model.2,14 More information on this model can be found at: USPreventiveServicesTaskForce.org
Quit lines are telephone-based tobacco cessation services. Most are accessed through a toll-free number and provide callers with services including educational materials, referral to formal cessation programs and individualized telephone counseling. They are a significant resource universally available to dental clinicians. Evidence has revealed that quit lines are convenient, effective and preferred by smokers.18
Of current smokers who visited a physician, 50.7% were advised to quit. Of current smokers who visited a dental healthcare provider, 11.8% were advised to quit. Of all smokers who reported receiving advice to quit smoking, more than 90% reported receiving the advice from a physician, whereas only 13.5% reported receiving such advice from a dental healthcare provider.9 These data indicate there is room to improve the rates at which any health care provider offers tobacco/nicotine cessation information.
Quitting smokeless tobacco may cause short-term problems, especially for those who have used heavily for many years. These temporary changes can result in nicotine withdrawal symptoms that include cravings, anger/irritability, anxiety, depression or weight gain. Tobacco cessation programs for chew users need to be carefully supported. Many times health education via photographs and the invasive nature of oral cancers surgeries are enough to motivate the user to quit. There are many resources to support smokeless tobacco cessation including the Guide to Quitting Smokeless Tobacco from the American Cancer Society. In addition, the following are suggested to assist in living a dip-free lifestyle:
| • | Limited contact with other dippers, especially in the early weeks of quitting. |
| • | Do not buy, carry, or hold dip cans for others. |
| • | Do not let people dip in your home. Post a small "No Tobacco" sign by your front door. |
| • | Ask others to help you remain tobacco-free. Give them specific examples of things that are helpful (such as not dipping around you) and things that are not helpful (like asking you to buy chew for them). |
| • | Focus on what is personally gained by quitting: health, saving money, extended lifespan, quality of life, improved hygiene.13 |
Alcohol Use & Addiction
In 2013, 52.2% of Americans age 12 and older had used alcohol at least once in the 30 days prior to being surveyed; 22.9% had binged (5+ drinks within 2 hours); and 6.3% drank heavily (5+ drinks on 5+ occasions). In the 12-17 age range, 11.6% had consumed at least one drink in the 30 days prior to being surveyed; 6.2% had binged; and 1.2% drank heavily.38
Ethyl alcohol, or ethanol, is the intoxicating ingredient found in beer, wine, and liquor. Alcohol is produced by the fermentation of yeast, sugars, and starches. It is a central nervous system depressant that is rapidly absorbed from the stomach and small intestine into the bloodstream. A standard drink (12 ounces of beer, 8 ounces of malt liquor, 5 ounces of wine, or 1.5 ounces [a "shot"] of 80-proof distilled spirits or liquor [gin, rum, vodka, or whiskey]) contains 0.6 ounces of pure ethanol.
Alcohol affects every organ in the body as well as damages a developing fetus. Intoxication can impair brain function and motor skills; heavy use can increase risk of certain cancers, stroke, and liver disease. Alcoholism or alcohol dependence is a diagnosable disease characterized by a strong craving for alcohol, and/or continued use despite harm or personal injury. Alcohol abuse, which can lead to alcoholism, is a pattern of drinking that results in harm to one's health, interpersonal relationships, or ability to work.25 The National Institutes of Health reports 15% of the people living in the United States are considered "problem drinkers." Within this population, 5%-10% of the men and 3%-5% of the women could be labeled as alcoholics (Table 1).
Oral Implications of Alcohol Use/Abuse
Excessive Bleeding or Bleeding Disorders: Excessive alcohol use may damage the liver and bone marrow resulting in excessive bleeding during dental treatment. If excessive bleeding is observed, treatment should be stopped and digital pressure applied. Referral for medical evaluation and necessary blood coagulation tests should be requested before treatment progresses.
Effectiveness of Drugs: The drugs used in dentistry that are metabolized in the liver include amide local anesthetics and benzodiazepines. These drugs can have a reduced effect in the alcohol abusive patient. They can metabolize faster as compared to a routine patient. Dental anesthetics may not work as well at the injection site in the alcohol abuser and may be carried into the bloodstream more rapidly. Repeated doses may need to be reduced, or the interval between doses prolonged, to prevent excessive blood levels.18
Periodontal Disease: Several biological explanations exist for the detrimental effect that alcohol may have on the periodontium. Studies have shown neutrophilic phagocytosis is associated with periodontal disease. Alcohol also impairs neutrophil function, contributing to bacterial overgrowth which may lead to periodontal inflammation. Additionally, alcohol may have a direct toxic effect on periodontal tissue. Finally, high alcohol intake increases monocyte production of inflammatory cytokines (tumor necrosis factor-alpha (TNF-∂), interleukins-1 and 6), in the gingival crevice which is associated with periodontitis.33
Oral Cancer: Drinking alcohol has been associated with oral cancer. Evidence suggests that this is because alcohol breaks down into acetaldehyde, which can bind to the proteins in the oral cavity. This can trigger an inflammatory response in the body. In the most severe cases, cancerous cells can develop. Oral cancer most often appears on the lips or tongue but can occur under the tongue, on the palate or on the gingiva.42 An oral cancer screening should be performed at each dental exam.
