You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The composition of the smile architecture includes pink and white (ie, gingiva and tooth structure, respectively), which complement each other and must be in balance and harmony in terms of color, texture, shape, polish, and stippling or microtexture. Therefore, the health and appearance of gingival tissues significantly affect smile esthetics. Unfortunately, many patients present with gingival recession, which is characterized by root surface exposure at the gingival margin. Because gingival recession causes unsightly smile esthetics, an increasing number of patients are seeking dentists to address their “absence of pink” through treatment that is cost effective and more convenient than invasive options such as surgical grafting procedures.1
Traditionally, treatments for gingival recession and resulting lesions have included specific restorative procedures, depending on causative factors.2,3 Other approaches have included laser therapy, tissue grafting, flap designs, orthodontics (eg, clear aligners), and guided tissue restoration, each of which is costly, time-consuming, and can potentially require a long, painful recovery for patients.4
Class V cervical lesions, a consequence of gingival recession and a factor contributing to smile disharmony, occur due to stress distribution. Vertical loading stresses in the crown of the tooth are transferred into horizontal stresses, then retransferred into the Class V area, where stress accumulates and proceeds vertically down the long axis of the root, creating problematic restorative areas in terms of biomechanical design.5,6
Fortunately, solutions for restoring Class V lesions have been developed that do not adversely affect gingival health, produce less inflammatory response, and ultimately contribute to better outcomes than leaving the roots exposed, particularly when the restorations are contoured, finished, and polished well.7 More recently, manufacturers have been developing “smart materials” that neutralize acid to establish a neutral pH, inhibit plaque formation, and decrease the risk of secondary decay. This emerging frontier of bioactive materials also seeks to harness the benefits of fluoride release, decrease demineralization, and decrease microleakage.8
However, using tooth-colored direct composites (eg, typical VITA shades) when treating gingival recession or Class V areas may leave the teeth appearing very long, contributing to an unesthetic smile.9 Therefore, it is important to remember that restoring challenging cases in the anterior requires a more comprehensive approach and a deeper understanding of the pink components of the smile, because the gingival architecture represents the frame of the tooth and the smile and is the hallmark of both pink and white esthetics.10
Achieving Dimensions of Pink Esthetic Dentistry
Pink esthetic dentistry is the application of comprehensive knowledge of facial esthetics and restorative techniques, combined with detailed patient and interdisciplinary communication, to regenerate the supporting periodontal structures that have been lost due to periodontal disease and/or gingival recession, which can result in dark margins on a tooth crown, exposed roots, black triangles between teeth, and other esthetic deficiencies.10,11 Whether created with porcelain, denture bis-acryl, or direct composite, these gingival prosthetic restorations are pink, not white, thereby introducing a fourth dimension of color to the restorative process.
For example, traditional color analysis of teeth is completed on three levels (ie, incisal, middle, and cervical) using VITA shade guides. When restoring pink esthetics, the fourth dimension of color encompasses the gingival architecture, or pink (Figure 1).12,13 According to Coachman, astute clinicians and technicians pay the same level of attention to detail to shade variations and texture when designing gingival prosthetics as they do when replicating tooth anatomy.10,12,13 Therefore, because the gingival architecture represents the frame of the teeth, if not restored correctly—either surgically or prosthetically—the 3-dimesional outcome of the entire smile design will be impaired, from both micro- and macro-esthetic perspectives.
