You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Despite declines in cigarette smoking among adolescents and adults in the United States (US), the use of electronic cigarettes (e-cigarettes) is increasing rapidly.1, 2 The percentage of adults who have ever used e-cigarettes rose from 3.3% in 2010 to 8.5% in 2013.3 Current e-cigarette use (defined as use in the past 30 days) among high school students increased from 1.5% in 2011 to 16% in 2015.1
E-cigarettes are battery-operated devices that work by heating and converting a liquid mixture, often called e-liquid, into an aerosol, commonly termed vapor, and delivering nicotine to the user without the combustion of tobacco.4 E-cigarettes contain nitrosamines (potent cancer-causing chemicals), diethylene glycol, and other contaminants potentially harmful to humans.5 The adverse health effects of e-cigarette use are currently under study.
As a possible alternative product for conventional cigarettes, it has been suggested that e-cigarettes have the potential to reduce harm.6 However, it also has been proposed that e-cigarettes could act as a gateway product to cigarette smoking and encourage dual use with other forms of tobacco and/or marijuana.7 Moreover, e-cigarettes are heavily marketed and portrayed as a safe alternative to tobacco.8 Mixed messages and lack of consensus may lead college students to rely on their own risk and benefit perceptions of e-cigarettes in their decision making about whether or not to use. Dental hygienists, like other healthcare professionals, play an important role in preventing initiation and encouraging cessation of tobacco use among their patients.9-11 The current Clinical Guideline for the Treatment of Tobacco Use and Dependence recommends that the 5A’s, consisting of the following:
Asking about tobacco use at each appointment, advising users to quit, assessing readiness to quit, providing assistance with the quitting process, and arranging follow up, be implemented at each patient visit.12 Studies have documented that a physician’s brief advice to quit smoking significantly increased long-term smoking abstinence rates by about 10%.12
Moreover, brief tobacco interventions by non-physician clinicians can result in estimated long-term abstinence rates of 16%.13 A 1996 telephone survey of first-year college students, however, revealed that only 26% of those who reported a medical visit within the past 12 months (89% of the total sample) had received any information from their physician about traditional tobacco products.14 Because e-cigarettes are a relatively new product, they are not explicitly mentioned in the Clinical Guideline for Treatment of Tobacco Use and Dependence.12 It is unknown whether or not healthcare professionals, including dental hygienists, address e-cigarettes in their delivery of tobacco related counseling to their patients.
Although e-cigarette use has been documented among college students generally, little is known about factors associated with use or exposure to health professional counseling about use among college students.15 Therefore, the purpose of this study was to assess e-cigarette use; factors associated with use (e.g., perceptions of risks and benefits); and exposure to e-cigarette-related information from health professionals, in a sample of college students attending a public university in the San Francisco bay area using a web-based survey.
Methods
This quantitative cross-sectional study surveyed a sample of English-speaking students aged 18 years or older at a public university in the San Francisco Bay Area. The study was implemented using the online survey software program, QualtricsTM (Qualtrics, Provo, UT). The Institutional Review Board of the University of California, San Francisco approved the study.
Recruitment and Informed Consent: The researcher contacted two faculty members teaching a total of three courses at the university to explain the study and to solicit help recruiting study participants. They agreed to distribute the recruitment letter explaining the study and to provide an electronic link to the survey and an attached consent form. A follow-up email message was sent to all students two weeks later as a reminder to complete the survey.