Dental Caries: Heavy drinkers may experience dry mouth at night and neglect both personal and professional oral health care. They may also consume higher levels of refined carbohydrates to satisfy their "munchies." Heavy drinking can also lead to frequent vomiting and the vomit is extremely acidic. All of these might increase their risk of developing dental caries.42
Xerostomia: Because alcohol will dehydrate the patient, their salivary flow may be compromised. An enlargement of the parotid salivary glands may be a sign of a chronic alcohol use problem.42 Educating the patient about the benefits of in-office and home therapeutic doses of calcium-phosphate fluoride varnishes and toothpastes will help to protect these patients from new or recurrent decay. Have the patient do a Caries Assessment Evaluation to discover their proper protocol for varnish and toothpaste regimens (Figure 7).
Blood Pressure: When treating an alcohol dependent patient, the clinician should consider the possibility of increased blood pressure and monitor vital signs at each appointment.
Dental Clinician/Patient Communication Regarding Alcohol Use
Patients may not openly admit they have an alcohol problem. Many times this is omitted from a medical history and only occasionally will it come up in conversation if a patient is seeking help or guidance. The dental clinician must be competent at recognizing signs, especially if a patient is "under the influence." Use the senses: the smell of alcohol on breath or the odor of alcohol upon opening the bloodstream during scaling; the patient has a red face or bloodshot eyes; has hypertrophy of parotid glands; exhibits slurred speech; or demonstrates impaired or inappropriate behavior.
When alcohol abuse is suspected in the dental patient, management depends on whether or not the patient is intoxicated, shows signs of alcohol abuse or reports a substance use disorder on the health history. A patient who comes to the appointment in an inebriated state should be rescheduled and accompanied to their home by a responsible person. This can become a delicate situation for which the dental office would become liable if they were to treat this patient by administering injectable/topical anesthetics or performing scaling which could induce prolonged bleeding. Some dental offices now keep an alcohol breathalyzer on hand to test the patient's blood alcohol levels to determine if treatment is contraindicated. Protocols for dealing with patients suspected of being under the influence of alcohol should be established in the office. The office personnel may consider testing the patient's blood alcohol levels, having the patient sign-off to have or not have treatment, gently suggesting the appointment be rescheduled for another day or dismissing the patient.
Patients with signs of oral-related pathology should be educated about oral cancers and conditions that can persist and may be related to alcohol consumption. Many patients withhold from their medical history and patient interview an accurate picture of the amount of alcohol or drug use. Providing an overview of associated lifestyle habits can infer to the patient's inherent risks of alcohol indulgence without getting invasive or too personal. Proper documentation of clinical findings and suspected lifestyle should be documented in the patient's chart for future reference.
If an alcohol dependent patient presents for dental treatment and wants to discuss their current dependency, it is important to provide a safe, accepting environment in which to deliberate. Having support materials on hand within your dental office from a resource such as Alcoholics Anonymous (AA) can provide a tie to that support system without the patient having to do research themselves. Keeping a printed list (or marking it in your web browser) is another convenient means to help an alcohol dependent patient seek help. Placing brochures or AA meeting lists inside the oral hygiene take-home bags will keep this information discrete. Make sure the patient approves of the information before providing it as a take along (Figure 8).
