You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
The gingiva has a complex topography, and compared to a scalpel, a laser beam can more easily cut, ablate, and reshape the soft tissues in the oral cavity with very limited bleeding, less pain, and with no or less need for suturing.1 This encompasses a spectrum of tissue interactions, such as warming the tissue, welding, coagulation, protein denaturation, drying, and, finally, vaporization (ablation) and carbonization, where soft tissues are evaporated or incised.1-7 This process collectively provides hemostasis, microbial inhibition and destruction, and photobiomodulation (PBM).1-7 In particular, there is increasing evidence that the appropriate use of lasers is associated with reduced intraoperative and postoperative pain and increased wound healing or tissue regeneration, compared to conventional scalpel usage or electrosurgery.1-4 Literature suggests that electrosurgery can be used for incising soft tissues with good hemostasis1,5; however, it comes with a risk of delayed wound healing due to unwanted thermal damage1,6 and necrosis of the underlying periosteum and alveolar bone.
Laser Excision/Incision Vs. Scalpel Surgery
Dental lasers are used for soft-tissue procedures such as gingivectomy, gingivoplasty, frenectomy, and excision of benign connective tissue inflammatory hyperplastic lesions such as fibrous hyperplasia.8-10 In particular, lasers have proven to be effective for esthetic gingival procedures or as an adjunct to restorative dentistry, such as in recontouring of gingiva, depigmentation, and crown lengthening.1,11 Compared to conventional scalpel surgery, the diode laser cut is more precise and easier for the clinician to see because of the simultaneous cut and hemostasis effect.1,7,8,12 This leaves a clear and dry field, with minimal or no surgical bleeding.1,7,8 The laser also sterilizes as it cuts, and residual bacteria are evaporated, destroyed, or denatured by laser irradiation.1 Furthermore, the need for sutures is usually minimal.8
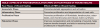
Laser incision with high-level laser therapy (HLLT) excises (ablates) diseased tissues, with simultaneous provision of low-level laser therapy (LLLT) that penetrates or scatters into the surrounding tissues during HLLT and stimulates tissues and cells without producing irreversible changes (Figure 1). LLLT promotes periodontal wound healing of the adjacent tissues as a desired effect,1,13,14 a process known as photobiomodulation (PBM) of tissues and cells following laser irradiation (Table 1).1 PBM can promote changes at the cell level and expression of cytokines that collectively promote wound healing by increasing collagen production, reducing inflammation, and supporting pain relief.1,15-61 Less wound contraction and edema also occur during mucosal healing; scars tend not to develop because less collateral damage occurs, and periodontal dressing is rarely required.7,62-65 These effects are attributed to the low-power (PBM) zones that surround the high-power surgical laser site,58 allowing faster or more favorable wound healing that requires less pain medication8 and leading to less postoperative discomfort compared to conventional scalpel surgery.1 The orthodontic treatment time can be shortened when soft-tissue procedures are needed that otherwise would require referral to other specialties such as a periodontist or oral surgeon. Therefore, the adjunctive use of soft-tissue lasers in orthodontics can attract fee-paying patients who demand optimal results in a timely fashion with minimal alterations in their eating and speech functions.8,62-65
Laser Wavelengths for Soft-Tissue Procedures
Various laser wavelengths have been used for soft-tissue procedures; the lasers work by ablating, incising, and excising the soft tissue, providing the much-needed coagulating effect. Frequently used soft-tissue lasers include: carbon dioxide [CO2] (9600 nm to 10600 nm); erbium (erbium-doped yttrium-aluminum-garnet [Er:YAG] (2940 nm) and erbium chromium-doped yttrium-scandium-gallium-garnet [Er,Cr:YSGG] (2780 nm)); neodymium doped yttrium-aluminum-garnet [Nd:YAG] (1064 nm); and diode (800 nm to 980 nm).1
Shallow or Deeply Penetrating Lasers and Hemostasis
