You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Published studies document that musculoskeletal disorders (MSDs) have been a potential occupational health hazard to practicing dental hygienists since the late 1980s.1-9 There is also evidence that some individuals may develop MSDs early in their exposure to the profession, even as students prior to entering clinical practice.4,9-11
Numerous studies have addressed the prevalence, type, location and severity of MSDs among practicing dental professionals.1-9,16,17 Additional publications in the non-refereed literature also discuss specific dental practice-related ergonomic challenges, advancements in ergonomic technologies, and suggestions for interventions to both prevent and treat MSDs.
Collectively, the results reveal that the predominant areas of MSDs and related pain identified and reported by dental hygienists were in the neck, back, shoulder, and hand/wrist. The body of literature supports that MSDs are a major cause of concern for dental hygienists in clinical practice.1,3,5-7,16,17
Dental hygienists perform procedures while seated next to patients from various positions, which in education settings, are typically referenced as clock positions. Clock guidelines for practicing dentistry have been based on whether the dentist/hygienist is working with a dental assistant.18 The clock position/zones referenced in basic instrumentation textbooks for both right-handed (RH)/left-handed (LH) operators places the patient's head at 12:00 o'clock, with instrumentation approaches from the 7:00/8:00-12:00 o'clock position for right-handed and 5:00/4:00-12:00 o'clock position for left-handed operators.19-23 These working positions/zones are taught in the majority of dental hygiene programs in Mississippi, and are referenced as the traditional, or ‘front', approach to operator positioning.
The Performance Logic (PL) model, developed in the 1960s as a component of "sit-down" dentistry, proposed an alternative approach to operator positioning, differing from the traditional front approach. The PL positioning model provides a systematic approach to operator and patient positioning by allowing the operator to self-determine and maintain a natural position for procedures performed.24-26 Theoretically, this self-derived position can repeatedly be determined by the operator, and varies among individuals. PL encompasses more than the where and how of how the dental hygienist sits and moves around the patient. Proper placement of the patient's chair and head position (specifically the maxillary occlusal plane) and the accessibility and placement of the operator's equipment are critical components of PL.26 Patient head position is particularly critical as the operator's spine typically parallels the patient's occlusal plane; failure to monitor the occlusal plane results in poor operator postures.27 With PL, the operator does not perform procedures from the seated front position, but instead uses clock positions ranging from 10:00 o'clock to 12:30 for right-handed operators, referenced as the "back" position.
Schoen and Dean's periodontal instrumentation text was the first dental hygiene instrumentation manual to discuss PL and the proprioceptive self-derivation approach to instrumentation.28 The text offers pictures and directions for alternative positioning when eliminating the 8:00 operator position. While there is generally some consensus among existing dental hygiene textbooks used in academic programs as to the value of PL and use of the back position, some minor variations occur in the descriptions of optimal sitting positions according to the clock. Therefore, practitioners may approach positioning while performing dental hygiene care from slightly modified locations. Operators may choose to work from either beside or behind the patient depending upon which textbook method was used to teach instrumentation skills.