Prescription Medication Use & Addiction
Prescription drug abuse is the intentional use of a medication without a prescription, in a way other than as prescribed, or for the experience or feeling it causes (for the "high"). It is a problem that deserves attention, especially from healthcare professionals. While prescription drugs can be powerful healing tools, they also pose serious health risks related to their abuse.31
In 2013, 6.5 million Americans aged 12 or older (2.5%) had used prescription drugs nonmedically in the past month.30 Additionally, there were approximately 2 million persons aged 12 or older who used psychotherapeutics nonmedically for the first time within the past year, which averages to approximately 5,500 initiates per day.38 The classes of prescription drugs most commonly abused are: opioid pain relievers, such as Vicodin® or OxyContin®; stimulants for treating Attention Deficit Hyperactivity Disorder (ADHD), such as Adderall®, Concerta®, or Ritalin®; and central nervous system (CNS) depressants for relieving anxiety, such as Valium® or Xanax®.1
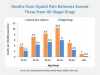
Prescription (Rx) and over-the-counter (OTC) medications account for most of the commonly abused drugs by high school seniors (Figure 9). After alcohol and marijuana, Rx and OTC medications are the most commonly abused substances by Americans age 14 and older. When asked how prescription narcotics were obtained for nonmedical use, 70% of 12th graders said they were given to them by a friend or relative.31
There are several factors that contribute to prescription drug abuse:
| • | Misperceptions about their safety. Because these medications are prescribed by doctors, many patients assume the medications are safe to take under any circumstances. This is not the case. Prescription drugs act directly or indirectly on the same brain systems affected by illicit drugs. Using a medication other than as prescribed can lead to a variety of adverse health effects including overdose, addiction or death. |
| • | Increasing availability. Between 1991 and 2010, prescriptions for stimulants increased from 5 million to nearly 45 million and for opioid analgesics from about 75.5 million to 209.5 million. |
| • | Motivations to abuse. Patients may use prescription drugs to get high; to counter anxiety, pain, or sleep problems; or to enhance cognition. Whatever the motivation, prescription drug abuse comes with serious risks.31 |
Commonly Abused Prescription Drugs
Opioids (used to treat pain): Prescription opioids act on the same receptors as heroin and can be highly addictive. People who abuse them sometimes alter the route of administration (e.g., snorting or injecting) to intensify the effects. Some even report moving from prescription opioids to heroin. It is estimated that approximately 1.9 million people in the U.S. meet the abuse or dependence criteria for prescription opioids. Abuse of opioids, either alone or with alcohol or other drugs, can depress respiration or lead to death. Unintentional overdose deaths involving prescription opioids have quadrupled since 1999 and now outnumber those from all other drugs combined, including heroin and cocaine. (Figure 10). Injecting opioids increases the risk of HIV and other infectious diseases through use of unsterile or shared equipment. Non-injection drug use can also increase these risks through drug-altered judgment and decision making.
While hydrocodone and oxycodone may be most familiar as the opioid analgesics commonly abused, there are two more about which the dental healthcare provider should be aware: fentanyl, a synthetic opiate and carfentanil, a derivative of fentanyl. Fentanyl is a powerful analgesic similar to morphine but 50 to 100 times more powerful. The legitimate use of fentanyl is generally limited to end-of-life pain management. Since 2013, law enforcement encounters (drugs submitted for analysis) testing positive for fentanyl have sharply increased.7 In 2013, zero states reported more than 500 encounters; in 2014 two states and in 2015 eight states reported more than 500 encounters. The total number of encounters has more than doubled in the U.S. from 5,343 in 2014 to 13,882 in 2015. States like New Hampshire and Ohio are noting rapid increases in encounters.7 These increases are primarily due to illicitly made fentanyl that is being mixed with or sold as heroin, with or without the users' knowledge. Carfentanil is 100 times stronger than fentanyl. Due to this extreme strength, the legitimate use of carfentanil is limited to elephant and other large animal sedation. Veterinarians licensed to use carfentanil cover their hands, arms and faces to protect them from contact, and keep an antidote close by. Carfentanil is illegally obtained by diverting legal veterinarian supplies or synthesized in street labs.41
CNS Depressants (used to treat anxiety and sleep problems): These drugs are addictive and, in chronic users or abusers, discontinuing them without a physician's supervision can bring about severe withdrawal symptoms, including seizures, which can be life-threatening.
Stimulants (used to treat ADHD and narcolepsy): Misuse of stimulants can causeaddiction and other health consequences. These include psychosis, seizures, and cardiovascular complications.31
Oral Implications of Prescription Medication Use/Abuse
Oral implications of prescription medication use and abuse are vast depending on the specific drug being used/abused. Common implications include xerostomia, clenching/grinding, caries and periodontal disease. A routine, thorough oral exam is recommended. Identifying the particular prescription drug will reveal more complete oral implications.
Identifying the Prescription Drug Abuser
The dental office can be a target for a prescription drug abuser as they may be seeking prescriptions from the office. Paying special attention to medications listed on the medical history may not be sufficient for the patient suspected of abusing prescription drugs as the patient may downplay their use of substances in order to obtain new prescriptions. A key indicator that a patient may be "prescription seeking" is if they skillfully ask for drugs by name, dosage and number of tablets. This should alert a clinician to investigate further. One can call local pharmacies or look up statewide databases which track doctors' prescription-writing, pharmacy prescription-dispensing, and patients' prescription filling activities (Figure 11).
Illegal Drug Use & Addiction
The National Survey on Drug Use and Health (NSDUH) obtains information on illicit drug use by surveying the following categories: marijuana/hashish, cocaine/crack, heroin, hallucinogens, and inhalants. Several drugs are grouped under the hallucinogens category including lysergic acid diethylamide (LSD), phencyclidine (PCP), peyote, mescaline, psilocybin mushrooms, and Ecstasy (MDMA). Inhalants include a variety of substances such as nitrous oxide, amyl nitrite, cleaning fluids, gasoline, spray paint, other aerosol sprays, and glue.