Soft-tissue lasers can be sorted into two categories: deeply penetrating type lasers (near-infrared spectrum; approximately 800 nm to 1100 nm) and superficially absorbed lasers (CO2, Er:YAG, and Er,Cr:YSGG). The deeply penetrating type lasers, such as diode and Nd:YAG lasers, are essentially transmitted through water, showing a lower absorption coefficient in water.66 This explains their deep penetration into healthy soft tissue, in which the laser light infiltrates and scatters deeply.66 However, these lasers are selectively absorbed in areas of inflammation by blood components and tissue pigment (hemoglobin and melanin).66 There is also minimal to no interaction of Nd:YAG and diode lasers with healthy dental hard tissue (ie, not covered by calculus), which makes them suitable for soft-tissue procedures.66 The Nd:YAG laser is often used in pulsed mode, with very short duration pulses and an emission cycle (ratio of “on” time to total treatment time) of <1% and very high peak power per pulse (100 W to 1000 W).66 The Nd:YAG laser produces a relatively thick coagulation layer on the lased soft-tissue surface, exhibiting strong hemostasis, and, therefore, is effective for ablation of potentially hemorrhagic soft tissue. Diode lasers, representing a shallower penetration depth compared to Nd:YAG lasers, are less likely to cause pulpal damage after use.63 Diode lasers are used with power outputs ranging up to 20W, in a continuous-wave or pulse mode,7 and are ideal for use in orthodontic set-up due to the relatively small size of the laser device and lower cost.67
With the second category of soft-tissue lasers—the superficially absorbed lasers—the laser beam is absorbed in the superficial layer of tissue and does not penetrate or scatter deeply.1,68,69 These lasers have higher absorption coefficient in water and, due to the high water content of oral mucosa (>90%), are very effective soft-tissue lasers.63 However, their relatively high cost and poor portability and movement issues make them unattractive for the orthodontic set-up.63 Soft-tissue penetration depth for a CO2 laser is approximately 0.2 mm66,70; for erbium lasers (Er:YAG and Er,Cr:YSGG) it can be as shallow as 5 μm.66,68 CO2 lasers have the highest absorption in hydroxyapatite and calcium phosphate and must be used with care during soft-tissue procedures to avoid direct contact with hard tissue.66 Absorbed at the tissue surface with very little scatter or penetration1 the CO2 laser beam is associated with a relatively thin layer of coagulation around the ablated site. The ablation for the CO2 laser is basically caused by heat generation (charring or carbonization).1 Erbium lasers have the highest absorption into water, and they target water or the hydroxide ion as primary targets and mineral as a secondary target, and, therefore are used for ablation of both hard and soft tissues.66 Erbium lasers provide the most rapid, favorable, and uneventful wound healing due to their precise ablation with minimal thermal effects and their low inflammatory response.70 However, hemostasis is less effective with erbium lasers because of the minimal tissue denaturation, which guarantees subsequent sufficient bleeding and blood clot formation in the ablated defects and, thereby, induces favorable wound healing.6 Overall, erbium lasers provide the highest absorption into water, minimizing the thermal effects on the surrounding tissues during irradiation; however, the cost, relatively poor laser portability and movement, and less clear-cut incision morphology compared with CO2 and diode lasers70 are potential drawbacks for erbium lasers in orthodontic practice.
Tissue Ablation: Noncontact or Contact Cutting Mode
Most surgical lasers produce a photothermal effect on soft tissue, evaporating the tissues by thermal effects. Noncontact lasers such as CO2 or erbium lasers (Er:YAG and Er,Cr:YSGG) directly and easily evaporate soft tissues by photothermal effects. However, diode lasers used in dentistry do not have sufficient power to cut tissue in a noncontact mode, and therefore, the laser tip needs to be activated (initiated) by touching a substance to create a charring effect on the tip.71,72 In this process, part of the emitting light in diode lasers, as well as in Nd:YAG lasers, is converted into heat by refraction or diffused reflection at the tip end, or, in simple terms; the laser tip end gets initiated, creating a condition called “hot tip.” This initiation produces a secondary thermal effect at the heated tip end that can cut or incise soft tissue and offer coagulation of the tissue as a result of contact with the overheated tip rather than by the laser energy itself.1,2 Diode and Nd:YAG lasers produce a relatively thicker coagulation layer on the treated surface than superficially absorbed lasers.3
Diode lasers are considered to be ideal for daily practice of orthodontic soft-tissue procedures because they achieve sufficient hemostasis and cut precisely.73,74 The hydroxyapatite of tooth structure is mostly unaffected by diode laser wavelengths and the hot tip used is relatively safe around enamel without prolonged exposure, but it can leave a damaged area on root structure, dentin, or osseous tissue.66 For the purpose of this article the use of diode lasers for soft-tissue procedures will be discussed in greater detail because of their ease of use in orthodontics and lower operating cost.
