You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
For digital implants, the key to success is a sound workflow supported by an involved team. As implant dentistry has shifted toward a more digital environment, focus has increased on full team collaboration, training in new diagnostic tools for treatment planning and restoring implants, and reconsideration of case presentations to be more effective. The best implementation of digital techniques requires simplification of how dentists organize their approach in the practice. Small changes in implant treatment strategies can make the practice run more efficiently. This article covers advancements in dental technology, ideal team dynamics, implant placement considerations, diagnostic data essentials, and guided implant surgery for case success.
Implant dentistry is becoming more prevalent, with more than 35 million Americans missing all teeth in one or both jaws. Of this total, only 3 million have implants, but the number is rising by about 500,000 a year. At this rate, in 6 years the amount of people with implants could at least double. Only about 10% of dentists in the United States place implants, yet this number is also growing to meet increased demand. The US and European market for dental implants is on track to hit $4.2 billion by the year 2022. Corresponding with this market growth is a consistent success rate of up to 98% for implants, which is unusually high for dental work such as restorations and bridges. This success can largely be attributed to digital processes.1
From Analog to Digital: Advancements in Dental Technology
In the past, analog tools such as a watch or calendar functioned tangibly and separately; today, they are frequently housed in one all-purpose digital device, such as a smartphone. Digital dentistry followed this same line of evolution. An example is the radiograph. Years ago, clinicians used a piece of lead to block radiation. The first digital advancement for radiographs was the daylight loader, which saved a large amount of time in a process that previously took 20 to 30 minutes.The second advancement was replacing radiograph film with a digital radiograph. Clinicians can take a volumetric digital image-cone-beam computed tomography (CBCT)—in 6 seconds or less.
Another area of dentistry that has seen significant advancement is the impression. Patients tend to dislike the impression "goop" that gets placed in their mouths; there is now a digital device called a scanner to replace it. A scanner can be used to take a digital impression in a matter of seconds, which has numerous applications in clinical dentistry. Digital dentistry in general has gone through many evolutions in the last few decades. CAD/CAM dentistry has been around for almost 30 years, but just roughly 24% of dentists have adopted the technology.2
Within the past decade, dental laboratories have also benefited from the technology. This development is notable because when digital dentistry first came onto the market, it began to appear that laboratories would be removed from the equation. However, as implementation of the technology has advanced, laboratories have not become obsolete. Laboratories are finding ways to manufacture with technology such as scanners and mills so that they can benefit from the procedures being performed in dental offices as well as in the laboratory.
Another factor in how common digital dentistry has become is that the barriers to taking on the technology, including cost, access, and support, continue to decrease. Additionally, intraoral scanners are consistently more accurate than traditional impression techniques. Research has found that digital scanners exhibit 99.7% accuracy.3 This measure is determined by the feedback from dentists on remakes they receive from digital technology. Additionally, the internal fit of digitally manufactured restorations has been proven to be just as good, if not better, than traditionally manufactured restorations.4-6 These promising data suggest digital technology will soon eclipse many analog processes.
In implant dentistry, the digital shift has followed a similar trend in improvements and technological advancement. Figure 1 shows the making of a traditional impression, using impression posts and analogues to create a cast in the laboratory. Clinicians can now use scan bodies and digital technology to create an accurate impression, such as the image shown in Figure 2, which is sent to the laboratory and used to fabricate restorations.
A pilot study of an intraoral laser scanner for implant dentistry by Lee et al found that of 36 patients, six needed contact adjustments, seven required occlusal adjustments, and three needed a gingivectomy around the implant to completely seat the restoration. Chair time for adjustments did not exceed 15 minutes.7 For many clinicians, that much time will not be necessary for seating a digitally manufactured restoration. The aforementioned study also concluded that intraoral scanners are becoming more useful for implant diagnoses and digital treatment planning. They are also good presurgical tools for ideal surgical and restorative positioning of implants.