Estimates of illicit drug use reported by the NSDUH reflect the use of any of the drug categories listed above. In 2013, an estimated 24.6 million Americans aged 12 or older were current illicit drug users, meaning they had used an illicit drug during the month prior to the survey interview. This estimate represents 9.4% of the population aged 12 or older (Figure 12).37,38
Four Common Illicit Drug Addictions
The following common illicit drug addictions will be discussed:
| • | Marijuana |
| • | Methamphetamine |
| • | Cocaine |
| • | Heroin |
Marijuana
Cannabis (marijuana, hashish, and hash oil) is also known as weed, pot, reefer, joint, Mary Jane, ganja, grass, sinsemilla, and dope. Additionally, blunts are cigars emptied of some tobacco and refilled with marijuana. Marijuana has been described as the most commonly used illegal drug in the United States. In 2013, there were 19.8 million current users aged 12 and older, up from 14.5 million users in 2007.30 Marijuana laws are changing and may result in an increase in use. As of January 2017, eight states (Alaska, California, Colorado, Maine, Massachusetts, Nevada, Oregon and Washington) and the District of Columbia allow the recreational use of marijuana.3,36 An additional 21 states allow for the use of medical marijuana. To view a map of marijuana legalization status, visit www.governing.com
Marijuana increases dopamine, which creates the euphoria or "high" associated with its use. A user may feel the urge to smoke marijuana again and again to re-create that experience. Repeated use could lead to addiction - a disease where people continue to do something, even when they are aware of the severe negative consequences at the personal, social, academic, and professional levels.
Cannabis may be smoked as a cigarette or in a pipe, as well as added to foods. A favorite way to use marijuana is through a "bong" in which the smoke is drawn through a layer of water that cools the smoke and removes some of the tar and irritants.
When marijuana is smoked, tetrahydrocannabinol (THC) rapidly passes from the lungs into the bloodstream, which carries the chemical to the brain and other organs throughout the body.
Contrary to common belief, marijuana is addictive. Estimates from research suggest that about 9% of users become addicted to marijuana; this number increases to 17% among those who start young. People who use marijuana may also experience a withdrawal syndrome when they stop using the drug. This withdrawal is similar to what happens to tobacco smokers when they quit - people report being irritable, having sleep problems, and loosing weight, which can last for several days to a few weeks after drug use is stopped. Relapse is common during this period, as users also crave the drug to relieve these symptoms.28
Oral Implications of Marijuana Use/Abuse
Periodontal Disease: Smoking marijuana may contribute to periodontal disease in a way similar to tobacco smoking. A recent study of individuals who reported smoking cannabis at 18, 21, 26 and 32 years of age in New Zealand investigated the relationship between marijuana and oral health. When measurements of oral health between ages 26 and 32 in the group reporting high cannabis use were compared, there were 23.6% more sites with clinical attachment loss compared with 11.2% in the 26 year old group. After controlling for tobacco smoking, the authors concluded that cannabis smoking may be a risk factor for periodontal disease that is independent of the use of tobacco.39
Xerostomia: Heavy use of marijuana may cause xerostomia in the mouth and dryness in the throat, irritation of oral tissues, edema, and erythema of the uvula. As an added detriment, the xerostomia may increase the caries rate.14
Tissue Changes: The high temperature of the burning product on the oral tissues causes some tissue change and cellular disruption. Additionally, oral leukoplakia/erythroplakia, leukoedema and hyperkeratotic lesions have been documented. Candida has been reported to be higher in marijuana users compared with tobacco users.5
Other Implications
In addition to oral effects, cannabis smoking has been implicated in cardiovascular disease. A recent systematic review reports atrial fibrillation, increased heart rate, and a risk for postural hypotension in healthy men who used marijuana.20 In older adults cardiovascular changes led to angina attacks from lack of oxygenated blood in cardiac muscle.18 For more information about the oral implications of marijuana, please see the following course on dentalcare.com: Marijuana Use and Oral Health
Methamphetamine
Methamphetamine (meth) abuse has increased significantly as documented in the National Survey on Drug Use and Health reports. Between 2002 and 2004, the percentage of meth users who were dependent on the drug increased from 27.5% to 59.3%. It is estimated there are 12.3 million Americans over the age of 12 who have used the drug at least once, with the majority of users between ages 18-34 years. In 2013, there were 595,000 current users of meth compared to 353,000 in 2010.30 Meth can be made from inexpensive medications or simple over-the-counter chemicals (lye, muriatic and sulfuric acids) that are easily obtained at stores.34 Street names include Speed, Ice, Chalk, Crank and Crystal.
