You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The ADAA has an obligation to disseminate knowledge in the field of dentistry. Sponsorship of a continuing education program by the ADAA does not necessarily imply endorsement of a particular philosophy, product, or technique.
Successful Management
The secret to success in dental practice administration is to maintain a balance between achieving assignment goals and developing and cultivating the relationships that support the philosophy of the dental practice. A competent practice administrator is likely to increase independent actions and decision-making by each team member through delegation of tasks and using positive feedback.
Personnel management is a mystery for many dentists, which is why they employ practice administrators. Recruitment and retention of qualified team members can be a challenge. At times the job market may be flooded with candidates, while at other times there is a severe shortage of qualified candidates. As a result, retaining current valued team members is important.
Successful management can be attributed to five key areas: delegation, respect, empathy, acknowledgement, and compensation.
Delegation to a team member is a must if the dental practice is going to be successful. A team member should be assigned all responsibilities that are legally delegable and for which they are properly trained. Team members cannot achieve their maximum potential and productivity if they are not given responsibility for tasks they are qualified to perform. Some practice administrators have a difficult time with the delegation of tasks. Accountability symbolizes a function or obligation to the practice and the employing dentist. If responsibility is withheld, then it can be assumed incorrectly by the employee that the employer or practice administrator does not feel the team member is capable of the task, and may seek employment elsewhere. If a team member is valued, concern should be given for retaining this employee.
Respect is an earned admiration given from one to another individual. Each member of the dental team must respect another's education, expertise, and standards. Lack of respect indicates a lack of confidence and can reflect poorly on the administrator, dentists, or practice as a whole. Each member has a key role on the dental team and should possess expert skills and credentials that warrant respect and positive attitude toward another individual's potential and accomplishments.
Empathy is the emotional relationship that exists among the dental team members. Each dentist sets the tone for the relational bond in the practice. Empathy includes good rapport between members of the team and is conveyed to the patients who recognize how well the team members work together during tense times and how they enjoy each other's professional friendship. Proper communication is a must for conflict resolution and is often practiced during department and team member meetings.
Acknowledgment of a job well done or special achievements is appreciated by all team members and dentists alike. It is human nature to want to succeed and the driving force is acknowledgement. Appreciation can come in the form of verbal praise, a sign recognizing employment and credentials, or a financial award for outstanding service or creativity. For many, a simple “thank you” will go a long way. It is important for the administration to verbalize appreciation on a regular basis; without it, team members may begin to feel that they are being taken for granted.
Compensation is a rewarding form of recognition for achievement. Most team members say that they are willing to work hard if they are compensated for their efforts. Compensation must be based on education, merit performance, longevity with the practice, and cost of living. Dentists who affirm employees with applicable compensation also tend to delegate responsibility, create a good atmosphere in the practice, and respect and acknowledge their employees.
Satisfied team members are provided compensation monetarily, for example, through periodic salary increases, reimbursement of licensing/registration/certification fees, professional association dues, paid holidays, paid time off, and continuing education reimbursement. Team members must know their worth and practice administrators and dentists must be willing to pay for excellence.
Performance Evaluation Procedures
The task of providing performance evaluations for many dentists and practice administrators can be difficult. However, a performance evaluation can be one of the most positive and proactive tools administrators can use to communicate with staff. Performance evaluations are indispensable, both for reinforcement of positive actions as well as to provide constructive criticism in areas of deficiency.
The following suggestions may help in making this often difficult task less tedious.
• Evaluate all year long by involving the team member in regular conversations about what he or she is doing within the practice, even if informally. It is important that the team member is aware of the interest in his or her work.
• Frequent evaluations prevent problems before they arise and reinforce positive attitudes and behaviors. When performance evaluations are given on a regular basis, small mistakes can be discovered before they develop into big problems. Team members are more likely to come forward with issues of concern if there is an air of open communication.
• Document, document, document. Document all positive and negative performance issues. It is unwise to rely on memory when it is time to write the evaluation. If a team member asks for examples during a negative evaluation, the rationale provided must be accurate and complete. Documentation will ensure that the administrator is not discriminating against this individual. This is especially important if a team member is terminated and legal action is sought at a later date.
• Involve the employee during the evaluation. Having each employee complete self-evaluations is a meaningful way to involve team members and give them the opportunity to think about their own work performance. Recently hired team members may need encouragement to develop goals and values for job performance, while experienced team members may need to reaffirm their goals and values. Some practices establish written agreements and commitments with their team members about the practice's goals and objectives for each employee to accomplish over the next year. The written document is completed and signed by the employee and either the dentist or the practice administrator. A copy is given to the team member and included in the employee's file.
• When evaluating work performance, it is important to actually evaluate the job performed and not the individual. Work performance must be based on predetermined goals, objectives, and standards. Provide specific examples of where the team member succeeded or failed to meet these goals, objectives, or standards. Clinical team members will have different sets of goals, objectives, and standards than administrative team members; however, some of the goals and objectives will overlap. It is important to address issues other team members may have with the team member's performance without disclosing the accuser. Each team member's performance within the practice will impact the entire team and practice as a whole.
• Close the evaluation on an upbeat, positive note. Spend quality time with the team member until an agreement is reached on each point in the performance review. This becomes extremely important when the performance evaluation is less than satisfactory and if the team member has failed to meet practice expectations. During a negative evaluation review, it is important to always document points discussed and have documentation on hand to corroborate the evaluation, particularly if the practice administrator expects to conclude the review with something constructive to say about the goals identified to be achieved before the next review.
Team Member Search
From time to time, staffing changes will occur. Examples include employees wishing to only work part-time, leaving to pursue other avenues in dentistry, moving from the geographic area, the addition of an associate dentist, or the need to terminate a team member. An active dental practice administrator will often have the time-consuming tasks of interviewing, hiring, orienting, evaluating, and the termination of staff members. These can be complex tasks and the administrator must be well equipped to understand job-related activities; state laws, required credentials, and education needed; recognize local and national salary scales; orient the new team member; and provide objective evaluations. Staffing is a fundamental responsibility for practice success and requires a great deal of skill and deliberation.
Writing an Opportunity Advertisement
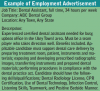
The first impression conveys a great deal about a dental practice. Carefully wording an employment advertisement is an opportunity to make a high-quality first impression that will attract the best candidates. The advertisement should describe the required competencies and identify key benefits of the position (Figure 1). Many dental practices may utilize their local or state organization's placement services while other dental practices use online classifieds or the traditional newspaper classifieds, while still others may use formal employment websites (such as dentalworkers.com, ihiredental.com, dentalpracticeworkers.com, and careerbuilder.com). In every one of these cases, the dental practice must strive to create specific qualifications for the position to gather as many qualified applicants as possible.
While advertisements seeking an inexperienced individual will most likely receive more responses, advertisements listing specific qualities the practice is seeking will help narrow the candidate pool and save the interviewer valuable time.
Job Descriptions
An up-to-date, accurate job description for each of the positions in the dental practice should be included in the practice procedural manual. These job descriptions will assist employers in telling prospective employees what will be expected of them on the job and will aid in training new team members.