Team Collaboration in Digital Implant Dentistry
One of the keys to successful digital implant dentistry is proper preparation and a team-oriented approach, which can be understood through the pyramid of implant success. The four components of the pyramid are a useful guide for dental team structures. The team is vital for the result of all implant restorations. The restorative dentist forms one aspect of the pyramid and is essential for identifying the patient's needs through a diagnosis; however, this dentist cannot, and should not, be the sole clinician involved. The responsibility of the restorative dentist is threefold: to replace function, form, and esthetics. The second piece of the pyramid is the dental implant surgeon. In some practices, the restorative dentist and surgeon will be the same person. Regardless, the surgeon is usually the second expert the patient sees in the process of implant placement. The surgeon provides or evaluates the location, bone quality and quantity, restorability, and safety of placement for the particular implant or implants. The final professional in the pyramid is an entity the patient may never see or meet: the dental laboratory. The laboratory's job is similar to the restorative dentist's. In the end, the pyramid of implant success centers on the fourth component, the patient.
With full team collaboration that recognizes the importance of each facet of the pyramid, many errors in implant dentistry can be eliminated, and the more engaged treatment-planning process will aid the team in creating an ideal result. Poor planning can lead to suboptimal results, which is why clinicians are encouraged to communicate with their team. The dramatic growth in digital technology has made communication between different team members much easier. Perhaps one of the biggest aspects of implant cases the team is responsible for is the comprehensive diagnostic foundation.
Case Reports
Full team collaboration begins with comprehensive implant diagnostics. Here, three cases will be presented in which the patients could have benefited from a team approach.
The first case involved a 45-year-old man presenting with the complaint that his dentist told him they could not put a tooth on his implant. He was also unhappy with an implant that was placed too supragingivally. The healing cap was in contact with the distal tooth. The implant was not restorable in the position it was placed (Figure 3). If the patient were willing to undergo orthodontics, there may have been a chance to place a tooth on the implant. In the end, though, no matter what the clinician was able to place or how the adjacent teeth were modified, the result would not be optimal.
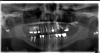
The second case was a 60-year-old man who primarily wanted new teeth. He had an All-on-4 case deemed appropriate by his surgeon. Unfortunately, proper preparation was not enacted, and the surgeon and restorative dentist were unfamiliar to each other. The surgeon evaluated the patient, decided an All-on-4 case would work, and sent the patient to the dentist for restoration. Figure 4 shows the result of this weak team dynamic. At the top there were four implants, and at the bottom there were three. The dentist did not feel the best result would come from using the three lower implants, so the patient was sent back to the surgeon with a recommendation that two more implants should be placed on the bottom. More implants were also desired on the top, but the sinuses would not allow it. If the surgeon and the dentist had discussed the case before the implants were placed, they could have proceeded further with the necessary implant placement much sooner.
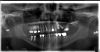
The final case was a 60-year-old patient who visited her clinician saying that her dentist had been procrastinating and all she wanted was her implants fixed. She presented with four implants in the No. 14, 15, 30, and 31 sites. The No. 30 and 31 implants, although not optimal, were likely restorable. Figure 5 shows that the No. 14 and 15 sites were not optimally placed for delivery of implant restorations.
In all three of these cases, a little more preparation could have led to better performance in the end. To remedy this situation and create a comprehensive implant diagnosis, clinicians should ask a few mandatory questions: (1) What are the restorative goals? (2) Is there enough bone of good quality? (3) Is it too close to a vital structure? (4) Is there enough room between teeth? (5) Is there too much room between teeth? (6) What are possible surgical complications? (7) Can the restorative goals be achieved?