Little is known about the long-range impact of use of PL and other ergonomic training models for preventing MSDs among practicing dental hygienists. Two studies have investigated the benefits of PL among dentists while one qualitative study analyzed the benefits of PL among dental hygienists.29-31 Sunell and Maschak found that only 12% (n=25) of dental hygienists reported ‘new' neck/back/shoulder pain after practicing PL. Comments as to benefits of practicing PL included greater comfort, less fatigue, decreased muscle soreness, and less strain to the neck/back/shoulders. Dental hygiene faculty believed that the problem-solving frame of the PL model also produced students who were more self-directed in analyzing instrumentation principles.31
Several research studies have examined development of MSDs with assessment of clock positions as part of the study design. Using a modified version of the Standardized Nordic Questionnaire (SNQ), Liss, et al. compared prevalence, symptoms, and diagnoses of carpal tunnel syndrome (CTS) with work-related factors consisting of number of years in practice, dominant hand used while scaling, and characteristics of patients treated by dental hygienists.6,32 While only 10% of dental hygienists developed CTS, factors that most strongly predicted prevalence of CTS included treating 3 to 4 patients with heavy calculus each day (high degree of difficulty), working for 5 to 14 years in practice, and sitting in the 10:00 and 12:00 o'clock operator positions ("back" positions). Anton, et al. examined prevalence of CTS and MSDs among dental hygienists also using a modified version of the SNQ, in addition to nerve conduction assessments.7 The modified SNQ asked participants to provide the number of hours worked per week, number and type of patients seen per day, and the clock position predominantly used when providing care. Approximately 93% of respondents reported experiencing at least one MSD, with the 10:00, 11:00 and 12:00 o'clock positions identified as the preferred working sites for 69% of the respondents. However, there were no associations between the clock positions used and specific sites of reported MSDs. Horton et al. conducted an observational study by videotaping 8 final-year, New Zealand oral health students performing routine clinical dental hygiene procedures on patients.9 Approximately 31% of the "time in the mouth" was spent sitting in the 8:00-10:00 o'clock position, while 60% was spent sitting in the 11:00-1:00 o'clock position. However, the majority of students demonstrated poor neck and shoulder postures. Collectively, these studies infer that working from a seated position behind the patient may contribute to MSD development.
Dental hygiene educators, to date, are unaware whether or not the current academic approaches to operator ergonomics actually prevents or contributes to the development of MSDs over the course of a dental hygienist's career. While it is not possible to control for all of the non-modifiable risk factors for MSDs, dental hygiene educators should select training methods that have been documented to reduce occupational risks for injury. It is critical to identify which aspects of ergonomic training result in the most effective risk reduction. The purpose of this study was to investigate the extent of occupational MSD development based on the training approach used to teach operator positioning and assess the impact of MSDs on workforce issues among dental hygienists in the state of Mississippi.
Methods
A convenience sample of registered dental hygienists in the state of Mississippi was used for this study. Email addresses (n=1,553) were obtained from the Mississippi State Board Dental Examiners' dental hygiene licentiate renewal list for 2012. An invitation to participate in the study was sent to all Mississippi dental hygienists with an active license. IRB approval for the study was granted by the University of Mississippi Medical Center.
A 47 item, modified version of the validated Standardized Nordic Questionnaire (SNQ) was used as the survey instrument.32 The Standardized Nordic Questionnaire (SNQ) has been used worldwide to assess MSDs in a number of occupations, including dentistry.7,12-13,17,29,33 The SNQ is a standardized questionnaire developed for occupational health care service evaluation and to serve as an instrument for the screening of MSDs in an ergonomic context.32 The questionnaire includes a dorsal view diagram of the body with nine typical symptomatic areas of MSD development that are clearly shaded so that subjects can plainly view areas of interest. Specific modifications made to the instrument for the purposes of this study were the inclusion of survey items to assess demographics, practice history, educational training on operator positioning, and the impact of MSDs on workforce issues. Participants were provided the Center for Disease Control (CDC) definition of a musculoskeletal disorder on the questionnaire as a point of reference.34 Operator positioning was defined for study participants as 8:00-12:00/9:00-12:30 for right-handed operators or 4:00-12:00/3:00-11:30 for left-handed operators.
Twelve practicing dental hygienists representative of the target sample assessed the face validity of the modified instrument and 19 dental hygienists living outside of Mississippi conducted a pilot-test to verify functionality of the online survey mechanism. Data for this study were collected using Research Electronic Data Capture (REDCap).35 Consent for participation was indicated by clicking on the link to the survey embedded in the email invitation. Two reminders were sent, giving each licentiate a maximum of three opportunities to participate.
Descriptive statistics were used to analyze demographics, work history, and work habits. Chi-square analysis was used to determine the relationship between operator positioning and development of MSDs. Chi-square analysis was also used to determine the relationship between onset of MSDs and four identified workforce retention factors: modification of patient workload, reduction of work hours, taking time off from work, and the ability to continue to practice with a MSD.
