You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Ever since the publication of the first United States (U.S.) Surgeon General's report on oral health in 2000, it has become common knowledge that certain segments of the U.S. population do not only have higher rates of oral disease, but are also likely to encounter challenges when seeking oral health care services.1 Individuals from socioeconomically disadvantaged and/or ethnic/racial minority backgrounds and those with special health care needs are particularly impacted by access to care barriers. One strategy for addressing the access to oral health care problem is to increase the scope of practice of dental hygienists, while concurrently decreasing the level of supervision by dentists.2 There are several ways to achieve such a professional change. One strategy is to increase the extent of dental hygienists' contributions through the adoption of a "direct access" model. This model allows dental hygienists to initiate treatment based on the assessment of a patient's needs without specific authorization of a dentist, treat patients without the presence of a dentist, and maintain a provider-patient relationship.2,3 Currently, 39 states have adopted policies enabling dental hygienists to provide oral health care to underserved populations through direct access models.4,5 While these states differ in which treatments dental hygienists are allowed to provide without direct supervision by a dentist, the provision of an oral prophylaxis, dental sealants, and application of topical fluoride have been included by the majority of the 39 states who use this model.6 A second approach to utilizing dental hygienists' capabilities to increase access to care is by introducing state-specific policies for indirect supervision by a dentist, such as the Public Act 161 in the state of Michigan.2 Catlett and Greenlee's comparison of the 50 states' and the District of Columbia's supervision requirements for dental hygienists from 1993 - 2000 versus 2001 - 2011 demonstrated a clear decrease in the required levels of supervision for 11 types of services over this time span.7
Historically, efforts to expand dental hygienists' scope of practice have faced opposition from dentists,8 and changes in dental hygienists' scope of practice in the U.S. are clearly not independent of general dentists' attitudes and behavior concerning dental hygienists' professional role. Reactions to the most recent changes in the dental hygiene profession reducing the need for direct and indirect supervision, in addition to the introduction of the dental therapist model, have been mixed.9-11 Some investigators have argued that negative reactions might be due to concerns regarding the quality of care provided by dental hygienists or to concerns about a competitive advantage of lower costs of care provided by dental hygienists that could harm dentists' earning potential.8 However, it is also possible that the resistance stems from the fact that dentists do not understand dental hygienists' scope of practice and the complex set of services they are able to provide. Research dating back to 1991 has shown that dental hygienists were not being utilized to provide their full range of professional services.12 There is a gap in the literature in regards to data analyzing dentists' knowledge of the legally allowable dental hygiene duties in their state and whether this knowledge level correlates with what duties they ask the dental hygienists in their own practices to perform. Exploring whether this relationship exists in context with the value dentists place on the services and contributions dental hygienists make in the dental practice, could provide insight into dentists' attitudes towards efforts to expand the scope of practice and decrease direct supervision duties. Insights gained concerning dentists' knowledge and attitudes may prove beneficial in creating a political support base for efforts to change dental practice acts.
The purpose of this study was to assess general dentists' perceptions and knowledge of what dental hygienists are legally allowed to perform in their state versus what services they actually provide in their individual practice; the importance of dental hygienists' contributions to their practice; and how well dental hygienists interact with dentists and patients. Relationships between dentists' attitudes, their age and number of dental hygienists and dental assistants employed in their practices and dental hygienists' actual duties in the dental practice were also examined.
Methods
Survey data were collected from general dentists who were all members of the Michigan Dental Association. This study was determined to be exempt from Institutional Review Board (IRB) oversight by the IRB for the Behavioral and Health Sciences, University of Michigan, Ann Arbor, MI. A draft version of the survey was pilot tested with six general dentists working in private practice settings and their feedback was used to finalize the survey. The MDA provided a membership list of approximately 6,000 members; a random number generator was used to select the 900 dentists who received the postal mailed, paper-pencil survey. The mailing included the survey and a cover letter from the academic dean of the University of Michigan School of Dentistry explaining the purpose of the anonymous study and an invitation to participate. A stamped, self-addressed return envelope was included in the mailing.