Measurements: The 18-item survey, developed in part by study investigators, consisted of 1 e-cigarette related awareness item (yes/no response option); 7 e-cigarette use status items (measured on frequency sliding scales); 2 harmfulness items related to use of e-cigarettes, other tobacco products, and marijuana (measured on a 5-point Likert-scale ranging from “not at all harmful”, to “extremely harmful” or “don’t know”); 1 addiction item related to use of e-cigarettes, other tobacco products, and marijuana (measured on a 5-point Likert-scale ranging from “extremely unlikely I would become addicted” to “extremely likely I would become addicted” or “don’t know”); 1 healthcare counseling item assessing which of 5 healthcare professionals (physicians, dentists, dental hygienists, psychologist, student health physician) had provided counseling for each of 6 investigated products (cigarettes, smokeless tobacco, e-cigarettes, hookah, cigars, marijuana); 1 social acceptability item (level of agreement with the statement: “My friends think it’s ok (socially acceptable) for me to use [specific product]” measured on a 5 point Likert-scale ranging from “strongly disagree” to “strongly agree” or “don’t know”); 1 previously developed conditional risk assessment of e-cigarette use item16, 17 (measured on a frequency sliding scale) where participants were asked to estimate the chance (perceived probability) from 0-100% that 15 specific health or social outcomes would happen to them given the hypothetical scenario: “Imagine that you just began using e-cigarettes. You use e-cigarettes 2-3 times/day, some-times… alone and sometimes…with friends;”16, 17 and 4 demographic items (age, ethnicity, gender, year in college).
Pre-testing: The survey was pretested for feasibility and acceptability by a convenience sample of 10 college students, aged 18-24 years old who did not take part in the final survey. The pre-test sample was debriefed after survey administration to address their understanding of questionnaire items and questions were revised based on their feedback.
Data analysis: Responses to the survey items were tabulated for each respondent using Microsoft Excel (2010) and the mean response frequency for each item was calculated. Perceived harmfulness, perceived environmental harm to others, and perceived social acceptance, respectively, were cross-tabulated by various tobacco products and marijuana. SPSS software (Version 22.0; IBM Corporation, Armonk, NY, USA) was used to analyze the perceived chance (from 0-100%) of developing physical and social risks and benefits associated with daily use of e-cigarettes among ever-users and never-users. The Mann-Whitney U-test was utilized with a level of significance set at ≤0.05. Respondents who did not complete the item related to risks and benefits of e-cigarettes use were removed from this particular analysis.
Results
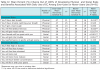
Of 300 online surveys distributed, 91 were completed (response percentage: 30%). The majority of the participants were 18-21 years of age, female, Caucasian or Asian, and in their second or third year of college (Table I).
Nearly all respondents were aware of e-cigarettes; almost half were ever-users (defined as having used at least once in their life) and 10% were current users (defined as having used in the past-30 days). All e-cigarette never-users reported it was unlikely that they would try e-cigarettes in the next 6 months.
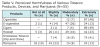
The remaining 6% did not answer the question. Ever-users’ most frequently stated reasons for using e-cigarettes were, “I enjoy sampling different e-juice flavors with friends” and “I enjoy watching the exhaled vapor” (Table II). Of the ever-users who responded, almost half reported using hookah pens. Most ever-users either used 0-6mg/ml of nicotine in their e-liquid, or did not know the concentration of nicotine used. The most common e-liquid flavors preferred by ever-users were fruit, mint/wintergreen, and candy (Table III).
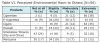
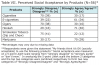
When given a hypothetical scenario of using e-cigarettes routinely, never users perceived a statistically significantly higher chance of experiencing 5 out of 8 physical and social risks from e-cigarette use than ever-users (P≤0.05) (Table IV). Although never-users perceived a lower chance of experiencing physical and social benefits from e-cigarette use than ever-users, this difference was not statistically significant (Table IV).
Most of the respondents perceived cigarettes, cigars and smokeless tobacco (dip and chewing tobacco) as “extremely harmful.” Whereas 60% perceived marijuana to be “not at all harmful” or “slightly harmful,” and 47% perceived e-cigarettes as “moderately harmful” (Table V).
Sixteen percent of respondents thought that e-cigarettes caused extreme environmental harm to those around someone using e-cigarettes (Table VI). In general, e-cigarettes, hookah, and marijuana were perceived as causing less environmental harm to others than cigarettes and cigars (Table VII).
Over half of the respondents perceived e-cigarettes, hookah, and marijuana as being socially acceptable, whereas cigarettes, cigars, and smokeless tobacco were perceived as less socially acceptable products (Table VII).