Soft-Tissue Diode Lasers
Semiconductor (diode) lasers are mainly available in 810-nm to 830-nm, 940-nm, 980-nm, and 1064-nm wavelengths63,67; the 810-nm to 980-nm lasers are used most frequently. Diode lasers demonstrate high absorption coefficients in hemoglobin, particularly in oxyhemoglobin. However, diode laser light is poorly absorbed by hydroxyapatite and enamel62,63; thus, the diode laser is an excellent soft-tissue surgical laser for incising, excising, and coagulating gingiva and mucosa. The active mediums of semiconductor (diode) lasers are varied and can include aluminum (Al), gallium arsenide (GaAs), and occasionally indium.63,75,76 Examples are gallium-aluminum-arsenic (Ga-Al-As), arsenic-gallium (As-Ga), and indium-gallium-aluminum-phosphide (In-Ga-Al-P) lasers. Besides being portable (<5 Kg), small, relatively inexpensive, and simple to use, diode lasers have a stable power output, long lifetime, and low installation and maintenance costs.75
Fiberoptic Tip Size, Power Output, and Continuous/Pulsed Mode
The diode laser is delivered by a fine glass fiber with a fiber system tip that can be angled, so that the dentist can hold it similar to a pencil for accurate manipulation, which is especially beneficial in difficult-to-handle areas.75 For surgical incisions and excision, a 400-μm-diameter fiberoptic tip is recommended, because smaller-diameter fibers tend to be more friable.76 The fiberoptic tip requires initiation prior to performing surgical excision; this is often done by tapping the initiated tip on a thick blue articulating paper, using black ink or a solid color in a magazine page, or using a piece of cork.63,73,77 Diode lasers with power outputs of <500 mW are used in LLLT to provide biomodulation, wound repair, and pain relief.63 However, to perform excision a continuous power output of 1 W to 1.5 W is often needed,77 depending on the fibrotic nature of the tissue. To decrease carbonization and thermal damage and allow for thermal recovery of the tissue, the pulsed mode has been suggested and implemented in many contemporary diode laser units.78
Anesthesia and Basic Soft-Tissue Guidelines
Diode laser soft-tissue surgery is often performed using local infiltration (eg, 2% lidocaine) approximately 5 minutes before the procedure; however, literature also reports using topical lignocaine anesthetic gel, applied for 3 minutes,79 or nonregulated compound topical anesthetics such as TAC Alternate for 3 minutes (20% lidocaine, 4% tetracaine, and 2% phenylephrine).76,77,80 To confirm adequate anesthesia prior to laser soft-tissue surgery, the clinician can gently probe the soft tissue.
Following surgical excision, the soft-tissue margins can appear dark and charred (carbonized), and the use of a high-speed suction is recommended to remove laser plume and objectionable charred odor.76,77 The remnants of carbonized tissue at the surgical margins can be removed using sterile gauze dampened with saline79 or a microapplicator brush soaked in 3% hydrogen peroxide solution.77
Various manufacturers present different arrangements for diode lasers with respect to output power, diameter of fiber, and wavelength. Though these parameters may influence collateral tissue damage, there is currently a lack of standardization in setting optimum parameters of diode laser for orthodontic soft-tissue procedures, a matter that should be investigated in future studies.81
Diode lasers are useful in recontouring the gingiva to gain access to the clinical crown in cases of gingival overgrowth or partially erupted teeth, which prevents the proper positioning of a bracket. When planning laser soft-tissue procedures, the general guideline is to leave at least 1 mm of pocket depth and preserve at least 2 mm of keratinized tissue to avoid further soft-tissue complications such as gingival recession.63 The aforementioned guidelines are based on the “biologic width” concept, as measured from the free gingival margin to the crestal bone, which is approximately 3 mm, consisting of, on average, 1 mm of junctional epithelium, 1 mm of connective tissue attachment, and a gingival sulcus depth of approximately 1 mm.63,76 To decide whether to use a conventional flap approach or laser gingivectomy, the gingivectomy location should be probed, and the amount of attached gingiva, the location of the crest of bone, and the desired amount of crown lengthening should be considered based on the limitations of the biologic width. In other words, an average of 3 mm of soft tissue will rebound (regrow) coronal to the alveolar crest in about 3 months.82
Laser Gingivectomy to Improve Oral Hygiene or Bracket Positioning
Gingival enlargement or hyperplasia is a common side effect of fixed orthodontic therapy, occurring in almost 10% of orthodontic patients.81,83 Gingival enlargement often impedes the maintenance of oral hygiene, causing esthetic and functional problems, and has been reported to compromise orthodontic tooth movement.81,84,85 Conventional treatment for gingival enlargement often includes oral hygiene instruction, scaling, root planing, and prophylaxis; however, extensive and often fibrotic gingival enlargement compromises self-care and may necessitate gingivectomy to maintain oral health.81,86 The adjunct use of diode laser gingivectomy can in a shorter amount of time further improve the gingival health of a patient with gingival enlargement.81 Figure 2 through Figure 5 depict a case of gingival hyperplasia that was successfully managed using diode laser.