To write a job description, a job analysis needs to be conducted. A job analysis involves observing each position and gathering information about that particular position. Some job descriptions include the following information:
• Definition of the job position (e.g., business assistant, clinical assistant, expanded duties experience, credentials needed, treatment coordinator, hygienist)
• Tasks that make up the job (daily, weekly, monthly, quarterly, annually)
• Skills needed to perform the job adequately
• Personality characteristics the practice desires
• Educational background needed for satisfactory job performance
Once the description is written, allow the current employee(s) to review the description for any duties/activities that may have been overlooked or misconstrued. Revise the description as necessary and place it in the practice procedural manual. An outline for a job description given to a prospective candidate should also include salary range and available benefits.
Hiring Process
There are several legal factors to be considered upon hiring an individual. These include: application forms, citizenship status, and testing in some cases. An employer must ensure that all application forms avoid any questions regarding age, marital status, race or ethnicity, and do not violate any state laws. In addition, each candidate must complete the same application form to avoid any type of discrimination.
Interview Process
Before conducting any interview, gather all information about each candidate, develop an outline of questions, and determine the interview's location. Figure 2 describes key points to consider when preparing for an interview. When the interview begins, the interviewer should establish rapport with the candidate by introducing oneself and creating a sense of cordiality. The process may begin by explaining a bit about the dental practice and the purpose of the interview to generate a relaxed atmosphere. During the interview process, the candidate should be encouraged to participate actively. The main component of the interview process consists of posing questions, listening to the responses, replying to questions, and providing transition from one discussion topic to another. Use various types of questions to gain insight into each aspect of the candidate's work ethic and ability to fit within the practice.
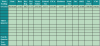
Types of questions asked during an interview process include: direct, indirect or open ended, and/or hypothetical (Table 1). The direct question will generally elicit an expected response. An indirect or open-ended question requires the candidate to expound beyond a “yes” or “no” on the answer. A hypothetical question typically involves a scenario and requires the candidate to respond accordingly. Interviewers usually favor hypothetical questions because the responses offer insight into the candidate's thought processes and problem-solving skills.
The interviewer has two main responsibilities: 1) to gather information about the candidate's qualifications for the position in a nondiscriminatory manner and 2) to convey information to the candidate about the practice, specific job responsibilities, and expectations. The first task is achieved by being aware of certain legal considerations and keeping questions and discussion relevant to the position. When asking interview questions, consider the following suggestions:
• Ask only for information that is intended to be used to make hiring decisions.
• Know how the information will be used to make a decision.
• Recognize that it is difficult to defend the action of seeking information unrelated to the job description.
Guidelines of the United States Department of Labor and EEOC (Equal Employment Opportunity Commission) prohibit discriminatory hiring based on race, creed, color, sex, national origin, handicap, or age. Questions related to any of these as well as marital status, children, ownership of a house or car, credit rating, or type of military discharge can also be considered discriminatory. Questions that should and should not be asked during interviews include many of those shown in Figure 3.
Before concluding the interview, the prospective candidate should be informed of:
• Specific job responsibilities
• Beginning employment date
• Orientation procedures
• Opportunities for advancement (if any)
• Practice policies
• Professional responsibilities
• Work hours and days
• Salary
• Benefits (vacation, holiday pay, sick pay, etc.)
• Continuing dental education
• Health insurance waiting period
As the interview process begins or concludes, it may be an appropriate time for the candidate to tour the office depending on the schedule of procedures. This may also be a good time, if convenient, for the rest of the dental team to meet the candidate. At the conclusion of the interview, inform all candidates of the plans for hiring determination and the date by which the decision will be made.
Some practices find it useful to conduct a “working interview.” The prospective candidate would return and actually spend time shadowing the position for which they are applying. This is a method used to access their skill level and see how the candidate interacts with other team members. If the candidate is actually working with the dental team, he/she is often paid as a substitute according to the standard office wages.
Employment Agreement
Once all prospective candidates have been interviewed and a decision is made, the candidate to be hired should be contacted promptly and offered the position. A formal letter defining the terms of employment should be drafted for the new team member stating the conditions of employment such as salary, work hours and days, beginning date, and other conditions agreed upon during previous discussions. The letter should identify probationary periods, which allow either party to terminate employment within an established period of time without fear of consequence. It is wise to have the employee sign the letter and give the employee a copy for his or her personal file; a copy is also placed in the employee file in the practice. A courtesy letter should also be sent to candidates not being hired and their applications may remain on file if desired. Some practices choose to notify by a telephone call. If this method is chosen, the candidate must be addressed directly. Do not give employment information to anyone else without the written consent of the candidate. The candidate should have been informed during the interview process how and when he/she will be notified.
New Employee Orientation
A well-organized dental team will provide a smooth transition for the new team member into the practice. It is important to document any necessary continuing education or health information concerning this new employee. Emergency contact numbers, critical health information, and formal government paperwork regarding salary should be completed and kept in the employee's new record. Each employee should be current in CPR certification. A date of expiration on the CPR card will document when the person must recertify. It is required that the new employee learn about the protocols established by the office; such as where the first aid kit and safety data sheets are kept. (This will be discussed in more detail later in the “records” section.)
It is also important for the existing team members to know about the orientation process for the new member. Time needed for the new team member to become well established in the office will vary according to the individual's previous experience in a dental practice and the individual's learning curve. Many dentists believe that it takes six months for an inexperienced clinical assistant to fully fit into a practice, a little less time for the dental hygienist because of his/her independent and repetitive work schedule, and varied times for administrative team members depending on previous experience and knowledge of dentistry and computer software. It is important for the practice administrator to set aside adequate and uninterrupted time for the orientation. Among the many activities involved in new team member orientation, find time to perform the activities in Figure 4.
Many practices offer a probationary period in which the new team member may begin at a lowered salary and after ninety days of satisfactory work performance a higher salary will go into effect. During the probationary period it is important to identify areas of strengths and weaknesses in the new team member. Some individuals may already know their areas of deficiency and assets, while others may need some guidance. Positive reinforcement for both strengths and weaknesses is necessary to create confidence in the new team member. However, poor performance should be corrected immediately to avoid implicitly supporting substandard work. It is easier to correct poor habits early in employment rather than later, when it seriously affects the practice as a whole. Additional training outside the practice may be needed in some instances and can be gained from texts, journal articles, ADAA Continuing Education Courses, and professional programs from a nearby accredited dental education program.
Once the new team member has settled in after the probationary period, it is important to evaluate performance on an ongoing basis, allowing room for improvement when needed. It is customary in the first year of employment to take evaluations every three months in order to provide feedback to the new team member. At the year anniversary, or when entire staff reviews are done, it is important to review progress with adequate benefits or salary increases. If all efforts to improve the team member's performance have failed, it is wise to terminate the employee promptly rather than to continue with substandard performance, which can affect overall team morale.