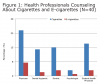
Students were more likely to report receiving counseling about the adverse health effects of cigarettes from physicians than from dental professionals. Few respondents reported receiving counseling regarding e-cigarettes from any health professional (Figure 1).
Discussion
Consistent with the 2011 findings of Trumbo and Harper, the majority of the college student participants in this study had heard of e-cigarettes.15 Moreover, one-tenth of the respondents were current e-cigarette users, and 49% of the survey population had used e-cigarettes at least once. In contrast though, Trumbo and Harper found that only 13% of college students in their study had ever used e-cigarettes.15 This discrepancy may be explained by the study’s small convenience sample size, as well as by the fact that the Trumbo and Harper study was conducted in 2011 three years prior to this study. Studies report that e-cigarette use has been increasing over time.1,3 The increase has been particularly rapid among high school adolescents, for whom e-cigarette use has been reported at 16% in 2015.1
In 2014, e-cigarette advertising was the most widely circulated of all marketing for non-combustible tobacco products.18 E-cigarettes entered the US market in 2007, and the affordability, availability, and marketing of these products has increased over recent years.19 A 2014 study indicated that young adult cigarette smokers were receptive to television ads and reported intentions to use e-cigarettes after viewing an advertisement that was televised on numerous US cable networks.20 Advertising of tobacco products such as e-cigarettes have been shown to influence consumer awareness, experimentation, and current use among young people.21
Among the ever-users of e-cigarettes in this study, less than half did not know the concentration of nicotine in the e-liquid that they used. Most users preferred an e-liquid flavored with fruit, mint/wintergreen, and candy as the most preferred flavors, illustrating that e-cigarette flavors are appealing to young adults. Farsalinos et al. reported that most of their adult respondents commonly used a fruit flavored e-liquid.22
Most e-cigarette ever-users in this study used pen-type devices. In contrast, other studies have shown that ever-users are more likely to use first generation devices, which look similar to a cigarette and are classified as “ciga-likes.” Established users (used e-cigarettes more than 50 times in their lifetime) are reported to be more interested in the advanced generation devices, classified as “tanks,” that have a large, high-powered battery and often a button to press before inhalation.23, 24
Major reasons for e-cigarette use in this study included “I enjoy sampling different e-juice flavors with friends” and “I enjoy watching the exhaled vapor.” These findings are consistent with those of Etter who reported that young adult and adult respondents used e-cigarettes because they liked the taste and the variety of flavors offered.25 In contrast, Peters et al found that almost half of their college students who ever used e-cigarettes endorsed quitting or reducing smoking as their reasons for use.26 In the Peters et al study, 32% also endorsed reasons for use related to curiosity/experimentation.26
In this study, e-cigarettes were perceived to be the most socially acceptable of all products included in this survey, followed by marijuana and hookah, whereas cigarettes and cigars were perceived as not socially acceptable. Berg et al reported similar findings among college students, suggesting that the new culture of hookah and e-cigarette lounges attracting young adults, supports the perception that hookah and e-cigarettes are being increasingly viewed as socially acceptable.27 This social acceptance may have been initally due to the lack of regulation of these products at the federal and state level. In 2013, the Food and Drug Administration (FDA) issued a deeming rule, which has was finalized in 2016, giving the FDA authority to regulate the marketing, sale, and manufacturing of e-cigarettes, cigars, pipe tobacco, and hookah tobacco.28 Previously, such restrictions were left to state and local governments. In California, where this sample was drawn, the sale of e-cigarettes to minors under 18 years of age has been banned since 2011.29 Local ordinances enacted in the community in which this study was conducted have amended clean indoor air laws to prohibit e-cigarette use in public areas, such as restaurants and bars. Local regulatory action may also influence the perceived social acceptability of e-cigarettes, and therefore, the level of social acceptance measured in this study might differ from what would be measured in communities under different regulatory approaches.