The survey consisted of four sets of questions. Part 1 included questions concerning the respondents' socio-demographic background, education, and practice characteristics. Part 2 consisted of a list of twenty-six procedures dental hygienists are legally allowed to perform in the State of Michigan. For each procedure listed, respondents were asked (A) if dental hygienists are able and permitted to provide this treatment, and (B) if dental hygienists in their own practice were currently performing these procedures. The answer alternatives for the questions regarding legally allowable procedures were "Yes", "No", and "Unsure", while the answer alternatives to the questions regarding what they allowed in their own practices were either "Yes" or "No". Questions regarding dental hygienists' contributions to the practice were included in Part 3. The first eight questions asked respondents to indicate on a 5-point scale (1="not at all important" to 5="very important") how important dental hygienists' input was for treatment and diagnostic considerations in their dental practice. Categories included diagnosis of periodontal disease, clinical caries, radiographic findings, oral cancer screening, temporomandibular joint dysfunction, and mucositis and explanations of treatment processes and outcomes. Six additional items regarding dentists' perceptions of the dental hygienists' contributions to their practice had a Likert-style response format, with 5-point answer scales ranging from 1="disagree strongly" to 5= "agree strongly." Part 4 included 3 items pertaining to interactions between dentists and dental hygienists and 7 items regarding dental hygienists' patient management skills.
Statistical analyses
Responses were entered into an SPSS data file (IBM Corp. Released 2013. SPSS Statistics for Windows. Version 22. Armonk, NY: IBM Corp). Descriptive statistics such as frequency distributions, means and standard deviations were computed to provide an overview of the responses. A factor analysis (Extraction Method: Principal Component Analysis; with Varimax Rotation) of the items included in Parts 3 and 4 of the survey was used to determine which questions loaded on the same factors. Indices were computed based on the results of the factor analysis. Cronbach alpha coefficients were used to determine the inter-item consistency of the indices. Inferential statistics determined whether Pearson correlation coefficients were significant (p<.05).
Results
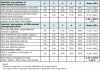
Responses were obtained from 292 (n=292) of the randomly selected MDA members (n=900) who received a postal mailed survey for a response rate of 32%. Table I shows that the majority of respondents were male (75%), from European American backgrounds (95%), ranging in age from 26-83 years (mean=52.23 years) and had graduated from dental school between 1962 and 2014. About one third (32%) practiced in a small town, 29% in a moderate sized city, 23% in a suburb of a large city and 11% in a large city. The highest percentage of responses (36%) came from dentists who were practice owners, followed by 31% indicating that they worked in a solo practice setting, 15% who worked in a partnership, 12% who worked in a group practice, and 10% who were associates. The remainder were employed in corporate practices (5%), followed by community dental clinics (3%), and academia (2%). The number of dental hygienists employed ranged from 0-40 (mean=3), the number of assistants ranged from 0-15 (mean=3) and the number of other staff members ranged from 0-11 (mean=3). Respondents worked on average 31 hours per week and treated an average of 61 patients per week. Dental insurance was the primary payment type for 80% of the respondents, followed by 39% self pay and 3% Medicaid. Twenty-two percent of the respondents reported caring for low-income patients.
Respondents' knowledge of the 26 different allowable duties for dental hygienists in Michigan and the actual duties that were performed in their individual practices are presented in Table II. The 26 services were categorized as preventive, diagnostic, patient behavior-related, pain management-related or related to supplemental/technical therapies or other services. Preventive services such as dental prophylaxis, scaling/root planing, periodontal maintenance, application of topical fluorides were provided by 99% of the dental hygienists in the practices surveyed. However, placement of dental sealants was only performed by 69% of the clinicians. The majority of dental hygienists (98%) completed periodontal chartings, 98% obtained medical histories and 98% took radiographic images. Recording patient vital signs and caries risk assessment was performed by 81% of dental hygienists, oral cancer screenings by 75%, intra and extra oral examinations by 68%, and radiographic interpretation by 68%. Nearly all dental hygienists (99%) were engaged in some sort of patient education. However, only 71% were involved in nutritional counseling and 61% in tobacco cessation counseling. The percentage of dental hygienists who applied desensitizing agents was 87%, while 70% administered local anesthesia, and 60% nitrous oxide sedation. Additional procedures allowed in the state of Michigan such as taking alginate impressions (52%), pouring cast models (36%), removing restoration overhangs (26%), adjusting restorations (1%), tooth whitening (40%), suture removal (21%) and supportive orthodontic treatment (15%) were performed by significantly fewer dental hygienists.
Dentists' responses concerning the importance of dental hygienists' input for dentists' patient care and the dental hygienists' contributions to the practice are shown in Table III. Overall, the vast majority of respondents agreed that dental hygienists play a very important (91%) role as a member of the dental team. When asked about the importance of the dental hygienists' input into different types of clinical practice behaviors, the majority of the respondents viewed the dental hygienists' input into the diagnosis of periodontal disease (85%) and the explanation of the treatment process and outcomes (66%) as being very important. However, fewer than half rated the role of dental hygienists in the diagnoses of oral cancer (47%), clinical caries (34%), radiographic findings (34%), mucositis (30%), and temporomandibular joint disorders (23%) as being very important. An index of clinical competence was computed by averaging the responses to these 7 items, and the mean response was 4.07 on a 5-point scale, demonstrating a positive rating of dental hygienists' clinical competence.