Survival analyses were used to test onset of MSDs in relation to operator positioning. Survival analysis consists of statistical steps in which time until an event occurs served as the outcome variable of interest and is typically referred to as survival time.36 Onset ranges were identified as: immediately, 1-3 years, 4-6 years, 7-10 years, 11-15 and 16+ years and referenced as: immediate, 2 years, 5 years, 8.5 years, 13 years and 15+ years respectively. Censoring, in survival analysis, refers to those participants whose exact survival time is unknown. Participants who did not experience an event by the end of the study were considered censored (e.g. not included in the analysis). For example, in this study, a participant who did not develop a MSD by 15+ years was considered censored.
Kaplan-Meier log rank (LR) (Mantel-Cox) and Breslow (generalized Wilcoxon) survival test statistics were used to determine if there was an association between onset of MSD development and the operator position used to practice. Log-rank (Mantel-Cox) analysis compares two groups, weighs all time points the same, but places more emphasis toward the end of the study. Therefore Log-rank is more powerful for detecting differences in the survival probabilities later in the study.37 Breslow (generalized Wilcoxon) analysis is a variation of the Log-rank test. Breslow analysis places more emphasis at the beginning of the survival curve because more people exist at the beginning of the study, thus early occurrences receive more weight than the later occurrences.
The total number of years in practice before a MSD developed was the time event or onset. Statistical Package for the Social Sciences (SPSS) syntax was used to capture the time of event based on years of practice along with the participant's response to when a MSD developed.
All analyses were conducted using SPSS 21 (2012) statistical software.
Results
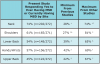
Three hundred and thirty-eight responses (n=338) were obtained for a 22% response rate. The respondents' demographic data were compared to data obtained from the American Dental Hygienists' Association (ADHA) annual practitioner survey conducted in 2016 to determine whether the study sample was representative of practitioners in Mississippi. According to personal communication with the ADHA Director of Research, the ADHA survey included 8,107 respondents nationally, with 64 reporting from the state of Mississippi. There were no significant differences in age, sex, employment status or hours worked (part-time or full-time). However, Pearson Chi Square analysis revealed a significant difference between the samples for work setting only, (p=0.005) with 70.5% of Mississippi hygienists in the ADHA sample reporting employment in a private practice setting versus 88.4% of the Mississippi hygienists in the study sample. As this study sought only hygienists who were currently in clinical practice, the analysis suggests that despite the low response rate, the sample was representative. In general, the majority of study respondents were female, 50% graduated prior to 2000 and 50% were between the ages of 20-39 years. Participant demographic data are reported in Table I.
The majority of respondents (72.5%) reported receiving didactic lectures on ergonomics in general while in school, but less than half (43.6%) reported having had lectures specific to MSDs. Over three-quarters (77%) were taught to use the 8:00-12:00 o'clock (front) operator position while 23% were taught to use the 9:00-12:30 o'clock (back) operator position. When responding to which position was primarily in clinical practice, nearly three-quarters (72%) of the actively practicing clinicians indicated the 8:00-12:00 o'clock position, while 28% used the 9:00-12:30 o'clock position. Reasons cited for changing positions were primarily due to workstation design (9.2%, n=31) and personal preference (9.5%, n=32). Only 4% (n=13) cited a health issue as a reason for changing position.
Pearson chi-square analyses revealed no significant difference (χ² (1) = 1.67, p=0.196) between those clinicians who developed and those who did not develop MSDs based on the clock position used in practice (Table II). However, further analysis of specific MSD sites revealed a significant difference between the position used and MSDs reported on after graduation for the upper back and wrists/hands. Dental hygienists who sat from 8:00-12:00 o'clock (n=84) were more likely to develop MSDs in the upper back (X2 = 8.09 (1), p<0.05) and in the wrist/hands (X2 = 8.29 (1), p<0.05) (n=104), when compared to those who sat from 9:00-12:30 o'clock (upper back: n=38; wrists/hands: n=52).
Using Breslow analysis, results also revealed a significant difference in early onset of MSDs and type of positioning used in clinical practice (χ² (1) = 3.92, p<0.05). Respondents reported developing a MSD at different times. Median time interval for a MSD to develop was 8.5 years for those seated at the 8:00-12:00 o'clock position versus 5 years for those seated at the 9:00-12:30 o'clock position.