The college students in this study who had never used e-cigarettes perceived a significantly higher percent chance of developing bad breath, feeling jittery and nervous, getting mouth sores, upsetting friends, and getting into trouble if they used e-cigarettes than college students who had ever used e-cigarettes. These findings are consistent with those of Halpern-Felsher and colleagues who reported that adolescent non-smokers estimated their chance of experiencing a smoking-related negative outcome as more likely than smokers.16 Chaffee and colleagues also reported in a sample of adolescents that risk composite scores were inversely associated with e-cigarette ever-use and use intention.17 These findings can be explained by the Health Belief Model which posits that when the perceived risks of performing a behavior outweigh the perceived benefits, an individual tends not to adopt the behavior.30
Respondents in this study perceived e-cigarettes, marijuana, and hookah use to be less harmful to their health and to cause less harm to others than the use of cigarettes. These findings are similar to those reported in a study of 2,002 students from two southeastern universities in the US that found students perceived marijuana, e-cigarettes, and hookah use to be less harmful to their health than use of cigarettes, cigar products, and smokeless tobacco.27 In that study, the majority of college students also believed that e-cigarettes had fewer health risks than traditional cigarettes. This perception is of concern, because if e-cigarette use is viewed as having few health consequences, there may be relatively little hesitation among young people to try the product. While e-cigarette aerosol may contain fewer toxicants than cigarette smoke, scientific evidence has not yet been accumulated to evaluate the short-term and long-term health effects of e-cigarette use.31 Dental hygienists need to inform their clients of this lack of evidence, to stay abreast of e-cigarette related research as it becomes available, and to incorporate such information into their client tobacco-related counseling.
In this study, college students reported receiving little or no counseling related to e-cigarette use from health professionals, including dental hygienists, although about a quarter of respondents reported receiving counseling regarding the adverse health effects associated with cigarette use. These findings suggest a need for dental hygienists and other healthcare professionals to increase their awareness of e-cigarettes and their comfort level in discussing e-cigarettes and other tobacco products with their college-age clients. These findings are consistent with several studies evaluating self-reported tobacco education and cessation interventions by dental profes-sionals. Such studies have reported that dental professionals, including dental hygienists, do not regularly ask about patients’ tobacco use or implement the 5 A’s,32-34 although evidence suggests that counseling from dental professionals can effectively reduce tobacco use when implemented.12 These findings are also consistent with those of Foote et al who found that only 26% of college students in their study reported receiving tobacco related counseling by physicians at their medical visit in the last year.14 In contrast, Sutfin et al found that 62% of North Carolina college students reported being screened for tobacco use at their student health center; and 50% of those students reported being advised to quit or reduce tobacco use.35
Although there have been multiple comprehensive reports about the adverse health effects of cigarettes, to date there have been no such reports on e-cigarettes as this evidence is being collected currently.21,36-38
A 2013 study of Minnesota health care providers’ awareness of e-cigarettes reported that although nearly all had heard of e-cigarettes, they knew little to nothing about e-cigarettes, and more than half were either somewhat or very uncomfortable talking to patients about e-cigarettes.39 The findings in this study highlight the need to encourage dental hygienists and other healthcare professionals to screen every patient routinely for use of e-cigarettes, as well as use of other tobacco products and to provide a brief intervention for users.
This study has several limitations. The sample is a small, convenience sample of college students enrolled in humanities and science courses at a university in northern California. At the state level, California has strict cigarette and smokeless tobacco regulations, and local ordinances have extended clean indoor air laws to include e-cigarettes. These regulations may influence e-cigarette perceptions and limit the ability to generalize findings to all United States college students. The low response percentage increases the possibility of selection bias in that those who responded may have been more interested in e-cigarettes than those who did not respond. In addition, the data analysis focused on ever-users and never-users of e-cigarettes. Due to the small number of current-users in this sample (n=9), this group was not analyzed separately. Further research is needed to examine how patterns of current use, including total nicotine exposure, are related to attitudes and risk perceptions among e-cigarette users. In addition, some questionnaire items were developed specifically for this study and further validity and reliability testing is warranted.