Meth is a highly addictive synthetic amine that stimulates the release and blocks the re-uptake of serotonin, dopamine and norepinephrine in the brain. The action of these neurotransmitting monoamines is to stimulate the reward centers of the brain and give the characteristic "high" of the substance. Lack of appetite frequently accompanies this drug's effect. The high can last 14 hours. During the high, the user is typically impaired and unable to care for themselves or others. Long-term use leads to depletion of these neurotransmitters, resulting in emotional depression.33
Oral Implications of Meth Use/Abuse
Dental Caries: Meth mouth, or crank decay, is commonly observed in methamphetamine users. The cause of meth mouth is multifactorial. Meth users commonly experience drug-induced cravings for high-calorie carbonated beverages. As a result, soft drinks containing high amounts of sugar and caffeine are often consumed to prolong the high and assuage the cravings. Reports indicate that Mountain Dew™ is commonly ingested by meth users; as much as several liters per day. The drug produces extreme xerostomia, reducing the amount of protective saliva and buffering capacity around the teeth. As a result of these behaviors, the oral bacterial levels can drastically increase, exacerbating the decay. The caustic nature of the drug, poor oral care and high sugar diet result in increased decay. This devastation can occur rapidly in as little as one year. Conventional dental treatment is frequently of little value. Often, the caries are so significant and rampant that full-mouth extractions are indicated (Figure 13).
Periodontal Disease: Methamphetamine users have an increased incidence of periodontal disease. The drug causes vasoconstriction of the vessels that supply blood to the oral tissues. With repeated use of the drug and repeated vasoconstriction, the blood vessels are permanently damaged and the oral tissues die. In addition, lack of proper daily oral hygiene further exacerbates the declining periodontal health.
Bruxism: Methamphetamine can cause users to feel anxious and nervous, resulting in clenching and grinding of the teeth. Signs of bruxism, including fractures of the teeth and severe attrition, are common. The vasoconstriction can also affect the vitality of the teeth, increasing the likelihood of enamel fractures.
Oral Ulcers and Infection: Oral ulcerations and infections are common among methamphetamine users. When smoked or snorted, the caustic ingredients of the drug bathe the oral cavity and irritate and burn the oral tissues. This leads to significant oral ulcerations and infections. This is also brought on by the severe dry mouth that accompanies the use of meth. Xerostomia is caused by the vasoconstriction and reduction of salivary gland function. The tongue and lining of the mouth can become raw and irritated without the surfactant action of saliva. This can lead to secondary infections and limited ability to speak and eat.17
Local Anesthesia and Sedation: The clinician must be sure the meth patient has not used several days prior to deep sedation and dental injections need to be closely monitored.
For more advanced clinical information about the oral implications of meth abuse, please see the following course on dentalcare.com: Methamphetamine: Implications for the Dental Team.
Cocaine
Cocaine is a powerfully addictive stimulant that directly affects the brain. Cocaine was labeled the drug of the 1980s and 1990s because of its extensive popularity and use during that period. However, cocaine is not a new drug. In fact, it is one of the oldest known psychoactive substances. Coca leaves, the source of cocaine, have been chewed and ingested for thousands of years, and the purified chemical, cocaine hydrochloride, has been an abused substance for over 100 years. In the early 1900s, for example, purified cocaine was the active ingredient in most of the tonics and elixirs that were developed to treat a wide variety of illnesses.
Cocaine is generally sold on the street as a fine, white, crystalline powder known as coke, C, snow, flake, or blow. Street dealers generally dilute it with inert substances such as cornstarch, talcum powder, sugar, or with active drugs such as procaine (a chemically related local anesthetic) or amphetamine (another stimulant). Some users combine cocaine with heroin - in what is termed a "speedball."
There are two chemical forms of cocaine that are abused: the water-soluble hydrochloride salt and the water-insoluble cocaine base (or freebase). When abused, the hydrochloride salt, or powdered form of cocaine, can be injected or snorted. The base form of cocaine has been processed with ammonia or sodium bicarbonate and water, and then heated to remove the hydrochloride to produce a substance that can be smoked. The term "crack," which is the street name given to freebase cocaine, refers to the crackling sound heard when the mixture is smoked.26
The National Survey on Drug Use and Health (NSDUH) estimates that in 2008, there were 1.9 million cocaine users and approximately 359,000 were current crack users.37 Cocaine use has declined slightly. In 2013, the number of current cocaine users was 1.5 million.30 Adults aged 18 to 25 years have a higher rate of current cocaine use than any other age group, with 1.5% of young adults reporting past month cocaine use. Overall, men report higher rates of current cocaine use than women.37
Users generally take cocaine in "binges," during which the cocaine is used repeatedly and at increasingly higher doses. This can lead to increased irritability, restlessness, panic attacks, and paranoia-even a full-blown psychosis, where the individual loses touch with reality and experiences auditory hallucinations. With increasing dosages or frequency of use, the risk of adverse psychological or physiological effects increases.26
Oral Implications of Cocaine Use/Abuse
Dental Caries: Cocaine users experience an increased rate of tooth decay for a variety of reasons: the drug contributes to xerostomia, the user does not seek regular professional care or perform regular personal oral care, and they may rub the drug directly onto the gingival tissue resulting in tooth erosion.