Implant Placement Considerations
After these key questions, there are further implant placement considerations. For example, the Rules of Six, from Lyndon F. Cooper, DDS, PhD, are principles for creating or identifying appropriate implant-placement bone volume.8 The first of these rules considers interradicular distance and states that 6 mm of space is needed between the roots of adjacent teeth for a 3.5-mm implant. For example, a 3.5-mm implant should have 1.5 mm of space on each side. If the clinician is dealing with a 4-mm implant, 7 mm are needed between adjacent teeth (1.5 mm on either side), and so on for larger implants. The second rule dictates guidelines for buccolingual distance. Just as with interradicular distance, buccolingual distance requires 6 mm for a 3.5-mm implant. This allows 1 to 1.5 mm of buccal wall thickness on either side of the implant. As such, if the clinician thinks there should be at least 1 mm on either side, 1.5 mm would better. For a 3-mm implant, the clinician would need 5 mm of bone.9
The next consideration is implant length, which, according to Cooper, should be a minimum of 6 mm. Short implants can pose some complications, so it is advisable to go with at least 10 mm in length. However, the research indicates that at least 6 mm should be sufficient. When determining the best length, it is also crucial to account for occlusal stresses and interfering stresses that the implant will be taking on. The fourth rule states that 6 mm of interocclusal distance is needed between the abutment and opposing dentition. This tells the clinician how long the abutment should be.8
Of particular importance to implant esthetic considerations is the fifth rule, which states that there must be 6 mm between the interproximal contact and bone crest. This is extremely important for maintaining the papilla between teeth, especially when working in the anterior region. The final rule is too often overlooked; it is also the most difficult to achieve. This rule states that implants must be placed in specific orientation to the soft-tissue reference of the gingival zenith. The implant abutment interface should be 3 mm apical and 2 mm palatal to the gingival zenith of the planned restoration. Although challenging to accomplish in the esthetic zone, this rule is a good goal to aim for when placing implants.8
An additional consideration is the apicocoronal position of the implant. Problems can arise when an implant is placed too deep, including soft-tissue collapse, cementation issues, or an odd emergence profile if the implant is too coronal. The ideal placement is 3 to 4 mm beneath the free gingival margin in the esthetic zone. Moreover, the interproximal distance between two teeth is one thing, but the distance between two implants is quite different. A minimum of 3 mm is needed between two implants, which means that between two teeth, the distance between the teeth and the distance between the implants as well as the width of the implants need to be accounted for to ensure there is an appropriate distance of 3 mm between implants. After these implant considerations have been assessed, papilla and bone height can be more easily conserved.10
Diagnostic Data Essentials
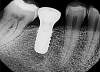
Gathering diagnostic data is the next step in properly assessing the patient. All types of diagnostics are not appropriate for every circumstance. For example, a periapical radiograph will not be the final stopping point for an implant placement, but it is a useful tool because it shows both bone quality and quantity. It can also demonstrate interradicular distance and contradicting pathology, which is useful for measuring the interproximal contact of the bone crest in various implant positions. However, as shown in Figure 6, it is not beneficial for every indication, especially on a cuspid where the implant is going to be placed in the corner of the mouth. It is virtually impossible to get a periapical radiograph repeatedly and predictably that will provide the appropriate distances needed.
The panoramic radiograph is a good diagnostic tool to implement as well, but with rotation of the cone around the patient's head and neck, there is going to be a distorted bone level. Figure 7 shows an artifact that can occur with the panoramic radiograph, where the patient's earrings relay across the ridge. Artifacts such as this and other distorted findings indicate that the radiograph should not be the sole tool for implant placement.
CBCT is a tool that clinicians can benefit from greatly in implant diagnoses. CBCT offers a high-resolution 3-dimensional (3D) image with doses more than 15 times lower than conventional radiography.11 Volumetric imaging can be taken in less than 6 seconds. CBCT is performed in an open environment, so patients don't feel any claustrophobia that comes with a traditional CT machine. A review of CBCT applications in the dental practice found that CBCT has reduced implant failures by providing information about bone density, the shape of the alveolus, and the height and width of the proposed implant site for each patient.12 The recommendation of the American Academy of Oral and Maxillofacial Radiology is to use some form of cross-sectional tomographic images for treatment planning dental implant cases.13
In addition to proper imaging for implant diagnosis, models should be used for implant placement. Digitally scanned models can be used, or traditional models can be made and converted to digital. After collecting images and models, clinicians can use software that provides prosthetic-driven implant-planning solutions, taking the CBCT and models and incorporating them into a single location for the restorative dentist, surgeon, and laboratory so that the team can communicate goals and set an end point.
An advantage of this type of software is seamlessly integrating the preoperative and prosthetic procedures. If placement and diagnosis are accurate, the clinician can immediately provisionalize the patient. Another advantage is that the clinician can create bone-supported or teeth-bone supported drill-guide fabrications (stents) for proper implant placement. The software improves communication between the dentist, laboratory, surgeon, and patient.