However, after 15+ years of practice, the difference in time of MSD onset was not significant for practitioners using the 9:00-12:30 o'clock position (79%) when compared to those using the 8:00-12:00 o'clock position (85%) (LR analysis (χ² (1) = 2.13, p=0.144). Of the 244 participants using the 8:00 - 12:00 o'clock position, 79% developed a MSD from the beginning of practice to 15+ or more years of practice. Of the 93 participants using the 9:00-12:30 o'clock position, 85% developed a MSD within the same time period. Time of MSD onset by operator clock position is illustrated in Figure 1. Significant differences are identified at the 5-year mark; however, no significant difference is shown at the 15+ year time period.
Workforce issues included items related to modifying patient workload, reducing hours of work, taking time off from work and ability to practice clinically. The majority of practitioners (85%, n=231/272) responded that they are still able to practice despite having a MSD. Only 44 practitioners (13.1%, n=338) reported ever having to modify their patient load; 56 (16.6%, n=338) reported reducing work hours, and 72 (21.4%, n=337) reported taking time off from work due to MSDs. Pearson chi-square analyses revealed no significant difference between time of onset of a MSD and the need to modify the patient work load (X2 = 3.5 (1), p=0.06), reduce work hours (X2 = 2.97 (1), p=0.08), take time off from work (X2 = 1.96 (1), p=0.16) or the ability to continue to work (X2 = .00 (1), p=0.97) due to MSDs.
Discussion
The most remarkable findings in this study were that regardless of operator position used, the majority of respondents reported experiencing a MSD. Almost half of respondents had an onset of a MSD within the first 6 years of practice, and the majority reported that they were able to continue clinical practice despite having a MSD. Overall, the percentage of dental hygienists affected with and type of MSDs reported in this study are highly consistent with findings reported by others (Table III).1,3,5-7,16,17
Operator Positioning
Results from survival analyses revealed that study participants developed a MSD sooner after entering practice than what has been previously reported in the literature. In this study, almost half of the dental hygienists developed a MSD within the first 6 years of practice, as compared to findings from a qualitative study by Crawford, et al. who reported that physical aches and pain appeared more frequently after 10 years of practice.8
Breslow analysis demonstrated that the median estimated time to develop MSDs was 5 years for those who practiced from "behind" the patient as compared to the median time of 8.5 years for those who practiced "in front" of the patient. This analysis may be more reflective of the true timing of the onset of MSDs as it examined the MSDs as variables of time; for example, a clinician's increasing age and number of years in practice may further compound signs and symptoms of MSDs. These same variables also may explain why the Log rank analysis showed no difference in onset of MSDs and positions used at later time points. Early onset MSDs may be related to the adjustment period following graduation with factors including the need to maneuver in a new and different work environment, space limitations within the operatory, and adjusting to new equipment and/or equipment placement. Furthermore, recent graduates must learn to transition from the low patient loads of the academic setting to the significantly higher patient loads and increased physical demands of the work setting. Anecdotally, students tend to accommodate patient comfort before personal comfort. If this habit continues when transitioning to the work environment, new graduates may not realize how poor postures can jeopardize their future health.
Later onset may also be caused by the nature of cumulative trauma. When poor postures become the "normal" position, tissues change and adapt to the new position.38 These new postures/positions can become the "default" postures; however, the resultant complications from practicing with these postures may take years to develop into MSDs. This phenomenon is supported by findings from the Log rank analysis, which demonstrated that while study participants sitting in the back position developed MSDs at an earlier time point, after 15+ years, hygienists sitting from either position were highly likely to have developed MSDs. Data suggests that regardless of operator position used, given an adequate amount of time, a large percentage of dental hygienists are going to develop MSDs.