Employee Termination
There is no easy way to terminate a team member and this decision should be chosen after careful deliberation. Many practice administrators, especially inexperienced ones, fail to terminate an employee until it is long overdue and team morale is jeopardized. Many dentists avoid the issue all together and delegate the responsibility to the practice administrator. By carefully working with a team member many performance deficiencies can be resolved. If a team member shows poor work habits, has substandard skills, or exhibits problems during the provisional employment time, there should be no hesitation to terminate this team member. Maintaining proper documentation is crucial when tracking employee performance issues.
Termination issues often involve the dentist. If it is a clinical team member with unsatisfactory work habits, it is usually the dentist's decision to terminate. When it is an administrative team member, the practice administrator will bring it to the attention of the dentist. If termination is being considered it is important to consider any potential ramifications and legal responsibilities that may affect the practice.
If termination is selected it is important to stick to the decision and determine a termination meeting date and time. Some practices wait until the end of the day on the last day of the work week; others will pick a time convenient to the dentist's schedule. It is sensible to include only the direct supervisor and the dentist in this meeting. Inform the team member in question politely that a matter must be discussed with him or her and begin the meeting. It is essential to be prepared with documentation and be able to show justifiable documentation of specific poor performance that is cited in the performance evaluations. Documentation should also include that the employee was given written documentation of this performance and opportunities to improve. All documentation should be signed and dated by the employee and practice administrator. This shows a timeline and that the employee was aware of the situation. Review the main reasons for the termination, summarize the efforts that have been made to assist the team member in improving skills or attitudes, and give a check for any monies due. When severance pay is being offered, a forfeiture document is prepared for employee signature, and the severance pay given to the employee. Explain any future work opportunities and gather any materials (keys, communication devices, etc.) belonging to the practice from the employee. As long as the employee maintains control of emotions, extend to him or her every reasonable courtesy. If the employee does lose control and becomes verbally abusive ask him or her to vacate the practice immediately.
Termination is one of the most difficult duties of a practice administrator and remaining calm and keeping emotions in check can be challenging. It is often in the best interest of all parties to have a witness to the procedures who can sign and verify that all issues were addressed and no foul play was involved. Actions, agreements, and outcomes must be documented and retained in the personnel files, as any dentist or practice administrator must consider the very real risk of a lawsuit when terminating an employee. To make potential litigation by a former employee less likely, it is imperative to abide by the law to avoid discrimination suits. When handling reference calls for such an employee, avoid future problems by only confirming dates of employment. Explain to the caller that it is practice policy to only confirm dates of employment. Any further information can place the administrator or the practice at risk.
Management of Grievances
Conflict is normal between a dentist or administrator and an employee. However, alarm would be warranted if numerous complaints are made, as this may indicate a more serious problem. There are two types of conflict that are present in every dental practice from one time to another, unnecessary conflict and resolvable conflict.
Unnecessary conflict appears when individuals have different opinions, lack of or inaccurate information, or antagonistic feelings that can appear unexpectedly, causing disagreements and poor morale. This can grow into a full-blown conflict if signs are not noticed early enough and if action is not taken. These conflicts often occur due to gossip. This is frequently seen between the clinical staff or between the clinical and administrative staff.
Resolvable conflict occurs when two team members' perspectives on a particular issue are initially seen as opposing but are actually based on different desires, goals, standards, or interests that must be understood and worked through to their mutual agreement. Examples of this type of conflict can occur when a team member does not understand the importance of punctuality, wants to or “needs to” leave early frequently, does not think the salary is fair, or has no concept of the goals or objectives of the practice. It is important to observe and recognize nonverbal signals that people are distressed or overwhelmed. Some of these cues are deep sighs, tense shoulders, crossed arms, lack of eye contact, extreme quietness or moodiness, and/or sarcasm.
The practice administrator should review the particulars of every grievance and seek to resolve the problem as quickly as possible. If delayed too long, the situation may result in additional conflict, or may be interpreted as disinterest or being unworthy of time on the part of the administration. It is important to listen patiently to all the issues while keeping an open mind. In doing so, the office manager can gain the team member's confidence by encouraging the person to talk while at the same time indicating fairness in resolving the issue. It is very important to identify the real underlying issue. Frequently, a grievance is made about a problem, when in reality a deeper concern is the real issue. For example, a person may be complaining about unfair work assignments, when actually the source of the problem is the punctuality and early departure of another team member.
Employee grievances are not easy to manage and exercising self-control is a must. It is the practice administrator's duty to avoid taking sides in personality conflicts between the complaining team members. It is important to avoid any delay in decision making since the dental practice is a comparatively small business organization and allowing a conflict to go unresolved can create additional tension and undue stress on the entire team. However, emotional outbursts generally do not lead to constructive resolution of any problem. Should this occur, it is wise to stop the meeting until a future meeting can be scheduled where the problem can be further discussed in a composed manner. If it is necessary to delay a decision, and at times it is, let the involved member know the status of the problem and that it will be resolved as quickly as possible.
Conflict Resolution
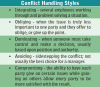
There are five basic types of conflict resolution. Depending on the type of conflict a dentist or office manager may choose to handle each situation differently.
Conflict does not only occur between team members, it can occur between a patient and a member of the dental team. The most important person in a dental practice is the patient and this is often forgotten. Without the patient, there would be no need for the practice or for the team to report to work. Many of the concepts provided above are effective when managing patient grievances. Yet again, do not overlook the fact that each patient comes from a different background and has different wants and needs. While communicating with patients it is important that practice administrators and the entire dental team recognize each patient as an individual with specific needs and that the practice must determine how to be sensitive to those needs. Dentistry is a service profession and each team member must make every effort to ensure the patient's distress is alleviated and the patient is taught to help him or herself.
Record Keeping of Grievances
With any type of grievance, it is important to maintain a record. Documentation of meetings or discussions is helpful should future conflicts arise over the same problem. It is impossible for the administrator to recall all of the issues concerning an incident; therefore, information should be retained in the employee file or appropriate area for future reference should the need arise.
Communication
Basic communication occurs when someone (the sender) has information (the message). This message can be communicated through verbal, written, or non-verbal ways (the medium). Another person (the receiver) is given this message and interprets it by offering some kind of response (feedback).
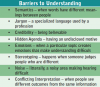
An administrative assistant or office manager must be able to communicate messages clearly. Non-verbal cues, gestures, and tone of voice can all lead to proper and improper interpretation of the message (Figure 6). During a time of conflict or an emotional situation, understanding may be more difficult to attain.
Types of Communication
Four basic types of communication exist in the dental practice. Upward communication takes place when an employee is voicing opinions or concerns to the dentist or office manager. Downward communication reverses those positions and takes place when information or directives are being announced to the staff. Horizontal communication occurs when people at the same level are communicating; say in the case of two or more chairside assistants or partnering dentists. The final type is known as informal, or the “grapevine.” The dentist and office manager should listen to what is being said informally and possibly address points of concern during team meetings.
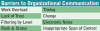
Barriers to Organizational Communication
Several barriers exist to good communication. If a barrier exists it is important to try and overcome it to be sure that communication is received and understood. An obvious barrier is machinery noise. It can be difficult to communicate over the sound of a handpiece or when standing near the lab or compressor.