Guided Implant Surgery for Case Success
After all data are collected, the final step in the process is guided implant surgery. Guided surgery provides a restorative-driven surgical approach with a clear end point. The surgeon works from the same restorative plan as the dentist and laboratory, with preplanning completed ahead of time to eliminate guesswork and errors.
Figure 6 showed a case where the patient presented with some internal resorption on tooth No. 11 that had been occurring for a number of years. The patient knew he needed an implant, but he also needed much additional work. The radiograph showed that the patient had internal resorption that could have started as external resorption but breached the tooth. There was also an infection in the alveolus that needed to be addressed with detailed planning.
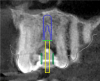
The CBCT and digital scan were placed in software to merge the two. Figure 8 shows the superimposition of the scan over the CBCT. The clinician used the volumetric data to determine implant size, depth, and position. The surgeon, dentist, and laboratory were all involved in a conference call to go through several different implants. They chose the implant size and length based on the position of the sinus, the width of the alveolus, and the appropriate position for an ideal surgical result.
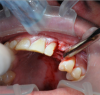
These data were used to fabricate the surgical guide and a temporary. Figure 9 shows the implant in place digitally. All the data and models were taken into account before surgery. The clinician received a 3D-printed model with the tooth extracted, a guide (Figure 10), and a healing cap and temporary (Figure 11). The latter two were required for initial stability of the implant to immediately provisionalize. The "bail-out clause" is the healing cap because if the implant cannot be immediately loaded, the healing cap can be placed instead. For this case, the patient's tooth was extracted and bone had been grafted several months previously. Figure 12 shows the patient's previous tooth bonded into place. The flap was laid (Figure 13) and the surgeon was given a set of instructions that come with every guided case.
These instructions typically comprise the implant position, type of implant, sleeve height, sleeve position, milling cutter, guided drill, cylinder drill, handle, profile drill, C handle, and tap. All of these aspects are used as a map for the dentist or surgeon to go through the guided surgery. Each of these items is also typically represented on a computer screen or a readily available print guide, as well as on the surgical kit for the patient.
The surgeon then began the surgery, placed the guide, started drilling an initial pilot drill, and verified the angulation. After that was completed, he went through the various procedures and finally got to the point of placing the implant.
Guided surgery can be performed with either a guided or non-guided implant. In this case, the surgeon used a guided implant, and a stop key informed him when the implant was placed to the appropriate depth. Figure 14 shows a mark on the guide that lines up with markings on the side of the implant. The laboratory-fabricated temporary was placed through digital techniques. The temporary went directly on top of the implant, as shown in Figure 15, exactly as planned. It was used because there was primary stability of the implant and thus the healing cap was not needed.
Considerations for Immediate Loading
Three considerations must be reviewed for immediate loading of implants: implant features, initial stability, and bone quality and quantity. In regard to implant features, the surface, shape, grooves, and length of the implant are of particular importance. An osteoconductive surface is preferable, and a tapered implant will have a better result.14 Grooves and a length of 10 to 13 mm are additional requirements for improving the chances of immediate stability and loading a single-tooth implant.14 It is also important to examine bone quantity and quality using a CBCT before the surgery to observe volume, density, and whether it is an extraction site, although at times the situation can appear differently when actually doing the surgery. If there was bone grafting at the time of placement, the implant most likely cannot be loaded immediately.
The key factor for immediately loading an implant is initial stability, which means the implant should be well anchored with at least 35 Ncm of torque at placement. There should be no difference in implant success when comparing a two-stage approach to an implant that is loaded immediately as long as it is initially stable.14
An advantage of immediately loading an implant is having a single surgical procedure. Additionally, the treatment time is shortened, there is no need to uncover the implant, fixed provisionalization is possible, and soft tissues can be sculpted with the tooth form.15 The most important advantage is that the patient leaves with a tooth. The greatest disadvantage is that this procedure requires coordination and communication between the surgeon, dentist, and laboratory unless the same person is performing all three roles.