In addition, laser gingivectomy can be performed to remove excess soft tissue and expose the crown of a partially erupted tooth, allowing brackets to be placed properly—ideally in the center of the teeth—to enable an improved level of hygiene maintenance during treatment (Figure 6 through Figure 8).63,87
Esthetic Laser Gingival Recontouring
Oftentimes during treatment or when debonding a case, the clinician may come across unsightly gingival margins that do not conform to the principles of smile esthetics and present with short or uneven crown heights, disproportionate tooth proportionality ratios, and unesthetic enlarged and fibrotic interdental papillae and gingival margins.7 Procedures to improve esthetics such as crown lengthening or papillae flattening can be technically demanding tasks in that the gingival margins sometimes need minor recontouring that requires a higher degree of precision than that achieved with a scalpel blade, regardless of the operator’s skill level.88 Diode lasers offer precise incision control because of minimal bleeding and a clear, dry field during surgery. Figure 9 and Figure 10 show a female patient who underwent localized gingival recontouring of the maxillary left central and lateral incisors.
Laser Exposure of Superficially Impacted Teeth
One of the interesting applications of diode lasers is for exposure of superficially impacted teeth, in particular maxillary permanent canines, which are the most frequently impacted tooth after third molars (0.92% to 4.3%).89,90 The conventional approach is to orthodontically create sufficient space for the impacted tooth and wait for it to erupt, which could delay treatment for months and adversely affect treatment efficacy. Alternatively, an apically positioned flap (buccally/labially positioned tooth) or full-thickness mucoperiosteal flap (palatally positioned tooth) could be raised using closed/open eruption techniques, and an orthodontic attachment subsequently bonded to the impacted tooth.77,91,92 This would involve use of a scalpel, leading to considerable bleeding and pain. Bonding orthodontic attachments requires a dry field and use of hydrophilic moisture-insensitive primers.92 The orthodontic traction should begin as soon as possible after exposure if the open eruption technique is not intended.92
The localization of the impacted tooth prior to laser exposure is vital to establish whether the impacted tooth is positioned superficially and is not covered completely by bone, or referral to an oral surgeon or periodontist is needed. The clinician carries out visual inspection and digital palpation; however, the presence of a labial bulge does not guarantee access to the crown after soft-tissue exposure, as a clinical crown might be fully covered by alveolar bone. The localization should be based on both clinical (ie, blanching of tissue with finger pressure) and, if there is any doubt, supplemental radiographic examination.93 Approximately 85% of canine impactions occur palatally and 15% buccally.93-95
Diode laser exposure is not applicable in cases of impaction of teeth fully covered by cortical bone. In these cases a conventional full-thickness mucoperiosteal flap (palatal impaction) or an apically positioned flap (buccal impaction) and removal of cortical bone until the crown portion of the retained tooth is exposed may be necessary. When superficially impacted teeth are present, it is recommended that sufficient space be created before the surgical laser exposure to facilitate bonding an eyelet or bracket and applying orthodontic forces immediately after laser exposure.92
Figure 11 depicts a male patient with a buccally impacted maxillary right canine. Figure 12 shows the tooth right after laser exposure, and Figure 13 shows it 24 hours after the laser treatment. Note that the amount of inflammation is minimal. Figure 14 illustrates the laser exposure site at approximately 6 weeks’ follow-up.
Superficially palatally impacted permanent maxillary canines are good candidates for laser exposure (Figure 15 through Figure 18). The remarkable healing process can be seen in a male patient with a palatally impacted maxillary right canine (Figure 15), immediately after palatal laser exposure (Figure 16), and at 2 weeks post-treatment (Figure 17). Finally, at 4 months’ follow-up (Figure 18) a thick band of keratinized gingiva is evident. Such laser exposure treatment on a superficially palatally impacted canine can be used as an alternative to a full-thickness mucoperiosteal flap.