When an assistant is overloaded with extended daily duties it may be difficult to convey the importance of the message. Timing refers to finding the best times in the day or week to offer information that allows for comprehension and possible questions.
Some employees find it difficult to accept change. Information regarding changes in office or clinical policies may not be easily accepted. It is important in this case to offer clear and complete information, and allow for questions and answers. If a lack of trust exists either from the sender or from past experiences the information may not be accepted as truthful in part or in whole.
Some people may not work well with authority figures. They may perceive the office manager to be using their rank or status within the group to meet their own personal gains. It is important that the position and span of authority be clear to all employees, and the manager should articulate the duties to the staff and maintain professional boundaries.
Finally, information that has been offered and then repeated several times may eventually become filtered or embellished. It is important that all policies be discussed often, that informal lines of communication are monitored, and that all parties be made comfortable to discuss matters during team meetings (see Figure 7).
Team Meetings
Regularly scheduled team meetings should become a regular part of the dental practice. More and more practices are opening the day with short staff meetings called “morning huddles,” allowing each team member to categorize the tasks for the day, assess issues that need to be resolved, and maintain open communication. With more frequent meetings, issues can be addressed more quickly and the need for lengthy meetings can be eliminated. Some practices hold department meetings bimonthly to address issues pertaining to each department. When the issues brought forth impact the entire practice, information is brought to a staff meeting. It is still sensible to maintain a longer meeting time to evaluate technology updates, goal revisions, or to do short- and long-range planning during an all-staff meeting. The staff meeting provides an excellent opportunity to define and review the goals for the practice, as well as an opportunity to brainstorm for marketing. While criticism may be part of a staff meeting, such a meeting should not be designed as a grievance session.
The time and length of the all-team meeting will vary, according to the needs of the practice. Some practices schedule one or two hours per week or once a month, while others may close the practice for a half or a full day for an intensive session, and still others find luncheon or breakfast meetings very effective. Team members typically know of the meeting date and time well in advance of the meeting. Patients are not scheduled during this time, and some practices require non-scheduled team members to come in on their day off for these meetings. Most meetings of this type are held during normal, working hours. An agenda may be used in planning and will serve to expedite the business objectives of the meeting. Agenda items may be suggested by the dental team or brought forth from departmental meetings. The practice administrator should review outcomes of the meeting and provide typed minutes to the dental team. It is important to maintain a strict meeting schedule, as everyone's time is valuable, allowing all who wish to address issues or to speak the opportunity to do so.
Guidelines Affecting Management of Personnel and Practice Records
Types of employment records required to be kept in dental practice personnel files vary from state to state. For most states if the employee has direct patient care, copies of licenses, registrations, and certifications should be in the file. Originals are displayed in visible areas where the dental team member will be working. For employees working directly with money or access to patient credit cards, a background check is often completed. Some practices will have these team members bonded to help protect the practice.
All U.S. employers must complete and retain Form I-9 (downloadable from IRS.gov) for each individual they have hired for employment since November 6, 1986, including citizens and non-citizens. The employer must verify the employment eligibility and identity documents presented by the employee and record the document information on the Form I-9. The law requires employers to maintain I-9 records in their own files for 3 years after the date of hire or 1 year after the date the employee's employment is terminated; whichever is later. This means that Form I-9 needs to be retained for all current employees, as well as terminated employees whose records remain within the retention period.
There is no fee for completing a Form I-9. Form I-9 records must be retained by the employer and made available for inspection by U.S. Government officials as specified in the USCIS Privacy Act Statement. Note: U.S. immigration law does not prescribe or proscribe storage of a private employer's I-9 records in employee personnel files. However, as a practical matter, and particularly if a large number of employees are involved, it may be difficult to extract records from individual personnel files in time to meet a 3-day deadline for production of I-9 records for official inspection. A new employee must verify and sign Section 1 of a Form I-9 no later than close of business on the first day of work and Section 1 should never be completed before the employee has accepted the job offer. The employee's signature holds him/her responsible for the accuracy of the information provided.
The employer is responsible for ensuring that the employee completes Section 1 in full. A list of acceptable documentation from the employee is attached to the form but employers cannot specify which documentation(s) they will accept from an employee. (see Appendix 2, Figure 17).
OSHA/State Compliance
Each state may have different compliance rules and regulations for OSHA. Each state's board of dentistry or board of dental examiners may also have state specific rules and regulations for exposing radiographic images. For employees with direct patient care, there are specific federal guidelines that are covered in section XIV under infection control.
In the states that do require continuing dental education as part of credentialing, it is often the individual team member's responsibility to keep track of deadlines and the number of credit hours earned. Some dental practices provide continuing dental education on a regular basis as a benefit to the team members.
Other Employment Records
Employee financial records such as time cards/sheets, merit increases, bonuses and vacations paid out are generally retained for seven years, as with most financial records, although some dental practices keep the records indefinitely. Tax preparation materials for each employee employed within the practice also are generally retained for a minimum of seven years. Always check with current state and federal regulations on these time requirements.
Payroll
Prior to beginning payroll, the practice needs an employer identification number. The dentist, as the employer, must apply for an employer identification number assigned to sole proprietors or corporations for filing and reporting payroll information. This is a nine-digit identification number unique to the practice and can be obtained by applying on Form SS-4 (Appendix 3, Figure 18). This form can also be completed online. Complete information on all IRS tax requirements and forms can be found at the IRS website - http://www.irs.gov/pub/irs-pdf/p15.pdf. Illustrations of most tax documents can be found in Part 8 of the Handbook for Employers available through the IRS.
Every dental practice has a system to administer payroll to its employees. Some dental practices do payroll in-house, while others choose to have an outside company keep track of the records and supply the practice with earning and deduction information. The dental practice must maintain each employee's record of earnings, including a summary of information for each employee.
The employee's record of earnings should contain the following information needed for various state and federal reports:
• Name, address, Social Security number, rate of pay, withholding exemptions claimed, marital status, and any special deductions such as insurance, retirement, or other accounts.
• The number of pay periods in a quarter and the date on which each pay period ends.
• Columns for regular earnings, overtime earnings, and total earnings.
• A column for each deduction and total deductions.
• A column for entering the net pay received after all deductions.
• A column for providing accumulated taxable earnings, Federal Insurance Contributions Act (FICA), and taxable wages for unemployment taxes.
• Columns for quarterly and annual totals.
Determining Wages
The dentist or practice administrator and the team member must reach an agreement on an acceptable wage. This wage may be determined as an hourly rate, weekly rate or a monthly amount. After the pay rate has been established, the procedure must be decided for determining net pay.
Regular hours are usually hours worked between 32 to 40 hours in a given week. Overtime hours are anything in excess of 40 hours in a given week. Pay for regular hours worked is figured by multiplying the pay rate by the number of regular hours worked. Overtime hours are figured by multiplying the number of overtime hours worked by 1.5 times the pay rate. Some dental practices may not pay overtime wages but instead offer “comp.” time or allow the team member to flex extra time during the pay period.