Dental hygienists' contributions to the respondents' practices were also viewed as positive. The majority of respondents considered dental hygienists to be well integrated into their practices (67%), that they worked well in a team environment (66%), and required little supervision (67%). Additionally, the majority agreed that dental hygienists managed their time well, were responsible for determining appropriate patient recall, and were capable of determining appropriate individualized treatment (Table III).
Table IV shows that the majority of respondents either agreed (28%) or strongly agreed (68%) that they valued the recommendations of dental hygienists in their practices; that they were comfortable speaking with dental hygienists where patient care is concerned (agreed:17%/strongly agreed:80%), and thought dental hygienists benefitted the business aspects of their practice (agreed:19%/strongly agreed:59%). Dentists' perceptions of the dental hygienists' patient management skills were also positive with the majority either agreeing or strongly agreeing that dental hygienists in their practices effectively created behavior change in patients (agreed: 39%/strongly agreed: 46%). Patient rapport, conflict resolution, specialized skills and patient communication skill responses are shown in Table IV.
An overview of the Pearson correlation coefficients for the relationships between the four attitudinal indices described in Tables III and IV and the six sum scores of dental hygienists' performed professional services (preventive services; diagnostic services; patient behavior modification; pain management; supplemental services and other services) is provided in Table V. The findings demonstrate an interrelationship in the respondents' attitudes. The higher the respondents rated their dental hygienists' clinical contributions to their practice, the more they considered them to make contributions to the practice overall (r=.34; p<.001), have better interactions with dentists (r=.40; p<.001), and better patient management skills (r=.34; p<.001). Attitudinal responses were also correlated with the different types of services assigned to dental hygienists by these respondents. While all four attitudinal indices were positively correlated with assigning diagnostic and supplemental services, only the importance of dental hygienists' clinical contributions was correlated with assigning them to engage in other services, and positive attitudes concerning dental hygienists' patient management skills were only positively correlated with patient behavior modification.
Relationships between respondents' age, the number of dental hygienists and assistants employed with the four attitudinal indices and the six sum scores of services the dental hygienists actually provide are summarized in Table VI. The findings demonstrate that the older the respondents were, the more they valued the clinical contributions of dental hygienists (r=.21; p<.001), and the more diagnostic procedures (r=.13; p<.05), technical services (r=.15; p<.05) and other services the dental hygienists performed (r=.13; p<.05). The number of dental hygienists and dental assistants employed in dentists' practices did not correlate with their attitudes. However, the number of dental hygienists negatively correlated with the number of additional services (r=-.13; p<.05) they provided in the respondents' practices. The number of dental assistants employed positively correlated with the number of pain management services (r=.21; p<.001) dental hygienists provided, but negatively with the sum of other services provided (r=-.14; p<.05).
Discussion
Dental hygienists have the potential to make significant contributions to resolving the access to dental care challenges of underserved populations in the U.S.8 Current advancements in the profession including increases in the number of direct access states4,5,9-11 and the development of specialized programs with increased responsibilities and professional autonomy as demonstrated in the dental therapist model,13-15 are trends that will continue. However, a moderating factor to this progress has been the input of dentists. Their understanding of dental hygienists' scope of practice along with their attitudes and behavior related to their professional interactions with dental hygienists are critical factors influencing their acceptance of changes in supervision levels and scope of practice of dental hygienists. Insight into the basis for their knowledge and attitudes can serve to inform the necessary educational interventions and guidance for how dental schools and professional organizations provide information aimed at increasing awareness of the role that dental hygienists play.
While over 90% of the respondents knew that dental hygienists in Michigan could provide all 5 of the preventive services, 5 out of 8 of the diagnostic services, and 2 out of the 3 behavior and pain management strategies respectively, less than 90% were aware that dental hygienists in the state of Michigan could also perform the other 12 of the 26 services listed. This lack of knowledge concerning dental hygienists' full scope of practice indicates a need for change. Dental school programs should explore strategies to ensure that graduates are educated about dental hygienists' scope of practice in order to work with them effectively. A discussion of whether such efforts should be solely focused in dental education settings or whether interprofessional education (IPE) efforts16-20 would be best suited to achieve optimal dental education goes beyond the scope of this paper. Additionally, continuing education programs from both dental and dental hygiene professional organizations can serve to provide ongoing updates on any changes in regards to dental hygienists' scope of practice as well as full utilization of the legally allowable duties. Data from this study showed that the more knowledge dentists had regarding the full spectrum of duties including the administration of nitrous oxide, removal of overhangs and adjusting restorations among other services, the more likely they were to delegate these services to a dental hygienist.