All cases demonstrated were performed using a 940-nm InGaAsP diode laser (Epic™ 10, Biolase, www.biolase.com), with a 400-μm diameter fiberoptic tip, and after initiation.
Postoperative Instruction
Postoperatively, the lased area should be kept clean, using a soft-bristle toothbrush (or cotton swab), or rinsing the mouth with salt water several times daily for a few days and removing any remaining tissue with a wet cotton swab.7,63 Vitamin E gel can be rubbed over the treated area to aid in healing and keep the area moist, and over-the-counter analgesics can be taken such as acetaminophen for pain control.63,81
Other Soft Tissue Orthodontic Applications and Future Research
Diode lasers have been used to uncover temporary anchorage devices (TADs), perform frenectomies where highly attached frenum is impeding tooth movement in diastema cases, remove operculum on mandibular second molars that prevents banding, or improve healing of minor aphthous ulceration following placement of fixed orthodontic braces.7,63,77 Presently, there is limited information on the variables the affect the efficiency of diode lasers for soft tissue procedures (continues of pulsed mode, wavelength, power output, fiber optic diameter).96 Further, the diode laser family is also expanding and there is a need for further research.97,98
Summary
The adjunct use of a diode laser can potentially improve the esthetic outcome of orthodontic treatment, decrease treatment duration in situations where surgical exposure of superficially impacted teeth is needed, and collectively reduce the number of appointments. Compared to conventional scalpel surgery, lasers offer a quicker, bloodless, and less painful alternative with improved healing potential.
About the Author
Ali Borzabadi-Farhani, DDS, MScD, MOrth RCS (Ed), Fellowship (Craniofac Orth, CHLA/USC)
Visiting Professor (Orthodontics)
Department of Clinical Sciences and Translational Medicine
University of Rome Tor Vergata
Rome, Italy
Specialist Orthodontist
London, England
Referneces
1. Aoki A, Mizutani K, Schwarz F, et al. Periodontal and peri-implant wound healing following laser therapy. Periodontol 2000. 2015;68(1):217-269.
2. Aoki A, Mizutani K, Takasaki AA, et al. Current status of clinical laser applications in periodontal therapy. Gen Dent. 2008:56(7):674-687.
3. Aoki A, Sasaki K, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontol 2000. 2004:36:59-97.
4. Pang P, Andreana S, Aoki A, et al. Laser energy in oral soft tissue applications. J Laser Dent. 2010;18(3):123–31.
5. Takei HH, Carranza FA. Gingival surgical techniques. In: Newman MG, Takei HH, Klokkevold PR, Carranza FA, eds. Carranza’s Clinical Periodontology. 10th ed. St. Louis, MO: Elsevier; 2006:915.
6. Sawabe M, Aoki A, Komaki M, et al. Gingival tissue healing following Er:YAG laser ablation compared to electrosurgery in rats. Lasers Med Sci. 2015;30(2):875-883.
7. Sarver DM, Yanosky M. Principles of cosmetic dentistry in orthodontics: part 2. Soft tissue laser technology and cosmetic gingival contouring. Am J Orthod Dentofacial Orthop. 2005;127(1):85-90.
8. Amaral MB, de Avila JM, Abreu MH, Mesquita RA. Diode laser surgery versus scalpel surgery in the treatment of fibrous hyperplasia: a randomized clinical trial. Int J Oral Maxillofac Surg. 2015;44(11):1383-1389.
9. Mathur E, Sareen M, Dhaka P, Baghla P. Diode laser excision of oral benign lesions. J Lasers Med Sci. 2015;6(3):129-132.
10. Parker S. Lasers and soft tissue: ‘fixed’ soft tissue surgery. Br Dent J. 2007;202(5):247-253.
11. Parker S. Lasers and soft tissue: ‘loose’ soft tissue surgery. Br Dent J. 2007;202(4):185-191.
12. Fornaini C, Merigo E, Sozzi M, et al. Four different diode lasers comparison on soft tissues surgery: a preliminary ex vivo study. Laser Ther. 2016;25(2):105-114.
13. Aoki A, Takasaki A, Pourzarandian A, et al. Photobiomodulation laser strategies in periodontal therapy. In: Waynant R, Tata DB, eds. Proceedings of Light-Activated Tissue Regeneration and Therapy II. New York, NY: Springer; 2008:181-190.