Finally, this study focused only on e-cigarette use and did not assess use behaviors of other tobacco products. Consequently, our groups of ever-users, current-users and never-users may have been users of other tobacco products which may have confounded our results. Nevertheless, this study provides insights into the use of e-cigarettes among college students and factors associated with use to inform future studies.
Conclusion
The use of e-cigarettes is increasing in the US, especially among adolescents and young adults. Our findings demonstrate a high prevalence of e-cigarette use and experimentation among college students in our sample population. Participants’ perceptions related to reduced harm of e-cigarettes may influence their willingness to use such products. Dental hygienists need to stay current with the scientific evidence related to e-cigarette use and incorporate this information into their tobacco-related education and cessation counseling. Such information will help their patients develop accurate perceptions about physical and social risks associated with e-cigarette use so that they can make informed decisions to protect their current and future health.
Shiva Abadi, RDH, MS, is a graduate of the Master of Science in Dental Hygiene Program at the University of California, San Francisco.
Elizabeth T. Couch RDH, MS, is an Assistant Professor, Benjamin W. Chaffee, DDS, MPH, PhD, is an Assistant Professor Margaret M. Walsh, RDH, MA, MS, EdD, Professor Emerita, all in the Department of Preventive and Restorative Dental Sciences at the University of California, San Francisco.
Acknowledgments
The authors would like to thank the students and faculty who gave their time to this research. The authors also acknowledge the passing of their colleague, mentor, and friend, Dr. Margaret Walsh, a renowned scholar in the areas of dental hygiene, oral disease prevention, and tobacco cessation. Her remarkable legacy will continue to inspire and impact the dental hygiene profession as a whole, especially those in the field of tobacco control.
References
1. Singh T, Arrazola RA, Corey CG, et al. Tobacco Use Among Middle and High School Students — United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65:361–367.
2. Agaku IT, King BA, Husten CG, et al. Tobacco product use among adults - United States, 2012-2013. MMWR Morb Mortal Wkly Rep. 2014 Jun 27;63(25):542-7.
3. King BA, Patel R, Nguyen KH, Dube SR. Trends in awareness and use of electronic cigarettes among US adults, 2010-2013. Nicotine Tob Res. 2015 Feb;17(2):219-27.
4. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014 May 13;129(19):1972-86.
5. Westenberger B. Evaluation of e-cigarettes. St Louis, MO: Food and Drug Administration. 2009:1-8.
6. Cahn Z, Siegel M. Electronic cigarettes as a harm reduction strategy for tobacco control: A step forward or a repeat of past mistakes? J Public Health Policy.2011 Feb;32(1):16-31.
7. Riker CA, Lee K, Darville A, Hahn EJ. E-cigarettes: Promise or peril? Nurs Clin North Am. 2012 Mar;47(1):159-71.
8. Grana RA, Ling PM. “Smoking revolution”: A content analysis of electronic cigarette retail websites. Am J Prev Med. 2014 Apr;46(4):395-403.
9. American Medical Association. AMA strengthens policy on electronic cigarettes to protect youth [Internet]. [cited 2015 Jun 30].Available from http://ama-assn.org
10. American Dental Association. Evidence-based dentistry: systematic reviews.[Internet]. [cited 2015 Jun 30]. Available from: http://ebd.ada.org/en/evidence/evidence-by-topic/tobaccouse-and-smoking-cessation.
11. American Dental Hygienists’ Association. ADHA association policy manual [Internet]. [cited 2014 June 23]. Available from: https://www.adha.org/resources-docs/7614_Policy_Manual.pdf.
12. Fiore MC, Jaén CR, Baker TB, et al. Treating tobacco use and dependence: 2008 update. clinical practice guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008.
13. Fiore MC. US public health service clinical practice guideline: Treating tobacco use and dependence. Respir Care. 2000 Oct;45(10):1200-62.
14. Foote JA, Harris RB, Gilles ME, et al. Physician advice and tobacco use: A survey of 1st year college students. J Am Coll Health.1996 Nov;45(3):129-32.