Federal regulations mandate that an employer make certain payroll deductions and that the employer also pays certain payroll taxes. Information pertaining to these guidelines can be found in the booklet issued by the Internal Revenue Service entitled Circular E. Most state tax bureaus publish a similar booklet on state taxes that must be withheld. Income tax deductions depend on the number of exemptions the employee indicated on Form W-4. An example of a W-4 can be found at: http://www.irs.gov/pub/irs-pdf/fw4.pdf (Appendix 4, Figure 20). The amount withheld in taxes is determined by the table in the Employer's Tax Guide - Circular E - http://www.irs.gov/pub/irs-pdf/p15.pdf.
The practice administrator in most dental practices is delegated to handle payroll by the dentist. The federal government requires that each employer maintain records on each employee for the number of hours worked (regular and overtime), the amount paid out to the employee, number of exemptions, and the amounts deducted for tax purposes. Complete and accurate records are mandatory for each employee, with previous records stored by year with the practice's other financial papers. A separate payroll sheet is maintained on each employee that lists records of pay rate changes, gross earnings before taxes, and each amount and type of deduction (see Figure 8). A withholding statement is supplied with each payroll check for each employee, providing the employee an explanation of all deductions and amount earned.
Other Duties Delegated by the Owner/Dentist
Delegation of duties to the practice administrator can vary greatly from one practice to another. In some dental practices, the dentist's spouse may have a key role in the day-to-day business dealing and decisions of the practice, while in other practices it becomes the role for the practice administrator to do or delegate as necessary.
Public Relations Activities
Another area of practice administration may be the development of public relations and marketing for the dental practice. There is a wide variety of opportunities for marketing, but the most common include direct marketing with promotional services, word of mouth referral, and a website.
With technology usage increasing, one of the best ways to advertise a dental practice is through a website. This is an area in which a small monetary investment will pay off in the long run. Patient wants and needs can change at a fast pace. Accessibility and visibility are essential when marketing the dental practice. With the use of a practice website, patients and potential patients are able to view treatment options and services offered, schedule appointments, and view and manage their accounts in some cases. Many practice websites offer a practice e-letter sent out to patients who choose to subscribe. It is a wonderful and effective marketing tool.
Practice Procedure Manual
Development and maintenance of an office procedure manual may be part of the practice administrator's responsibility. This manual will need to be updated along with changes in technology or in the scope of practice for allied dental personnel.
A practice procedural manual lists all of the policies and regulations of the dental practice. The manual should be accessible to the entire dental team, in the event a question regarding some aspect of protocol arises. Common areas covered in the procedure manual include:
• Objectives and practice philosophy
• Hours of operation
• Holidays the practice is closed
• Holidays paid
• Vacation protocol, including accruement rate
• Sick policies
• Team meeting protocols
• Internet/telephone usage
• Dental services/fees to employees
• Dental services/fees to employee's immediate family
• Bereavement policy
• Jury duty policy
• Resignation/termination procedures
There may be a practice instruction manual for each position within the practice. Often, this manual is used as an adjunct in training and orientation of a new team member. Instruction manuals will list the objectives of each position and, in some cases, outline in detail specific steps for some of the duties delegated to this position.
Practice Equipment
Practice administrators are often the delegated employees to select, requisition, and purchase business equipment used in the administrative areas of the practice. In addition to the above duties, practice administrators normally maintain the equipment purchase records, warranty, and maintenance files. Dental equipment maintenance files are kept in separate folders from business equipment files. Following manufacturer's instructions and regular maintenance of equipment aids in its efficiency and longevity, and is the best way to avoid major problems. By adhering to a routine schedule for preventive maintenance, the warranty will not be voided and the life of the equipment will be extended. Use, care, and cleaning instructions should be kept in a central location or they can be kept in a location near the piece of equipment. The delegated team member should keep a maintenance log, or record of routine maintenance, for those pieces of equipment for which it is appropriate. When equipment does not function properly, a service call will need to be placed to inspect and rectify the problem.
Team Responsibilities
As an office manager, it is important to understand the role of each person should a problem occur. Advocating for the continuing education of the dental team concerning the signs and symptoms of the various forms of abuse and neglect will potentially protect the patients and office alike. To avoid possible legal dilemmas the whole dental team must be aware of their responsibilities to the dental patient.
Responsibilities of the dental team include:
• First and foremost, the dental team has a duty to treat the patient by providing all of the appropriate treatment required by the patient, including transfer to a medical facility when warranted.
• Second, the dental team must not abandon the patient. The dental team must not allow a patient to leave the office until they are confident the emergency situation is resolved. If medical assistance has been summoned, emergency care must be provided while waiting for medical assistance to arrive.
• Third, the dental team must be prepared for any emergency in the dental practice. This means they must have:
• Current training in CPR
• Emergency equipment available, including an oxygen tank and a complete emergency kit
• Knowledge of how to use emergency equipment
• The ability to accurately obtain and record vital signs
The dental practice must also:
• Use contemporary dental techniques
• Maintain current health histories on all patients
• Establish an emergency routine and regularly practice this routine with all dental team members
• Maintain all emergency protocols in writing
• Maintain a current list of emergency phone numbers easily accessible to the individual designated to call for medical assistance
Standard of Care
Standard of care is generally misinterpreted within the dental profession. Many believe that it is a state law or set of regulations listing specific steps a dentist must follow. It is not a state law or regulation, but a legal concept that provides common limits that a dentist must comply with in a given situation. The standard of care that a dentist must meet is the practice of highly regarded dentists who have comparable education and knowledge, who practice in similar disciplines, and those who practice in a comparable area. When a dentist fails to meet the standard of care and the patient is wronged due to negligence, the dentist may be held liable for malpractice.
Most medical and dental malpractice claims arise from an unfavorable interaction with the doctor and not necessarily from an outcome of poor treatment. The statute of limitations for filing a lawsuit varies from state to state. Generally, plaintiffs must file within five years of the last date of service or within three years of the date of discovery. As a point of reference, it takes approximately seven years to settle a claim.
If a dental team member is notified that he or she is involved in a complaint, immediately inform the doctor. Resist any temptation to call or to contact the patient and do not add anything to the patient's record, no matter how important or helpful it is thought to be; an addendum on a separate sheet of paper can be created with the additional information. It cannot be stressed enough - never send out copies of a record to anyone without first notifying the dentist and verifying there is a signed Release of Information form in the record. The dentist must be aware of all duplicates of records that are transferred or sent out, no matter the reason. It is very important not to document, in the clinical record, conversations with attorneys and/or the malpractice insurer. Additionally, do not file in the clinical record any lawsuit correspondence or letters from attorneys and/or the malpractice insurer. Keep this documentation under separate cover in a secure location.