In addition to understanding dental hygienists' scope of practice, dentists' attitudinal responses concerning the value of their contributions to a dental practice should be considered. Dentists' attitudes towards dental hygienists in this study were very positive. However, correlations between these positive attitudes and the actual procedures that were delegated to dental hygienists were not consistently high. Exploring more explicit connections between dentists' attitudes and specific types of professional behaviors such as pain management strategies and tobacco cessation counseling might be achieved through team-based IPE. Clinical or community- based IPE experiences with dental and dental hygiene students working collaboratively could result in increased positive attitudes concerning dental hygienists' role and contributions to patient care.
Results from this survey showed that the respondents were much more likely to delegate preventive services to the dental hygienist over the adjunctive services. This may be due to the fact that these were billable services that generate incrementally more revenue than the other services. In addition, dental assistants, have overlapping scope of practice for diagnostic procedures such as taking alginate impressions and radiographic imaging. When considering why some respondents may not be delegating local anesthesia and nitrous oxide to dental hygienists, the lower rates may be due to the relatively recent addition of these expanded duties in the state of Michigan (2002 and 2004 respectively).
The relationship between the age of the dentist and their appreciation of the clinical contributions of dental hygienists is a finding that deserves further discussion. Data from this study demonstrated that the older the dentists were, the more they appreciated the clinical contributions of dental hygienists' and the higher their involvement in diagnostic and adjunctive services. Younger respondents demonstrated lower levels of appreciation and were less likely to utilize all of the duties dental hygienists are allowed to perform.
The assumption that the more recent graduates would appreciate the role of dental hygienists more and involve them in a wider range of services did not bear true in this study and raises the question whether more IPE and interprofessional collaboration opportunities between dental students and dental hygiene students would change these perceptions and increase the full utilization of dental hygienists.
This study had several limitations. There was a potential self-selection bias of respondents, with respondents being more favorable towards a decrease in supervision of dental hygienists and an increase in the scope of practice of dental hygienists as compared to non-respondents. Additionally, the relatively small number of respondents does not allow for sub-group comparisons such as whether dentists who are practice owners differ in their responses from dentists working in community dental clinic settings. Future research should aim at increasing the number of respondents to allow more in-depth analyses. Results from this study are limited to the state of Michigan. A national survey would provide a basis for generalizations of the findings.
Conclusions
The majority of the dentist respondents from the State of Michigan reported having knowledge of the range of preventive and diagnostic services, pain management and patient behavior modification strategies a dental hygienist is allowed to provide. However, gaps in knowledge regarding the full scope of dental hygiene practice indicate a need for future educational efforts in dental school settings and in continuing education courses for practicing dentists. The range of services that dental hygienists actually provided in the dental practices of the respondents highly correlated with the dentists' beliefs regarding the allowable duties for dental hygienists. Overall, respondents had exceptionally positive attitudes regarding both the clinical and general contributions dental hygienists made to their practices, their patient management skills, and their interpersonal interactions in the dental setting. However, these positive attitudes did not translate into full utilization of the dental hygienists' scope of practice in the state of Michigan. Interprofessional education in dental school setting might provide the basis for improving dental team members' knowledge about each other's scope of practice, attitudes and professional competencies.
Acknowledgments
This study was made possible by a University of Michigan, Rackham Graduate School student grant to the first author. The authors wish to thank the Michigan Dental Association for the provision of their member addresses and the respondents for their time in responding to this survey.
About the Authors
Samantha K Mishler, RDH, MS is an adjunct clinical lecturer, Department of Periodontics and Oral Medicine; Marita R Inglehart, Dr. phil. habil. is a professor, Department of Periodontics and Oral Medicine, School of Dentistry and adjunct professor of psychology, College of Literature, Science, and the Arts; Martha J McComas, RDH, MS is a clinical assistant professor, Department of Periodontics and Oral Medicine; Carol Anne Murdoch-Kinch, DDS, PhD is an associate dean, Academic Affairs and the Dr. Walter H Swartz Professor of Integrated Special Care Dentistry, Department of Oral and Maxillofacial Surgery/Hospital Dentistry; Janet S Kinney, RDH, MS is an associate professor and director, Division of Dental Hygiene, Periodontics and Oral Medicine; all at the University of Michigan School of Dentistry, Ann Arbor, MI.