For this reason, as an ethnically diverse population continues to age and clinicians increasingly encounter patients with gingival recession, customizing shades for gingival prosthetic restorations will be of paramount importance for achieving esthetic outcomes. Clinicians and laboratory technicians have long interpreted pink esthetic shades in denture prostheses and implant-supported prosthetics using bis-acryl and ceramics, respectively.10,12,13 The use of direct composite restorative materials has also been cited in the literature, at least as far back as 1997,14 where it was noted that the cervical contour must be created in such a way as to prevent plaque retention. Interestingly, Coachman asserts that when fabricating artificial gingiva using both pink and white, composite resin is better than using pink porcelain alone because the material is more biocompatible subgingivally, is easier to repair for continual maintenance, and provides excellent esthetics.10,12,13
Requisites for Direct Pink Esthetic Restoratives
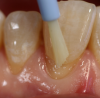
As dentistry continues to embrace minimal intervention restorative approaches, materials that are truly restorative and therapeutic, versus inert, will be required. Direct composites have recently been introduced that are bioresponsive and demonstrate bioactivity in terms of fluoride release, inhibiting marginal demineralization after acid exposure, and decreasing the biofilm that accumulates subgingivally and contributes to plaque.15-17 Such characteristics are essential when creating artificial gingiva and restoring pink esthetics for patients who present with gingival recession (Figure 2), because biofilm and plaque development could result in inflammation of the surrounding natural tissues, caries, and future esthetic compromises.
One available direct composite (Beautifil® II, Shofu Dental, www.shofu.com) that demonstrates these necessary characteristics contains surface pre-reacted glass fillers (S-PRG), a technology known as Giomer. When used to treat gingival recession and Class V lesions, the benefits of this Giomer technology-based composite include an antiplaque effect, remineralization of dentin, discharge and recharge of fluoride ions, and moisture protection for long-term durability.15-17
To best achieve an illusion of gingival tissues (ie, an admittedly imperfect simulation that is acceptable at a distance of 3 feet or more), it is imperative that the selected gingiva replacement composite demonstrate light-diffusing properties and a chameleon effect with surrounding natural tissues. The highly filled composition of the aforementioned Giomer-based composite contributes to light refraction and, therefore, optical properties similar to those exhibited by gingival tissues. The replacement composite should also provide a sufficient range of gingival color options to enable suitable shade approximation and custom matching (Figure 3 and Figure 4).
Given the small and delicate gingival area being restored, it is also necessary for gingival composite materials to demonstrate ideal handling characteristics. These include a non-sticky texture and non-slumping flowable viscosity for precise placement and marginal adaptation. The material’s physical properties should include high radiopacity and high compressive strength.
Individualizing Pink Esthetic Dentistry
Among the armamentarium required for creating direct composite pink prosthetic restorations are pear-shaped diamonds for carefully cutting the micro box (Figure 5 and Figure 6) and a marginator fine flame diamond (ie, very small inverted cone diamond bur) to create undercuts or micromechanical retention (Figure 7 and Figure 8). Note that there is no radius beveling at the gingival margin; a butt joint is created that will require sealing.
After selectively etching, rinsing, and drying the enamel (Figure 9), a 7th generation bonding agent (eg, BeautiBond®, Shofu Dental)—or one with a 5-µm film thickness—is applied to the preparations using a brush applicator (eg, Benda® Brush, Centrix, www.centrixdental.com). Care must be taken to place the adhesive precisely to avoid debris along the gingival preparation lines to prevent tissue irritation. The adhesive should be air-thinned and light-cured (Figure 10 and Figure 11).
Because there are benefits to heating composites, such as enhanced flow capabilities in gingival areas, a composite warmer can be used. A ball burnisher (eg, #18, Hu-Friedy, www.hu-friedy.com) is an appropriate tool for transferring the composite. The first layer of gingival composite is placed, and a Goldstein microplacement instrument can be used to precisely work the margins prior to light-curing; this ensures no excess remains that could potentially cause gingival tissue inflammation or shrinkage (Figure 12). The sulcus and microtexture are created by placing a second layer of composite using the microplacement instrument and then curing (Figure 13).
To begin finishing pink restorations, a series of finishing discs, burs, and polishers are used. First, a high luster is created—even in the tight marginal areas—using polishing discs (eg, Super-Snap X-Treme™, Green, Shofu Dental) to help decrease the likelihood of microorganisms accumulating in voids and defects (Figure 14). Then, all margins can be approximated using a polishing disc with semi-spherical particles (eg, Super-Snap X-Treme, Red) (Figure 15). A one-step aluminum-oxide polisher (eg, OneGloss®, Shofu Dental) is then used prior to imparting the microtexture (Figure 16).