Legal Responsibilities
The legal responsibilities of a dentist to a patient include many areas of patient treatment as seen in Figure 9. The dentist may refuse to treat a patient, however this decision must not be based on the patient's ethnicity, color or faith. Additionally, the Americans with Disabilities Act protects individuals with infectious diseases such as AIDS or a HIV infection. A patient infected with HIV cannot be refused treatment simply because of the disease. The only exception would be if an HIV patient had a unique condition, such as an endodontic infection of a salvageable tooth that required the care of a specialist and the dentist would refer any patient with the same condition to a specialist, regardless of their medical status. Individuals cannot be refused treatment on the sole basis of their medical/disease condition.
Patient abandonment refers to the discontinuation of care after treatment has begun, but before the treatment has been completed. The dentist may be liable for abandonment if the dentist terminated the dentist-patient relationship without giving the patient reasonable notice, usually thirty days. Even if the patient refuses to follow treatment instructions or fails to keep appointments, the dentist is obligated to give the patient another appointment. After notification of termination of the dentist-patient relationship, the dentist is obligated to continue care during those thirty days, until the patient has time to find another provider. The dentist can be accused of abandonment if he/she chooses to go out of town without making arrangements for another dentist to be available for emergencies, or without leaving a forwarding telephone number for the patient to call for care. Patients also have responsibilities to their dentist. The patient is legally required to pay a reasonable and agreed upon fee for services rendered. The patient is also expected to cooperate and follow instructions regarding treatment and home care.
Due care is a legal term referring to appropriate and satisfactory care, or the absence of negligence. The dentist has a legal commitment to use due care in treating all patients and the commitment applies to all treatment procedures. For example, when prescribing an antibiotic for an oral infection, due care implies that the dentist is familiar with the medication, its properties, and side effects. The dentist must also have adequate information about the patient's health to know whether the drug is suitable for the patient.
Prevention of Lawsuits
While patients may bring a lawsuit against the dentist, it does not guarantee that they will win. The following four circumstances, often referred to, as the “Four Ds” all must be present for the malpractice suit to be victorious:
• Duty - a dentist-patient relationship must exist to establish the duty.
• Derelict - negligence occurred as a result of not meeting the standard of care.
• Direct cause - the negligent act was the direct cause of injury.
• Damages - the pain and suffering of the patient, loss of income, medical bills incurred are all included in damages.
Malpractice is professional negligence and in dentistry there are two types of malpractice: acts of omission and acts of commission. An act of omission is the failure to perform an act that a “reasonable and prudent professional” would perform. An example would include the dentist who failed to diagnose a carious lesion because radiographic images were never taken. An act of commission is performance of an act that a “reasonable and prudent professional” would not perform. An example would include the dentist prescribing an antibiotic that the patient is allergic to, without glancing at the medical history or conferring with the patient about allergies to medications. In most malpractice cases, an expert witness is not needed. Under the doctrine of res ipsa loquitur, “the action speaks for itself,” the evidence is quite clear. Examples of this include doing a root canal on the wrong tooth and extracting the wrong tooth.
The major areas of risk management involve three simple concepts:
• Maintaining accurate and complete records
• Gaining informed consent prior to an examination or treatment procedure
• Doing everything possible to maintain the highest standards of clinical excellence
Perhaps the greatest factor in preventing legal issues is maintaining an atmosphere of excellent rapport and open communication with all patients. When patients become frustrated and feel they are not being heard, lawsuits are more likely to occur in order to get the attention of the dentist.
Informed Consent
One of the best ways a dental practice can prevent lawsuits is by obtaining informed consent from patients. The concept of informed consent is based on the idea that it is the patient who must pay the bill and endure the pain and suffering that may result from treatment. Informed consent to the patient is based on the information provided by the dentist about the dental treatment in question. Two things must occur for the patient to give informed consent: the patient must be informed and the patient must give consent. The dentist must give the patient enough information about the oral condition and all available treatment options. Normally, when treatment options are given contraindications or possible undesirable outcomes are also typically given with each option if any exist. The patient and the dentist then openly discuss these options and the patient chooses the most suitable treatment choice.
Informed consent is further broken down into implied and written consent. Implied consent can be described as the case where a dental patient enters the office for an appointment as a new patient, implying consent for at least a dental examination. Likewise, when a dentist recommends a new restoration to replace a deteriorating restoration, the patient is implying consent if he or she does not object to the proposed treatment. Implied consent is a less reliable form of consent in a malpractice suit. The preferred means of gaining consent is through written consent, by obtaining and documenting the patient's consent and understanding of the treatment option.
The patient, at any time, has the right to refuse treatment. If a patient refuses proposed treatment options, it is the duty of the dentist to inform the patient about the likely negative outcomes and obtain the patient's informed refusal. By obtaining the patient's informed refusal, the dentist is still responsible for providing the standard of care. A patient cannot consent to poor quality care and the dentist cannot legally or ethically agree to perform such care. For example, if a patient refuses periodic examinations and radiographic images, the dentist may refer the patient to another provider for treatment because the dentist considers that both periodic examinations and radiographic images are an essential standard of care. Another practitioner, however, may be willing to treat the patient without radiographic images or periodic examinations and may request a written statement signed and dated by the patient documenting this agreement. The statement is then filed with the patient record.
There are some exceptions to disclosure of information when referring to informed consent. The dentist is not under any legal obligation to disclose information about the proposed treatment in the following circumstances:
• The patient requests not to be advised.
• The proposed procedure is straightforward and life-threatening risk is unlikely - for example, death from a sealant.
• The treatment is minor and rarely results in serious side effects - for example, the taking of an impression with alginate material.
• The information would be so upsetting that the patient would be unable to make a rational decision; this is known as therapeutic exception.
Minor patients must have parental, custodial parent or legal guardian consent before any dental treatment is rendered. The dental practice must have on record the name of the custodial parent in the case that the child lives with one parent. In situations of joint custody of child patients, letters of consent, authorization, and billing information on record from both parents are key in the instances where emergency treatment is needed and only one parent is in the practice with the child.
Documenting Informed Consent
In many states there is no specific protocol for the documentation of informed consent. At the very least, the patient's record should show that the patient received information about the benefits, risks, and alternatives of the proposed treatment and whether the patient consented or refused the options. Any time treatment is extensive, invasive, or outcomes uncertain a written consent from the patient is recommended. The patient, dentist, and a witness sign the document then the patient receives a copy and the original is filed in the patient record (see Figure 10).
Informed consent is a process involving in-person discussion between the treating dentist and the patient. Adequate time should be allowed to answer all of the patient's concerns and questions. If the patient is uncertain, treatment should be delayed and the patient should be allowed to go home and think it over. The dentist should then follow up with a courtesy telephone call inquiring if the patient has any additional questions.