14. Izumi Y, Aoki A, Yamada Y, et al. Current and future periodontal tissue engineering. Periodontol 2000. 2011:56(1):166-187.
15. Mester E, Spiry T, Szende B, Tota JG. Effect of laser rays on wound healing. Am J Surg. 1971:122(4):532-535.
16. Enwemeka CS, Parker JC, Dowdy DS, et al. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004:22(4):323-329.
17. Woodruff LD, Bounkeo JM, Brannon WM, et al. The efficacy of laser therapy in wound repair: a meta-analysis of the literature. Photomed Laser Surg. 2004:22(3):241-247.
18. Albertini R, Villaverde AB, Aimbire F, et al. Anti-inflammatory effects of low-level laser therapy (LLLT) with two different red wavelengths (660 nm and 684 nm) in carrageenan-induced rat paw edema. J Photochem Photobiol B. 2007:89(1):50-55.
19. Bjordal JM, Johnson MI, Iversen V, et al. Low-level laser therapy in acute pain: a systematic review of possible mechanisms of action and clinical effects in randomized placebo-controlled trials. Photomed Laser Surg. 2006:24(2):158-168.
20. Enwemeka CS, Parker JC, Dowdy DS, et al. The efficacy of low-power lasers in tissue repair and pain control: a meta-analysis study. Photomed Laser Surg. 2004:22(4):323-329.
21. Isman E, Aras MH, Cengiz B, et al. Effects of laser irradiation at different wavelengths (660, 810, 980, and 1064 nm) on transient receptor potential melastatin channels in an animal model of wound healing. Lasers Med Sci. 2015;30(5):1489-1495.
22. Ogita M, Tsuchida S, Aoki A, et al. Increased cell proliferation and differential protein expression induced by low-level Er:YAG laser irradiation in human gingival fibroblasts: proteomic analysis. Lasers Med Sci. 2015;30(7):1855-1866.
23. Dias SB, Fonseca MV, Dos Santos NC, et al. Effect of GaAIAs low-level laser therapy on the healing of human palate mucosa after connective tissue graft harvesting: randomized clinical trial. Lasers Med Sci. 2015;30(6):1695-1702.
24. de Melo Rambo CS, Silva JA Jr, Serra AJ, et al. Comparative analysis of low-level laser therapy (660 nm) on inflammatory biomarker expression during the skin wound-repair process in young and aged rats. Lasers Med Sci. 2014;29(5):1723-1733.
25. Liao X, Xie GH, Liu HW, et al. Helium-neon laser irradiation promotes the proliferation and migration of human epidermal stem cells in vitro: proposed mechanism for enhanced wound re-epithelialization. Photomed Laser Surg. 2014;32(4):219-225.
26. Fujimura T, Mitani A, Fukuda M, et al. Irradiation with a low-level diode laser induces the developmental endothelial locus-1 gene and reduces proinflammatory cytokines in epithelial cells. Lasers Med Sci. 2014;29(3):987-994.
27. Batista JD, Sargenti-Neto S, Dechichi P, et al. Low-level laser therapy on bone repair: is there any effect outside the irradiated field? Lasers Med Sci. 2015;30(5):1569-1574.
28. Pinheiro AL, Aciole GT, Ramos TA, et al. The efficacy of the use of IR laser phototherapy associated to biphasic ceramic graft and guided bone regeneration on surgical fractures treated with miniplates: a histological and histomorphometric study on rabbits. Lasers Med Sci. 2014;29(1):279-288.
29. de Vasconcellos LM, Barbara MA, Deco CP, et al. Healing of normal and osteopenic bone with titanium implant and low-level laser therapy (GaAlAs): a histomorphometric study in rats. Lasers Med Sci. 2014;29(2):575-580.
30. Tim CR, Pinto KN, Rossi BR, et al. Low-level laser therapy enhances the expression of osteogenic factors during bone repair in rats. Lasers Med Sci. 2014;29(1):147-156.
31. Pagin MT, de Oliveira FA, Oliveira RC, et al. Laser and light-emitting diode effects on preosteoblast growth and differentiation. Lasers Med Sci. 2014;29(1):55-59.
32. Peccin MS, de Oliveira F, Muniz Renno AC, et al. Helium-neon laser improves bone repair in rabbits: comparison at two anatomic sites. Lasers Med Sci. 2013;28(4):1125-1130.