Gingival and Periodontal Diseases: Xerostomia and lack of routine oral hygiene care lead to an increased rate of periodontal diseases. Bruxing may also contribute to disease.
Bruxism and TMJ: Clenching and grinding contribute to the destruction of the supporting structures leading to cervical abrasion, occlusal wear and TMJ disorders.
Gingival Lesions: The user may rub the drug on the gingival tissue resulting in gingival lesions.
Nasal and Oropharynx: Regularly snorting cocaine can lead to loss of sense of smell, nosebleeds, problems with swallowing, hoarseness, and an overall irritation of the nasal septum, which could result in a chronically inflamed, runny nose.
Other Oral Effects: Other manifestations include oral candida infections, perforation of palate, bilateral cleft lip and palate in the fetus, angular cheilitis, halitosis, glossodynia, erosive lichen planus, corrosion of gold restorations, and excessive hemorrhage after tooth extraction.22,26 Cocaine users may exhibit buccolingual dyskinesia - a movement disorder characterized by protruding the tongue and pursing the mouth or lips - also known as ‘crack dancing' or boca torcida (twisted mouth).
Local Anesthesia: The administration of a local anesthetic with vasoconstrictors may result in an acute rise in blood pressure, which could lead to cardiac arrest. There is also a risk of convulsions associated with the combination of lidocaine and cocaine potentiates. Use of epinephrine-impregnated retraction cords is also contraindicated. It is advisable to postpone any dental treatment at least 6 to 24 hours after the use of cocaine.22
Heroin
Heroin is a powerful opioid drug made from morphine, a natural substance taken from the seed pod of the Asian opium poppy plant.27 Use of heroin produces euphoria and feelings of relaxation. Regular heroin use changes the functioning of the brain, causing tolerance and dependence. Heroin can be a white or brown powder, or a black sticky substance known as black tar heroin. Heroin can be pure or mixed with fillers or other drugs such as fentanyl. Other common names for heroin include dope, horse, junk, and smack.29
Heroin use has been increasing in recent years among both genders, most age groups and all income levels. Some of the greatest increases have occurred in demographic groups with historically low rates of heroin use: women, the privately insured and people with higher incomes. In particular, heroin use has more than doubled in the past decade among young adults aged 18-25 years. Heroin-related overdose deaths have more than quadrupled since 2010, with nearly 13,000 people dying in 2015. The rising rate of heroin use is attributed to increased availability, relatively low price (compared to prescription opioids) and high purity of heroin in the U.S.6,10 Past misuse of prescription opioids is the strongest risk factor for starting heroin use.6
Heroin can be injected, smoked or snorted.27 Because heroin is so rapid acting and users do not know the actual strength or purity of the drug, uses face a high risk of overdose or death.29
Oral Implications of Heroin Use/Abuse
Dental Caries: Heroin users have increased numbers of decayed, missing and filled teeth possibly the result of the drug contributing to cravings for sweet foods.12
Gingival and Periodontal Diseases: Heroin users demonstrate increased incidence of gingival and periodontal diseases as a result of the lack of personal and professional dental care.12
Other Oral Effects: Oral fungus, oral viral infections and discoloration of the tongue have been observed in heroin users. In addition, a 2012 study published the Journal of the American Dental Association found that the pattern of decay known as "meth mouth" was characteristic of intravenous heroin users as well.4
Dental Clinician/Patient Communication Regarding Illegal Drug Use
Patients may not admit they have a drug dependency. The dental clinician must be competent at recognizing signs, especially if a patient is "under the influence."
When abuse is suspected, management depends on whether or not the patient is high, shows signs of abuse or whether they are seeking help with a drug problem. As with alcohol, protocols for dealing with patients should be established in the office.
Patients with signs of oral-related pathology should be educated about the conditions. Proper documentation of clinical findings and suspected lifestyle should be included in the patient's chart.
If a drug dependent patient presents for dental treatment and chooses to discuss their current dependency, provide a safe, accepting environment for discussion. Having support materials on hand from a resource such as Narcotics Anonymous (NA) can provide a link to that support system.18 Further communication suggestions are available at Partnership for Drug-Free Kids and the National Institutes of Health's National Institute on Drug Abuse.