Work Habits
Surprisingly, only small numbers of hygienists who developed early or late onset MSDs reported modifying their workloads despite having a MSD. A previous study reported that 25% of study participants with MSDs modified their workloads; however, the time of onset was not identified.6 The need to reduce work hours in the present study was reported by 18% of those with early onset MSDs and 27% of those with late onset. Two other published studies documented similar percentages of respondents, 27% and 31% respectively, who needed to reduce work hours due to late onset MSDs.8,17
One quarter of the dental hygienists in this study reported taking time off from work due to early onset MSDs as compared to 33% with late onset. Previous studies reported that dental hygienists with neck and forearm pain were more likely to take off from work than those without pain.7,13,39 In this study, 24% missed work due to chronic musculoskeletal pain and only a very small percentage of dental hygienists were absent due to MSDs.
The majority of Mississippi dental hygienists who participated in this study with both early and late onset development of MSDs continue to practice clinically despite having MSDs. A qualitative study by Crawford et al. assessed reasons why dental hygienists continue to work with severe discomfort and pain.8 Reasons cited included financial obligations which prevented being absent, no sick leave, and fear of job loss if absent. It can be assumed that these identified reasons are similar to those of this study population. Although previous studies report that a number of dental hygienists with MSDs leave the profession due to physical stress, being adversely affected by discomfort, and neck and carpal tunnel pain,8,12,14 the data from this study suggests that the dental hygiene workforce productivity in Mississippi has not been negatively impacted by the presence of MSDs.
Results from this study suggest that existing approaches to operator positioning are insufficient to protect against future injury. In many dental hygiene programs, the greatest ergonomic training emphasis is placed on operator positioning; however, findings from this study do not support that one position is considered to be better than the other, as MSDs affected the majority of participants regardless of the chosen sitting position. Knowledge and mindfulness of proper body mechanics, such as sitting with more neutral postures in conjunction with regular movement and exercise, may be a more effective approach to training dental hygiene students.
Limitations in this study included that the working identified clock positions did not reflect the full variation in operator positioning. Although the 9:00 - 12:30 o'clock position eliminates the 8:00 o'clock position and slightly extends the 12:00 o'clock position, there may not have been enough of a distinct difference between the two working zones for participants to distinguish the difference or make a difference in the MSD rates due to the overlapping of these two zones. The use of a survey instrument dependent upon the participant's ability to accurately recall and report the events under investigation, has intrinsic limitations. Self-reported positions used while practicing could not be verified, and all responses are subject to recall bias. While it is assumed that respondents reported their typical operator position as requested, in reality practitioners often shift positions frequently while working, and this most likely occurred with these study participants as well. It was also assumed that participants provided their responses to questions about MSDs based upon their occupational risk and work habits. Injuries due to other causes, such as motor vehicle accidents, or pain and physical limitations due to illnesses or chronic conditions such as arthritis, could not be controlled for in this study.
It is important to note that many other factors can influence the development of MSDs, including the use of devices meant to assist with operator positioning, such as: custom stools, devices to assist with visibility and head posture (magnification loupes with/without headlamps), and instruments to reduce hand fatigue and physical demands on the operator (instruments with wide handles, power instruments, swivel cords). Exercise, including history of regular exercise and type of exercise regimen, may also be an important consideration for both the prevention and time to onset of MSDs among practitioners. To date, there is little evidence documenting the effects of these factors on either the development, prevention and/or reduction of MSDs in dental hygienists in clinical practice. Existing literature discusses the theoretical benefits of these interventions but there is a need for more definitive research assessing their impact on the long-term health outcomes and career longevity among practitioners.
To date, most ergonomics-related research has been conducted with dental hygiene students. It is imperative for researchers to conduct longitudinal studies on practicing dental hygienists working within the true clinical environment, using typical patient workloads and mimicking actual working conditions, so that identified behaviors leading to the development of MSDs can be adequately assessed and measured. While studies conducted on dental hygiene students have merit, these populations are often comprised of healthy young adults who are practicing under optimal conditions within the academic environment and treating a limited number of patients per day. Differences are most likely to occur between student populations and practicing clinicians.