33. Boldrini C, de Almeida JM, Fernandes LA, et al. Biomechanical effect of one session of low-level laser on the bone-titanium implant interface. Lasers Med Sci. 2013;28(1):349-352.
34. Pinheiro AL, Soares LG, Barbosa AF, et al. Does LED phototherapy influence the repair of bone defects grafted with MTA, bone morphogenetic proteins, and guided bone regeneration? A description of the repair process on rodents. Lasers Med Sci. 2012;27(5):1013-1024.
35. Rosa AP, de Sousa LG, Regalo SC, et al. Effects of the combination of low-level laser irradiation and recombinant human bone morphogenetic protein-2 in bone repair. Lasers Med Sci. 2012;27(5):971-977.
36. Anders JJ, Moges H, Wu X, et al. In vitro and in vivo optimization of infrared laser treatment for injured peripheral nerves. Lasers Surg Med. 2014;46(1):34-45.
37. Takhtfooladi MA, Jahanbakhsh F, Takhtfooladi HA, et al. Effect of low-level laser therapy (685 nm, 3 J/cm(2)) on functional recovery of the sciatic nerve in rats following crushing lesion. Lasers Med Sci. 2015;30(3):1047-1052.
38. Masoumipoor M, Jameie SB, Janzadeh A, et al. Effects of 660- and 980-nm low-level laser therapy on neuropathic pain relief following chronic constriction injury in rat sciatic nerve. Lasers Med Sci. 2014;29(5):1593-1598.
39. Gasperini G, de Siqueira IC, Costa LR. Lower-level laser therapy improves neurosensory disorders resulting from bilateral mandibular sagittal split osteotomy: a randomized crossover clinical trial. J Craniomaxillofac Surg. 2014;42(5):e130-e133.
40. Akgul T, Gulsoy M, Gulcur HO. Effects of early and delayed laser application on nerve regeneration. Lasers Med Sci. 2014;29(1):351-357.
41. Lazovic M, Ilic-Stojanovic O, Kocic M, et al. Placebo-controlled investigation of low-level laser therapy to treat carpal tunnel syndrome. Photomed Laser Surg. 2014;32(6):336-344.
42. de Sousa AP, Paraguassu GM, Silveira NT, et al. Laser and LED phototherapies on angiogenesis. Lasers Med Sci. 2013;28(3):981-987.
43. Goralczyk K, Szymańska J, Łukowicz M, et al. Effect of LLLT on endothelial cells culture. Lasers Med Sci. 2015;30(1):273-278.
44. Ogita M, Tsuchida S, Aoki A, et al. Increased cell proliferation and differential protein expression induced by low-level Er:YAG laser irradiation in human gingival fibroblasts: proteomic analysis. Lasers Med Sci. 2015;30(7):1855-1866.
45. Esmaeelinejad M, Bayat M, Darbandi H, et al. The effects of low-level laser irradiation on cellular viability and proliferation of human skin fibroblasts cultured in high glucose mediums. Lasers Med Sci. 2014;29(1):121-129.
46. Pellicioli AC, Martins MD, Dillenburg CS, et al. Laser phototherapy accelerates oral keratinocyte migration through the modulation of the mammalian target of rapamycin signaling pathway. J Biomed Opt. 2014;19(2):028002.
47. Basso FG, Oliveira CF, Kurachi C, et al. Biostimulatory effect of low-level laser therapy on keratinocytes in vitro. Lasers Med Sci. 2013;28(2):367-374.
48. Fujihara NA, Hiraki KR, Marques MM. Irradiation at 780 nm increases proliferation rate of osteoblasts independently of dexamethasone presence. Lasers Surg Med. 2006;38(4):332-336.
49. Goncalves RV, Novaes RD, Matta SL, et al. Comparative study of the effects of gallium-aluminum-arsenide laser photobiomodulation and healing oil on skin wounds in Wistar rats: a histomorphometric study. Photomed Laser Surg. 2010;28(5):597-602.
50. Xavier M, David DR, Souza RA, et al. Anti-inflammatory effects of low-level light emitting diode therapy on Achilles tendinitis in rats. Lasers Surg Med. 2010;42(6):553-558.
51. Novaes RD, Goncalves RV, Cupertino MC, et al. The energy density of laser light differentially modulates the skin morphological reorganization in a murine model of healing by secondary intention. Int J Exp Pathol. 2014;95(2):138-146.