Corresponding author: Marita Rohr Inglehart, Dr. phil. habil.; mri@umich.edu
References
1. U.S. Department of Health and Human Services. Oral health in America: A report of the surgeon general. [Internet]. Rockville (MD): U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000 Sept [cited 2011 Feb 1]. 332 p. Available from: https://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Documents/hck1ocv.@www.surgeon.fullrpt.pdf
2. Pervez A, Kinney J, Gwozdek A, CM Farrell, Inglehart MR. Michigan's PA 161 Public Dental Prevention Program: Dental and Dental Hygiene Students', Faculty and Licensed Hygienists' Educational Experiences, Knowledge, Attitudes, and Interests. J Dent Educ, 2016 Sep;80(9):1071-81.
3. American Dental Hygienists' Association (ADHA). Direct access. [Internet]. Chicago: American Dental Hygienists' Association. 2010 Mar [cited 2013 Sept 6]. Available from: http://www.adha.org/direct-access
4. American Dental Hygienists' Association (ADHA). Revised standards for clinical dental hygiene practice. [Internet]. Chicago: American Dental Hygienists' Association. c2012-2015 2016 [cited 2016 June 3]; [about 40 screens]. Available from: https://www.adha.org/resources-docs/2016- Revised-Standards-for-Clinical-Dental-Hygiene-Practice.pdf
5. Naughton DK. Expanding oral care opportunities: direct access care provided by dental hygienists in the United States. J Evid Base Dent Prac. 2014 Jun;14 Suppl:171-82.e1.
6. American Dental Hygienists' Association (ADHA). Direct access states. [Internet]. Chicago: American Dental Hygienists' Association. Updated 2016 Dec [cited 2017 Jan 18]. Available from: http://www.adha.org/resources-docs/7513_ Direct_Access_to_Care_from_DH.pdfhttp://www.adha.org/governmental_affairs/downloads/ direct_access.pdf.
7. Catlett AV, Greenlee R. A retrospective comparison of dental hygiene supervision changes from 2001 to 2011. J Dent Hyg. 2013 Jun;87(3):110-7.
8. American Dental Hygienists' Association. Access to care position paper. Chicago (IL): American Dental Hygienists' Association; 2001. 9p.
9. Reinders JJ, Krijnen WP, Onclin P, van der Schans CP, Stegenga B. Attitudes among dentists and dental hygienists towards extended scope and independent practice of dental hygienists. Int Dent J. 2017 Feb;67(1):46-58.
10. Blue CM, Funkhouser DE, Riggs S, et al. Utilization of nondentist providers and attitudes toward new provider models: Findings from the National Dental Practice-Based Research Network. J Public Health Dent. 2013;73(3):237-44.
11. Blue C, Phillips R, Born D, et al. Beginning the socialization to a new workforce model: dental students' preliminary knowledge of and attitudes about the role of the dental therapist. J Dent Educ. 2011 Nov;75(11):1465-75.
12. Pritzel SJ, Green TG. Working relationship between dentists and dental hygienists: their perceptions. J Dent Hyg. 1990 July-Aug;64(6):269-72.
13. Blue CM. Kaylor MB. Dental therapy practice patterns in Minnesota: a baseline study. J Comm Dent Oral Epidemiol. 2016 Oct;44(5):458-66.
14. Mathu-Muju KR. Chronicling the dental therapist movement in the United States. J Public Health Dent. 2011 Fall;71(4):278-88.
15. Fiset L. DENTEX: the emergence of dental therapists in the United States. JAAPA. 2016 Apr;29(4):1-5.
16. Formicola AJ, Andrieu SC, Buchanan JA, et al. Interprofessional education in U.S. and Canadian dental schools: an ADEA Team Study Group report. J Dent Educ. 2012 Sep;76(9):1250-68.
17. Furgeson D, Kinney JS, Gwozdek AE, Wilder R, Inglehart MR. Interprofessional education in U.S. dental hygiene programs: A national survey. J Dent Educ. 2015 Nov;79(11):1286-94.
18. McComas MJ, Inglehart MR. Dental, dental hygiene, and graduate students' and faculty perspectives on dental hygienists' professional role and the potential contribution of a peer teaching program. J Dent Educ. 2016 Sep;80(9):1049-61.
19. Munz SM, Kim RY, Holley TJ, Donkersloot JN, Inglehart MR. Dental hygiene, dental and medical students' OMFS/hospital dentistry-related knowledge/skills, attitudes and behavior: an exploration. J Dent Educ. 2017 Feb;81(2):149-61.
20. Ateah C, Snow W, Wener P, MacDonald L, et al. Stereotyping as a barrier to collaboration: does interprofessional education make a difference? Nurse Educ Today. 2011 Feb;31(2):208-13.