Then, to begin diffusing light—rather than create a high-shine, high-luster appearance—and imparting microtexture, the necessary armamentarium includes a yellow flamed diamond (Figure 17), while a green stone (eg, Dura-Green Stones, Shofu Dental) is used to diffuse the surface texture (Figure 18). The realistic luster synonymous with gingival tissue can be created using a small, synthetic velvet mini buff disc (eg, Super-Snap Mini Buff Disk, Shofu Dental) (Figure 19) and polishing paste.
Conclusion
The gingival architecture represents the framework for the teeth. Restoring the esthetics of this pink component of the smile, however, is not about precise shade matching or anatomical duplication. Rather, pink esthetics is fundamentally an illusion (Figure 20) that is a cost-effective, minimally invasive solution for many patients with gingival recession and an absence of pink. When created with new bioresponsive direct restorative materials, pink esthetic restorations also represent an opportunity for dentists to preserve their patient’s oral health.
REFERENCES
1. Zalkind M, Hochman N. Alternative method of conservative esthetic treatment for gingival recession. J Prosthet Dent.1997;77(6):561-563.
2. Bartlett DW, Shah P. A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85(4):306-312.
3. de Melo FV, Belli R, Monteiro S Jr, Vieira LC. Esthetic noncarious Class V restorations: a case report. J Esthet Restor Dent. 2005;17(5):275-284.
4. Kassab MM, Badawi H, Dentino AR. Treatment of gingival recession. Dent Clin North Am. 2010;54(1):129-140.
5. Ceruti P, Menicucci G, Mariani GD, et al. Non carious cervical lesions: a review. Minerva Stomatol. 2006;55(1-2):43-57.
6. Bartlett DW, Shah P. A critical review of non-carious cervical (wear) lesions and the role of abfraction, erosion, and abrasion. J Dent Res. 2006;85(4):306-312.
7. Blank LW, Caffesse RG, Charbeneau GT. The gingival response to well-finished composite resin restorations. J Prosthet Dent.1979;42(6):626-632.
8. Gordon VV, Mondragon E, Watson RE, et al. A clinical evaluation of a self-etching primer and a giomer restorative material: results at eight years. J Am Dent Assoc. 2007;138(5):621-627.
9. van Dijken JW, Sjöström S, Wing K. The effect of different types of composite resin fillings on marginal gingiva. J Clin Periondontol. 1987;14(4):185-189.
10. Coachman C, Salama M, Garber D, et al. Prosthetic gingival reconstruction in a fixed partial restoration. Part 1: introduction to artificial gingiva as an alternative therapy. Int J Periodontics Restorative Dent. 2009;29(5):471-477.
11. Wahbi, MA, Al Sharief HS, Tayeb H, Bokhari A. Minimally invasive use of coloured composite resin in aesthetic restoration of periodontially involved teeth: Case report. Saudi Dent J. 2013;25(2):83-89.
12. Salama M, Coachman C, Garber D, et al. Prosthetic gingival reconstruction in the fixed partial restoration. Part 2: diagnosis and treatment planning. Int J Periodontics Restorative Dent. 2009;29(6):573-581.
13. Coachman C, Salama M, Garber D, et al. Prosthetic gingival reconstruction in fixed partial restorations. Part 3: laboratory procedures and maintenance. Int J Periodontics Restorative Dent. 2010;30(1):19-29.
14. Zalkind M, Hochman N. Alternative method of conservative esthetic treatment for gingival recession. J Prosthet Dent. 1997;77(6):561-563.
15. Han L, Okamoto A, Fukushima M, Okiji T. Evaluation of a new fluoride-releasing one-step adhesive. Dent Mater J. 2006;25(3):509-515.
16. Perdigão J, Geraldeli S. Bonding characteristics of self-etching adhesives to intact versus prepared enamel. J Esthet Restor Dent. 2003;15(1):32-41.
17. Ikemura K, Tay FR, Endo T, Pashley DH. A review of chemical-approach and ultramorphological studies on the development of fluoride-releasing dental adhesives comprising new pre-reacted glass ionomer (PRG) fillers. Dent Mater J. 2008;27(3):315-339.