Conclusion
Substance use disorders are a national concern. The dental professional must be aware of the indications of substance use, have the knowledge to recognize and treat dental concerns, and provide the patient with cessation information.
References
1. American Society of Addiction Medicine (ASAM). Quality & Practice. Definition of Addiction. Accessed July 10, 2017.
2. Boyd LD. Tobacco Trends. Dimensions of Dental Hygiene. Feb 2017;15(2):50-53. Accessed July 10, 2017.
3. Bricken H. Medical vs. recreational marijuana in 2015. Posted in Colorado, Medical Marijuana, Oregon, Recreational Marijuana, Washington. January 5, 2015. Accessed July 10, 2017.
4. Brown C, Krishnan S, Hursh K, et al. Dental disease prevalence among methamphetamine and heroin users in an urban setting: a pilot study. J Am Dent Assoc. 2012 Sep;143(9):992-1001.
5. Burkhart NW. Marijuana. RDH. 2010:30(8). Accessed July 10, 2017.
6. Centers for Disease Control and Prevention. Heroin overdose data. What is Heroin? Accessed July 10, 2017.
7. Centers for Disease Control and Prevention. Reported Law Enforcement Encounters Testing Positive for Fentanyl Increase Across US. Accessed July 10, 2017.
8. Centers for Disease Control and Prevention. Youth and Tobacco Use. Accessed July 10, 2017.
9. Danesh D, Paskett ED, Ferketich AK. Disparities in receipt of advice to quit smoking from health care providers: 2010 National Health Interview Survey. Prev Chronic Dis. 2014 Jul 31;11:E131. doi: 10.5888/pcd11.140053.
10. Deadly drug overdoses more than double since 1999. The Cincinnati Enquirer. February 25, 2017.
11. DeNoon D. WebMD Survey: The Lies We Tell Our Doctors. MedicineNet.com. September. 21, 2004. Accessed July 10, 2017.
12. Hussain F, Frare RW, Berrios KL. Dental Management of Patients with a History of Substance Abuse with Special Consideration for Addicted Pregnant Women and Addicted Dental Care Providers. Oralhealth. March 21, 2003. Accessed July 10, 2017.
13. Ralston A. Chewing Tobacco Facts. Facts about Smokeless Tobacco. July 18, 2016. Accessed July 10, 2017.
14. Ditmyer MM, Demopoulos CA, Mobley C. Under the influence. Dimensions of Dental Hygiene. July 2013;11(7):40-44. Accessed July 10, 2017.
15. National Institute on Drug Abuse. Drugs, Brains and Behavior: The Science of Addiction. Drug Abuse and Addition. What is drug addiction? Accessed July 10, 2017.
16. US Food & Drug Administration. Tobacco Products. Vaporizers, E-cigarettes, and other Electronic Nicotine Delivery Systems (ENDS). Accessed July 10, 2017.
17. Frese PA, McClure EA. Methamphetamine: Implications for the Dental Team. dentalcare.com. Accessed July 10, 2017.
18. Frieda P. Substance Abuse: Considerations for the Oral Health Professional When the Client is Suspected to be Abusing Substances. Course developed for Tennessee Dental Hygienists' Association, August 2012. Accessed July 10, 2017.
19. Friedlander AH, Norman DC. Geriatric alcoholism: pathophysiology and dental implications. J Am Dent Assoc. 2006 Mar;137(3):330-8.
20. Korantzopoulos P, Liu T, Papaioannides D, et al. Atrial fibrillation and marijuana smoking. Int J Clin Pract. 2008 Feb;62(2):308-13. Epub 2007 Nov 21. doi: 10.1111/j.1742-1241.2007.01505.x.
21. Krall EA, Abreu Sosa C, Garcia C, et al. Cigarette smoking increases the risk of root canal treatment. J Dent Res. 2006 Apr;85(4):313-7. doi: 10.1177/154405910608500406.
22. Maloney W. The Significance of Illicit Drug Use to Dental Practice. Webmed Central Dentistry, Drug Abuse 2010;1(7):WMC00455. Accessed July 10, 2017.
23. Mehrotra R, Gupta DK. Exciting new advances in oral cancer diagnosis: avenues to early detection. Head Neck Oncol. 2011 Jul 28;3:33. doi: 10.1186/1758-3284-3-33.
24. National Cancer Institute. Fact Sheet, Cigar Smoking & Cancer. Accessed July 10, 2017.
25. National Institute on Drug Abuse. Advancing Addiction Science. Alcohol. Alcohol Use: Statistics & Trends, December 2011. Accessed July 10, 2017.
26. National Institute on Drug Abuse. Advancing Addiction Science. Cocaine: Abuse and Addiction, 2010. Accessed July 10, 2017.