The definitive tooth-colored abutment is somewhat difficult to prepare during the placement of the implant. Because it is a surgical site, adjusting in the patient's mouth should be limited as much as possible. Similarly, staining with a polymethyl methacrylate (PMMA) should be kept to a minimum, but immediate loading is the best option, if at all possible.14
For this case, immediate loading was completed. Figure 16 shows the patient 2 weeks postoperatively. The tissue was healing well, and the patient decided to go through with bleaching his teeth. The results after 3 months of healing are shown in Figure 17. The shade was chosen by the patient. He then wanted to redo the rest of his teeth because of how successful the treatment was using digital dentistry.
Conclusion
Digital dentistry has improved many aspects of the profession, especially in the way implant dentistry is performed and the results for patients. Scanners, guided surgery, CAD/CAM design, and more are together drastically improving the quality of treatment outcomes. After multiple skilled professionals, including the restorative dentist, dental laboratory, and surgeon, communicate effectively about patient goals and needs, the technology is truly able to enhance restorative and surgical processes. Digital technology has resulted in crucial tools that are more effective and accurate. Digital scans, models, and CBCT have ensured diagnoses can closely represent a patient's true condition and lead to greater implant placement success.
About the Author
Chad C. Duplantis, DDS
Private Practice
Fort Worth, Texas
References
1. Dental implants facts and figures. American Academy of Implant Dentistry. http://www.aaid.com/about/Press_Room/Dental_Implants_FAQ.html. Accessed June 20, 2018.
2. 2015 technology census. Dental Product Shopper. 2016;10(2).
3. Data on file. 3M. 2015.
4. Ng J, Ruse D, Wyatt C. A comparison of the marginal fit of crowns fabricated with digital and conventional methods. J Prosthet Dent. 2014;112(3):555-560.
5. Vennerstrom M, Fakhary M, Von Steyern PV. The fit of crowns produced using digital impression systems. Swed Dent J. 2014;38(3):101-110.
6. Paradies G, Zarauz C, Valverde A, et al. Clinical evaluation comparing the fit of all-ceramic crowns obtained from silicone and digital intraoral impressions based on wavefront sampling technology. J Dent. 2015;43(2):201-208.
7. Lee CY, Wong N, Ganz SD, et al. Use of an intraoral laser scanner during the prosthetic phase of implant dentistry: a pilot study. J Oral Implantol. 2015;41(4):e126-e132.
8. Cooper LF, Pin-Harry OC. "Rules of Six"--diagnostic and therapeutic guidelines for single-tooth implant success. Compend Contin Educ Dent. 2013;34(2):94-98.
9. Chiche FA, Leriche MA. Multidisciplinary implant dentistry for improved aesthetics and function. Pract Periodontics Aesthet Dent. 1998;10(2):177-186.
10. Gastaldo JF, Cury PR, Sendyk WR. Effect of the vertical and horizontal distances between adjacent implants and between a tooth and an implant on the incidence of interproximal papilla. J Periodontol. 2004;75(9):1242-1246.
11. John GP, Joy TE, Mathew J, Kumar VR. Fundamentals of cone beam computed tomography for a prosthodontist. J Indian Prosthodont Soc. 2015;15(1):8-13.
12. Alamri HM, Sadrameli M, Alshalhoob MA, et al. Applications of CBCT in dental practice: a review of the literature. Gen Dent. 2012;60(5):390-400.
13. Tyndall DA, Price JB, Tetradis S, et al; American Academy of Oral and Maxillofacial Radiology. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg Oral Med Oral Path Oral Radiol. 2012;113(6):817-826.
14. Ostman PO, Hellman M, Sennerby L. Direct implant loading in the edentulous maxilla using a bone density-adapted surgical protocol and primary implant stability criteria for inclusion. Clin Implan Dent Relat Res. 2005;7(suppl 1):S60-S69.
15. Immediate load implants. Dentistry IQ. http://www.dentistryiq.com/articles/wdj/print/volume-5/issue-4/you-and-your-practice/immediate-load-implants.html. Published July 1, 2007. Accessed June 20, 2018.