Additional research also is needed to determine the significance of operator positioning on the development of MSDs. Specifically, studies are needed to examine whether working from a variety of clock positions (moving between 8:00 to 4:00 o'clock) would allow for operators to use different muscle groups and thus reduce musculoskeletal strain, and/or whether alternating between sitting and standing positions throughout the day can sufficiently break up the static postures associated with "sit down" dentistry. Prospective studies are also needed to explore how alternating positions in combination with exercise habits, stretching and/or use of ergonomic devices influences the development of MSDs in practicing dental hygienists.
Conclusion
Dental professionals are at high risk for developing MSDs due to positioning and repetitive motions that can lead to permanent tissue injury and chronic pain and dysfunction. Participants in this single state study developed MSDs earlier after entering clinical practice than what has been previously reported in the literature. Data from this study suggests that regardless of operator position used, over time, a large percentage of dental hygienists will develop MSDs. However, data from this study also suggests that the while the presence of MSDs may impact quality of life, they do not appear to negatively impact the dental hygiene workforce productivity in the state of Mississippi.
Acknowledgement
The authors thank Sunstar for their support of the World Dental Hygienists award program. This study was selected as the Sunstar 2017 best research project award and was presented at the IFDH symposium in Basil, Switzerland in June 2017.
About the Authors
Rebecca M. Barry, RDH, PhD is a professor and chair, Department of Dental Hygiene, University of Mississippi Medical Center, School of Dentistry, Jackson, MS; Ann E. Spolarich, RDH, PhD, is a professor and director of research, Arizona School of Dentistry and Oral Health, A.T. Still University, Mesa, AZ.
Mark Weber, PT, PhD, SCS, ATC, is the associate director, School of Physical Therapy, Texas Woman's University Dallas Center, Dallas, TX.
Denise D. Krause, PhD, is a former professor; William D. Woodall, PT, EdD, ATC, is a retired professor; Jessica Bailey, PhD, RHIA, CCS, is a professor and dean, School of Health Related Professions; all at the University of Mississippi Medical Center, Jackson, MS.
Corresponding Author: Rebecca M. Barry, RDH, PhD; bbarry@umc.edu
References
1. Gravois SL, Stringer RB. Survey of occupational health hazards in dental hygiene. J Dent Hyg 1980 Nov; 54(11):518-23.
2. Oberg T. Ergonomic evaluation and construction of a reference workplace in dental hygiene: a case study. J Dent Hyg 1993 Jul-Aug; 67(5):262-7.
3. Oberg T, Oberg U. Musculoskeletal complaints in dental hygiene: a survey study from a Swedish county. J Dent Hyg 1993 Sep-Oct; 67(5):257-61.
4. Barry RM, Woodall WR, Mahan JM. Postural changes in dental hygienists. four year longitudinal study. J Dent Hyg 1992 Mar-Apr; 66(3):147-50.
5. Osborn JB, Newell KJ, Rudney JD, et al. Carpal tunnel syndrome among Minnesota dental hygienists. J Dent Hyg 1990 Mar-Apr; 64(2):79-85.
6. Liss GM, Jesin E, Kusiak RA, White P. Musculoskeletal problems among Ontario dental hygienists. Am J Ind Med 1995 Oct; 28:521-540.
7. Anton D, Rosecrance J, Merlino L, et al. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med 2002 Sep; (42):248-257.
8. Crawford L, Gutierrez G, Harber P. Work environment and occupational health of dental hygienists: a qualitative assessment. J Occup Environ Med 2005 Jun; 47(6):623-632.
9. Horton SJ, Johnstone CL, Hutchinson CM, et al. Clinical working postures of bachelor of oral health students. N Z Dent J 2011 Sep;107(3):74-8.
10. Morse T, Bruneau H, Dussetschleger J. Musculoskeletal disorders of the neck and shoulder in the dental professions. Work 2010;35(4):419-429.
11. Werner RA, Franzblau A, Gell N, et al. Prevalence of upper extremity symptoms and disorders among dental and dental hygiene students. J Calif Dent Assoc 2005 Feb;33(2):123-131.
12. Akesson I, Johnsson B, Rylander L, et al. Musculoskeletal disorders among female dental personnel--clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health 1999 Sep;72(6):395-403.