27. National Institute on Drug Abuse. Advancing Addiction Science. Heroin. Accessed July 10, 2017.
28. National Institute on Drug Abuse. Advancing Addiction Science. Marijuana. Revised February 2017. Accessed July 10, 2017.
29. National Institute of Drug Abuse. Media Guide. The Science of Drug Abuse and Addiction: the Basics. Accessed July 10, 2017.
30. National Institute on Drug Abuse. Advancing Addiction Science. Nationwide Trends. Revised June 2015. Accessed July 10, 2017.
31. National Institute on Drug Abuse. Advancing Addiction Science. Prescription and Over-the-Counter Medications Revised November 2015. Accessed July 10, 2017.
32. US Department of Health and Human Services. National Institutes of Health. National Institute on Drug Abuse (NIDA). Research Report Series. Tobacco Addiction. What Are the Extent and Impact of Tobacco Use? Accessed July 10, 2017.
33. Pitiphat W, Merchant AT, Rimm EB, et al. Alcohol consumption increases periodontitis risk. J Dent Res. 2003 Jul;82(7):509-13. doi: 10.1177/154405910308200704.
34. Rees TD. Oral effects of drug abuse. Crit Rev Oral Biol Med. 1992;3(3):163-84.
35. Spiller MS. Oral Cancers: Snuff Pouch, 2009. Accessed July 10, 2017.
36. State Marijuana Laws in 2017 Map. Accessed July 10, 2017.
37. Substance Abuse and Mental Health Services Administration, Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings, NSDUH Series H-41, HHS Publication No. (SMA) 11-4658. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2011. Accessed July 10, 2017.
38. Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (September 4, 2014). The NSDUH Report: Substance Use and Mental Health Estimates from the 2013 National Survey on Drug Use and Health: Overview of Findings. Rockville, MD. Accessed July 10, 2017.
39. Thomson WM, Poulton R, Broadbent JM, et al. Cannabis smoking and periodontal disease among young adults. JAMA. 2008 Feb 6;299(5):525-31. doi: 10.1001/jama.299.5.525.
40. Centers for Disease Control (CDC). National Center for Health Sciences. Health, United States, 2015 - Individual Charts and Tables: Spreadsheet, PDF, and Power Point files. Table 51 (page 1 of 3). Use of selected substances in the past 30 days among 12th graders, 10th graders, and 8th graders, by sex and race: United States, selected years 1980-2014. Accessed July 10, 2017.
41. Warning: Elephant opioid hitting streets. The Cincinnati Enquirer. July 16, 2016. Accessed July 10, 2017.
42. Zaremski E. The more you booze, the more you lose - How alcohol affects teeth and the oral cavity. (2012). Accessed July 10, 2017.
Additional Resources
• American Council for Drug Education
• A Student's Guide to Recognizing Disorders, Seeking Help and Promoting Wellness
• Balancing Student Stress
• Centers for Disease Control and Prevention
• Community Anti-Drug Coalitions of America
• Council for Prevention of Alcohol and Substance Abuse
• Department of Health and Human Services
• Depression Guidebook for Students
• Freevibe.com (abovetheinfluence.com)
• Geriatric Mental Health Foundation: Substance Abuse and Misuse Among Older Adults
• Medicare Plans by State
• Methamphetamine Treatment Project
• Narconon International
• National Addiction Rehab Locator
• National Clearinghouse for Alcohol and Drug Info
• National Institute on Drug Abuse (NIDA)
• NIDA for Teens
• Office of Community Oriented Policing
• Ohio Parents for Drug Free Youth
• Ohio Department of Alcohol and Drug Addition
• Ohio Drug-Free Action Alliance Coalition against Meth
• Partnership for Drug-Free Kids
• Street Drugs
• Substance Abuse and Mental Health Services Administration
• Substance Abuse in College
• U.S. Drug Enforcement Administration
• Withdrawal.org
About the Authors
Patricia A. Frese, RDH, MEd
Patricia Frese is Professor Emerita of the University of Cincinnati Blue Ash College Cincinnati, Ohio. She has been in education since 1980. She is a 1976 graduate of the dental hygiene program at Raymond Walters College (now UC Blue Ash). She has private practice experience in general, research and periodontal practice settings. She has presented on a variety of topics at professional meetings. Pat is an active member of the American Dental Hygienists' Association.
Email: patricia.frese@uc.edu
Elizabeth McClure, RDH, MEd
Elizabeth (Biz) McClure is Professor of Dental Hygiene at the University of Cincinnati Blue Ash College, Cincinnati, Ohio, where she has taught since 1990. She graduated from the Raymond Walters College (now UC Blue Ash) dental hygiene program in 1984 and has worked in general practice and research. She is an active member of the American Dental Hygienists' Association. She has presented a variety of topics at professional meetings.
Email: mcclurea@uc.edu