15. Trumbo CW, Harper R. Use and perception of electronic cigarettes among college students. J Am Coll Health. 2013;61(3):149-55.
16. Halpern-Felsher BL, Biehl M, Kropp RY, Rubinstein ML. Perceived risks and benefits of smoking: Differences among adolescents with different smoking experiences and intentions. Prev Med. 2004 Sep;39(3):559-67.
17. Chaffee BW, Gansky SA, Halpern-Felsher B, Couch ET, Essex G, Walsh MM. Conditional risk assessment of adolescents’ electronic cigarette perceptions. Am J Health Behav. 2015 May;39(3):421-32.
18. Richardson A, Ganz O, Stalgaitis C, Abrams D, Vallone D. Non-combustible tobacco product advertising: How companies are selling the new face of tobacco. Nicotine Tob Res. 2014 May;16(5):606-14.
19. Chen IL. FDA summary of adverse events on electronic cigarettes. Nicotine Tob Res. 2013 Feb;15(2):615-6.
20. Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014 Jul;134(1):e29-36.21. US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Washington, DC.,US GPO.2012.
22. Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Spyrou A, Voudris V. Impact of flavour variability on electronic cigarette use experience: An internet survey. Int J Environ Res Public Health. 2013 Dec17;10(12):7272-82.
23. Giovenco DP, Lewis MJ, Delnevo CD. Factors associated with e-cigarette use: A national population survey of current and former smokers. Am J Prev Med. 2014 Oct;47(4):476-80.
24. Yingst JM, Veldheer S, Hrabovsky S, Nichols TT, Wilson SJ, Foulds J. Factors associated with electronic cigarette users’ device preferences and transition from first generation to advanced generation devices. Nicotine Tob Res. 2015 Oct;17(10):1242-6.
25. Etter JF. Electronic cigarettes: a survey of users. BMC Public Health. 2010 May 4;10:231,2458-10-231. 26. Peters EN, Harrell PT, Hendricks PS, et al. Electronic cigarettes in adults in outpatient substance use treatment: awareness, perceptions, use, and reasons for use. Am J Addict. 2015 Apr;24(3):233-9.
27. Berg CJ, Stratton E, Schauer GL, et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Subst Use Misuse. 2015 Jan;50(1):79-89.
28. Food and Drug Administration (US). Products, guidance and regulations: deeming extending authorities to additional tobacco products. Final rules. Fed Regist. 2016 May; 81FR: 28973-29106.
29. CA Health and Safety Code. Division104. Environmental Health; HSC:119405.[Internet] California Legislative Information;2015 [cited 2015 Dec 22]. Available from http://www.leginfo.ca.gov.
30. Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988 Summer;15(2):175-83.
31. Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014 Mar;23(2):133-9.
32. Warnakulasuriya S. Effectiveness of tobacco counseling in the dental office. J Dent Educ. 2002 Sep;66(9):1079-87.
33. Tomar SL. Dentistry’s role in tobacco control. J Am Dent Assoc. 2001 Nov;132:30S-5S.
34. Studts JL, Burris JL, Kearns DK, et al. Evidence–based tobacco cessation treatment by dental hygienists. J Dent Hyg. 2011 Winter;85(1):13-21.
35. Sutfin EL, McNamara RS, Blocker JN, et al. Screening and brief intervention for tobacco use by student health providers on college campuses. J Am Coll Health. 2012;60(1):66-73.
36. US Department of Health and Human. Preventing tobacco use among young people: A report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 1994;338p.
37. US Department of Health and Human Services. The health consequences of smoking: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2004.
38. US Department of Health and Human Services. The health consequences of smoking—50 years of progress: a report of the surgeon general. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health. 2014.
39. Alberg AJ, Shopland DR, Cummings KM. The 2014 surgeon general’s report: commemorating the 50th anniversary of the 1964 report of the advisory committee to the US surgeon general and updating the evidence on the health consequences of cigarette e smoking. Am J Epidemiol. 2014 Feb 15;179(4):403-12.