Consent forms should contain the following information:
• The nature of the proposed treatment
• Benefits and alternatives
• Risks and potential consequences of not performing treatment
• Other information specific to a particular situation
Whenever a patient's case may be outside the scope of practice for a dentist, a patient referral is done. The dentist must inform the patient that the needed treatment cannot be properly performed in the practice and requires the services of a specialist. The dentist should assist the patient in finding a suitable specialist. Many malpractice claims involve the failure of a dentist to refer a patient to a specialist. This is frequently seen in general dentistry. It is important that the dentist establishes the patient's periodontal baseline as well as existing conditions of the teeth and restorations. When referring a patient to a specialist, the following information must be documented in the patient record:
• Description of the problem
• Reasons for referral
• Name and specialty of the referral dentist
• Whether the patient has consented to the referral or not
Another area of risk management is the documentation of broken appointments or last-minute cancellations. These actions can be interpreted as contributory negligence on the part of the patient. Contributory negligence occurs when the patient's actions, or lack of action, negatively affect the treatment outcome. With proper documentation the practice is protected against legal recourse should the patient decide to claim negligence against anyone on the dental team. An example would include a patient who was told a deep area of decay was found on a radiographic image that was close to the nerve of the tooth and needed immediate treatment before the condition worsened. The patient broke several appointments (contributory negligence) and twelve months later requires extraction of the tooth because it was so badly decayed.
The primary goal of keeping good dental records is to maintain continuity of care. Diligent and complete documentation and charting procedures are essential. Second, because dental records are considered legal documents they help protect the interest of the doctor and/or the patient by establishing the details of the services rendered. In malpractices cases an expert witness usually helps the court decide if a dentist did or did not perform in accordance with the accepted norms, guidelines, and degree of competence that can be reasonably expected from such a professional. Referred to as “standard of care,” this legal duty of a dentist requires exercising the degree of skill and care that would be exhibited by other prudent dentists faced with the same patient-care situation. Dental associations and state dental boards promulgate standards and recommendations that typically determine the standard of care.
The outcomes of dentistry can be unpredictable. With proper documentation, the dental practice will be armed to fight any legal issues directed its way.
Health Insurance Portability and Accountability Act (HIPAA)
The practice administrator must understand the patients' and employees' privacy rights.
The acronym HIPAA stands for the Health Insurance Portability and Accountability Act (HIPAA) of 1996. Definite regulations were included in all areas of health care. HIPAA requires that the transactions of all patient health care information be designed in a standardized electronic style. In addition to protecting the privacy and security of patient information, HIPAA includes legislation on the formation of health savings accounts (HSAs), the authorization of a fraud and abuse control program, the easy transport of health insurance coverage, and the simplification of administrative terms and conditions.
HIPAA covers three key areas and its privacy requirements can be broken down into three types: privacy standards, patients' rights, and administrative requirements.
Privacy Standards
A fundamental concern of HIPAA is the careful use and disclosure of protected health information (PHI). PHI is commonly electronically controlled health information that can be recognized individually, typically through the use of Social Security numbers or other individually designated identifiers. PHI also refers to verbal communication, although the HIPAA Privacy Rule is not intended to obstruct necessary verbal communication. The United States Department of Health and Human Services (USDHHS) does not require restructuring of the dental practice, such as soundproofing, architectural changes, and so forth, but some caution is necessary when exchanging health information via conversation.
An Acknowledgment of Receipt Notice of Privacy Practices, which allows patient information to be used or divulged for treatment, payment, or healthcare operations (TPO), should be obtained from each patient. The patient must sign a statement acknowledging receipt of the practice's written privacy policy and this acknowledgement is kept in the patient's record for a minimum of six years. A detailed and time sensitive authorization can also be issued, which allows the dentist to release information in special circumstances other than TPOs. A written consent is also an option. Dentists can disclose PHI without acknowledgment, consent, or authorization in very special situations such as any of the following:
• Fraud investigation
• Law enforcement with valid permission (i.e., a warrant)
• Suspected child abuse
• Public health supervision
When divulging PHI, a dentist must try to disclose only the minimum necessary information to help safeguard the patient's information as much as possible. It is important that dental professionals adhere to HIPAA standards because health care providers (as well as health care clearinghouses and health care plans) that convey electronically formatted health information via an outside billing service or merchants are considered covered entities. Covered entities may be dealt serious civil and criminal penalties for violation of HIPAA legislation. Failure to comply with HIPAA privacy requirements may result in civil penalties of up to $100 per offense with an annual maximum of $25,000 for repeated failure to comply with the same requirement. Criminal penalties resulting from the illegal mishandling of private health information can range from $50,000 and/or 1 year in prison to $250,000 and/or 10 years in prison.
Patient Rights
HIPAA allows patients, authorized representatives, and parents of minors, as well as minors, to become more aware of the health information privacy to which they are entitled. If any health information is released for any reason other than TPO, the patient is entitled to an accounting of the transaction. Therefore, it is important for dentists to keep accurate records of such information and to provide them when necessary.
The HIPAA Privacy Rule determines that the parents of a minor have access to their child's health information. This privilege may be overruled, for example, in cases where there is suspected child abuse or the parent consents to a term of confidentiality between the dentist and the minor. The parents' rights to access their child's PHI also may be restricted in situations when a legal entity, such as a court, intervenes and when a law does not require a parent's consent. For a full list of patient rights provided by HIPAA, be sure to acquire a copy of the law and to understand it well (see Figure 11).
Administrative Requirements
Complying with HIPAA legislation may seem like a chore, but it does not need to be so. It is recommended that the practice administrator become appropriately familiar with the law, organize the requirements into simpler tasks, begin compliance early, and document progress in compliance. An important first step is to evaluate the current information and practices of the dental office. Dentists will need to write a privacy policy for their office; a document for their patients detailing the office's practices concerning PHI. It is useful to try to understand the role of health care information for patients and the ways in which they deal with the information while they are visiting the practice. Staff training is a must, thereby ensuring that all staff members are familiar with the terms of HIPAA and the practice's privacy policy and related forms. HIPAA requires that a privacy officer be designated. A privacy officer is a person in the practice who is responsible for applying the new policies in the practice, fielding complaints, and making choices involving the minimum necessary requirements. Another employee, with the role of contact person, will process complaints.
A Notice of Privacy Practices, a document detailing the patient's rights and the dental practice's obligations concerning PHI, also must be drawn up. Further, any role of a third party with access to PHI must be clearly documented. This third party is known as a business associate (BA) and is defined as any entity that, on behalf of the dentist, takes part in any activity that involves exposure of PHI (Figure 12).
The following are not considered to be Business Associates: a member of the staff such as an employed dental associate, assistant, receptionist or hygienist; the U.S. Postal Service; or a janitorial service.
HIPAA Security
The Security Rule defines highly detailed standards for the integrity, accessibility, and confidentiality of electronic protected health information (EPHI) and addresses both external and internal security issues.
Entities covered by HIPAA are required to:
• Assess potential risks and vulnerabilities.
• Protect against threats to information security or integrity, and guard against unauthorized use or disclosure of information.
• Implement and maintain security measures that are appropriate to their needs, capabilities, and conditions.
• Ensure entire staff compliance with these safeguards.
The standard is broken into three separate parts:
Administrative Safeguards- This segment, which makes up half of the complete standard, limits information access to proper individuals and shields information from all others. It must include documented policies and procedures for daily operations, address the conduct and access of workforce members to EPHI, and describe the selection, development, and use of security controls in the workplace.