13. Hayes MJ, Taylor JA, Smith DR. Predictors of work-related musculoskeletal disorders among dental hygienists. Int J Dent Hyg 2012 Nov;10(4):265-9.
14. Miller DL. An investigation into attrition of dental hygienists from the work force. J Dent Hyg 1991 Jan;5(1):25-31.
15. Krause DD, Frate DA, May WL. Demographics and distribution of dentists in Mississippi: a dental work force study. J Am Dent Assoc 2005 May;136(5):668-77.
16. Lalumandier JA, McPhee SD. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J Dent Hyg 2001 Spring;75(2):130-4.
17. Yee T, Crawford L, Harber P. Work environment of dental hygienists. J Occup Environ Med 2005 Jun;47(6):633-9.
18. Peterson SA. Clinical dental hygiene. 3rd ed. St. Louis: Mosby; 1968. 429p.
19. Cooper MD, Wiechmann L. Essentials of dental hygiene preclinical skills. Upper Saddle River: Pearson/Prentice Hall; c2005. 321p.
20. Millar D. Reinforced periodontal instrumentation and ergonomics for the dental care provider. Philadelphia. Wolters Kluwer Lippincott Williams & Wilkins; 2008. 41p.
21. Nield-Gehrig JS. Fundamentals of periodontal instrumentation and advanced root
22. Instrumentation. 7th ed. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins; 2013. 637p.
24. Wilkins EM. Clinical practice of the dental hygienist. 11th ed. Philadelphia: Wolters Kluwer Health: Lippincott Williams & Wilkins; 2013. 1189p.
25. Colangelo GA, Belenky MM. Performance logic. a new horizon in the delivery of dental care. Dentistry 1989 Apr;9(2):12-5.
26. Colangelo G, Belenky MM. Performance logic: A key to improving dental practice. J Dent Pract Adm 1990 Oct-Dec;7(4):173-7.
27. Murphy DC. Ergonomics and the dental care worker. Washington, DC: American Public Health Association. c1998. Chapter 11 Human-centered ergonomics: proprioceptive pathway to occupational health and peak performance in dental practice; p. 281.
28. Murphy DC. Ergonomics and the dental care worker. Washington, DC: American Public Health Association. c1998. Chapter 12 Optimizing dental operatory working environments. p. 306-8.
29. Schoen DH, Dean MC. Contemporary periodontal instrumentation. Philadelphia: W.B. Saunders Company; 1996. 246p.
30. Rucker LM, Sunell S. Ergonomic risk factors associated with clinical dentistry. J Calif Dent Assoc 2002 Feb; 30(2):139-148.
31. Chaikumarn, M. Working conditions and dentists’ attitude towards proprioceptive derivation. Int J Occup Saf Ergon 2004;10(2):137-146.
32. Sunell S, Maschak L. Positioning for clinical dental hygiene care: preventing back, neck and shoulder pain. Probe 1996 Nov-Dec;30(6):216-9.
33. Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987 Sep;18(3):233-7.
34. Rundcrantz BL, Johnsson B, Moritz U. Cervical pain and discomfort among dentists. Epidemiological, clinical and therapeutic aspects. Part 1. A survey of pain and discomfort. Swed Dent J 1990;14(2),71-80.
35. Elements of ergonomic programs. [Internet] Atlanta: Centers for Disease Control and Prevention, National Institute of Occupational Safety and Health; 2017 [modified 27 July 2017; cited 20 Nov 2017] Available from: https://www.cdc.gov/niosh/topics/ergonomics/ergoprimer/default.html
36. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009 Apr;42(2):377-81.
37. Kleinbaum DG, Klein M. Survival analysis: a learning text. New York: Springer; 2012.
38. Lang TA, Secic M. How to report statistics in medicine. Philadelphia: American College of Physicians; 2012.
39. Langford ML. Poor posture subjects a worker’s body to muscle imbalance, nerve compression. Occup Health Saf 1994 Sep;63(9):38-40, 42.
40. Chismark A, Asher G, Stein M, et al. Use of complementary and alternative medicine for work-related pain correlates with career satisfaction among dental hygienists. J Dent Hyg 2011 Fall; 85(4):273-284.