Physical Safeguards- Physical safeguards prevent unauthorized individuals from gaining access to EPHI via computerized systems and the Internet.
Technical Safeguards- This section includes using technology to protect and control access to EPHI.
Summary
The practice administrator must act as a professional liaison between the dental team members and between the dental team and the patients they serve. The person employed in the position of practice administrator must be capable to effectively communicate the policies of the practice to all parties as necessary and understand the importance of the many forms of dental documentation and HIPAA protection laws. Several daily tasks occurring within the dental office and managed by the practice administrator keep the practice running smoothly and production at an optimum level. The employment responsibilities such as interviewing, hiring, training, and termination are best handled by a knowledgeable practice administrator. Additional responsibilities such as public relations, delegation of duties, and conflict resolution are situations that any practice administrator may encounter and be expected to handle with educated efficiency.
Glossary
credibility - barrier to understanding communication if the person is believed to be unqualified
FICA - Federal Insurance Contributions Act; also known as the Social Security tax
Form I-9 - government form that verifies the eligibility, citizenship, and identity of the employee
grievance - a complaint filed by an employee when they feel wronged by another person
hidden agenda - barrier to understanding communication if the sender and receiver of information are using it to fulfill their personal ambition
HIPAA - abbreviation for Health Insurance Portability and Accountability Act of 1996
jargon - barrier to communication if professional, technical terms are used to explain or convey information to the nonprofessional
noise - barrier to communication and understanding when there is distracting or loud noises in the workplace, such as a handpiece, the office compressor, or printer
PHI- abbreviation for Protected Health Information
practice administrator - one who manages the staff of a practice; also referred to in this course as Office Manager
semantics - barrier to understanding when a word or term conveys a different meaning to the receiver (example: handpiece vs. drill)
stereotyping - barrier to communication when someone is wrongly judged by appearance
termination - to end employment
References
Andujo, Emily. Dental Assistant: Program Review and Exam Preparation (PREP). Stamford, CT: Appleton and Lange, 1997.
Bird, Doni, and Robinson, Debbie. Torres and Ehrlich Modern Dental Assisting. 10th ed., St. Louis: Elsevier Saunders, 2012.
Finkbeiner, Betty Ladley, and Johnson, Claudia Sullens. Mosby's Comprehensive Dental Assisting: A Clinical Approach. St. Louis: Mosby, 1995.
Finkbeiner, Betty L. and Finkbeiner, C.A. Practice Management for the Dental Team. 7th ed., St. Louis, Elsevier Inc., 2011.
Finkbeiner, Betty L. “Basic Concepts of Dental Practice Management.” American Dental Assistants Association, 2006.
Gaylord, Linda J. The Administrative Dental Assistant, 3rd ed., St. Louis, Elsevier Saunders, 2011.
Palmer, Craig. New form required for new hires. ADA News: March 14, 2013. http://www.ada.org/news/8364.aspx. Accessed August 15, 2013.
Phinney, Donna J., and Haldstead, Judy H. Delmar's Dental Assisting: A Comprehensive Approach. 2nd ed.; Clifton Park, New York. Delmar, 2004.
About the Authors
Natalie Kaweckyj, LDARF, CDA, CDPMA, COMSA, CPFDA, MADAA, BA
Natalie Kaweckyj currently resides in Minneapolis, MN, where she is the Clinic Coordinator and Compliance Analyst for a nonprofit pediatric dental clinic. She is a Licensed Dental Assistant in Restorative Functions (LDARF), Certified Dental Assistant (CDA), Certified Dental Practice Management Administrator (CDPMA), Certified Orthodontic Assistant (COA), Certified Oral & Maxillofacial Surgery Assistant (COMSA), Certified Preventive Functions Dental Assistant (CPFDA), and a Master of the American Dental Assistants Association. She holds several expanded function certificates, including the administration of nitrous oxide/oxygen analgesia. Ms. Kaweckyj graduated from the American Dental Association-accredited dental assisting program at ConCorde Career Institute and has received a Bachelor of Arts in Biology and Psychology from Metropolitan State University. She is currently writing her dissertation for her master's in Public Health. She has worked clinically, administratively and academically. Ms. Kaweckyj is currently serving as on several ADAA Councils after having served on the ADAA Board of Trustees 2002 - 2012. She served as ADAA President in 2010-2011. She is the current Business Secretary and legislative chairman for the Minnesota Dental Assistants Association (MnDAA) and a three-time past president of MnDAA. She also is a Past President of the Minnesota Educators of Dental Assistants (MEDA) and still an active member. In addition to her association duties, Natalie is very involved with the Minnesota state board of dentistry as well as with state legislature in the expansion of the dental assisting profession. She is a freelance writer and lecturer and is always working on some project. She has authored many other courses for the ADAA.
Acknowledgement of Contributing Authors
Wendy Frye, CDA, RDA, MADAA
Wendy Frye, CDA, RDA, MADAA, currently lives in St Louis, Missouri where she is a chairside dental assistant and implant treatment coordinator in a periodontal office. She is a Certified Dental Assistant, Registered Dental Assistant, and a Master of the American Dental Assistants Association. Wendy graduated from the ADA accredited dental assisting program at Kirkwood Community College in Cedar Rapids, Iowa.
Wendy has served in many various capacities on the local and state levels of the Iowa and California Dental Assisting Associations. She has served on various committees of the American Dental Assistants Association and as delegate to the ADAA House of Delegates.
Lynda Hilling, CDA, MADAA
Lynda Hilling, CDA, MADAA, lives in Billings, Montano. She is a Certified Dental Assistant and has been employed in the private practice of Michael W. Stuart, DDS for the last ten years as a chairside assistant. Lynda began her dental assisting career as an on the job trained assistant and then challenged the CDA exam in 1999. Lynda is a Master in the American Dental Assistants Association and has served on the Executive Board of the Montana Dental Assistants Association, including the Presidency.
Lisa Lovering, CDA, CDPMA, MADAA
Lisa Lovering, CDA, CDPMA, MADAA, is a Certified Dental Assistant and a Certified Dental Practice Administrator employed chairside in the private practice of Michael W. Stuart, DDS. Lisa began her dental assisting career as an on the job trained assistant, and then challenged the CDA and CDPMA exams. She is a former Tenth District Trustee for the ADAA.
As a member of the American Dental Assistants Association, Lisa has received her Mastership. Lisa has served on the Montana Dental Assistants Dental Assistants Association Executive Board including the Presidency.
Linette Schmitt, CDA, RDA, MADAA
Linette Schmitt, CDA, RDA, MADAA, is a graduate from the ADA accredited dental assisting program at Hibbing Community College. Linette currently works as a chairside assistant in a large group practice. She is a MN Registered Dental Assistant and a Certified Dental Assistant, and is also certified to administer nitrous oxide analgesia. She is a member of the American Dental Assistants Association and holds an ADAA Mastership.
She has served in many capacities at the local and state levels of her association level, and as the ADAA Seventh District Trustee. Linette is legislatively involved with the MN Board of Dentistry's Policy Committee.