52. Posten W, Wrone DA, Dover JS, et al. Low-level laser therapy for wound healing: mechanism and efficacy. Dermatol Surg. 2005;31(3):334-340.
53. Houreld NN, Sekhejane PR, Abrahamse H. Irradiation at 830 nm stimulates nitric oxide production and inhibits pro-inflammatory cytokines in diabetic wounded fibroblast cells. Lasers Surg Med. 2010;42(6):494-502.
54. Pogrel MA, Chen JW, Zhang K. Effects of low-energy gallium-aluminum-arsenide laser irradiation on cultured fibroblasts and keratinocytes. Lasers Surg Med. 1997;20(4):426-432.
55. Martignago CC, Oliveira RF, Pires-Oliveira DA, et al. Effect of low-level laser therapy on the gene expression of collagen and vascular endothelial growth factor in a culture of fibroblast cells in mice. Lasers Med Sci. 2015;30(1):203-208.
56. Goncalves RV, Mezencio JM, Benevides GP, et al. Effect of gallium-arsenide laser, gallium-aluminum-arsenide laser and healing ointment on cutaneous wound healing in Wistar rats. Braz J Med Biol Res. 2010;43(4):350-355.
57. Avci P, Gupta A, Sadasivam M, et al. Low-level laser (light) therapy (LLLT) in skin: stimulating, healing, restoring. Semin Cutan Med Surg. 2013;32(1):41-52.
58. Khan I, Arany P. Biophysical approaches for oral wound healing: emphasis on photobiomodulation. Adv Wound Care (New Rochelle). 2015;4(12):724-737.
59. Tuner J, Beck-Kristensen PH, Ross G, Ross A. Photobiomodulation in dentistry. In: Convissar RA, ed. Principles and Practice of Laser Dentistry. 2nd ed. St. Louis, MO: Elsevier Mosby; 2016:251-274.
60. AlGhamdi KM, Kumar A, Moussa NA. Low-level laser therapy: a useful technique for enhancing the proliferation of various cultured cells. Lasers Med Sci. 2012;27(1):237-249.
61. Borzabadi-Farahani A. Effect of low-level laser irradiation on proliferation of human dental mesenchymal stem cells; a systemic review. J Photochem Photobiol B. 2016;162:577-582.
62. Kang Y, Rabie AB, Wong RW. A review of laser applications in orthodontics. Int J Orthod Milwaukee. 2014;25(1):47-56.
63. Chmura LG, Convissar RA. Lasers in orthodontics. In: Convissar RA, ed. Principles and Practice of Laser Dentistry. 2nd ed. St. Louis, MO: Elsevier Mosby; 2016:203-219.
64. Romanos G, Nentwig GH. Diode laser (980 nm) in oral and maxillofacial surgical procedures: clinical observations based on clinical applications. J Clin Laser Med Surg 1999;17(5):193-197.
65. Aldelaimi TN, Khalil AA. Clinical application of diode laser (980 nm) in maxillofacial surgical procedures. J Craniofac Surg. 2015;26(4):1220-1223.
66. Mizutani K, Aoki A, Coluzzi D, et al. Lasers in minimally invasive periodontal and peri-implant therapy. Periodontol 2000. 2016;71(1):185-212.
67. Migliorati EK, de Almeida Rosa DS. Regenerative laser periodontal therapy. In: Convissar RA, ed. Principles and Practice of Laser Dentistry. 2nd ed. St. Louis, MO: Elsevier Mosby; 2016:67-88.
68. Ishikawa I, Aoki A, Takasaki AA, et al. Application of lasers in periodontics: true innovation or myth? Periodontol 2000. 2009;50:90-126.
69. Pang P, Andreana S, Aoki A, et al. Laser energy in oral soft tissue applications. J Laser Dent. 2011;18(3):123-131.
70. Merigo E, Clini F, Fornaini C, et al. Laser-assisted surgery with different wavelengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci. 2013;28(2):497-504.
71. Bornstein E. Near-infrared dental diode lasers. Scientific and photobiologic principles and applications. Dent Today. 2004;23(3):102-108.
72. Strauss RA, Magid KS. Esthetics and laser surgery. In: Aschheim KW, ed. Esthetic Dentistry: A Clinical Approach to Techniques and Materials. 3rd ed. St. Louis, MO: Elsevier Mosby; 2015:446-454.
73. Goharkhay K, Moritz A, Wilder-Smith P, et al. Effects on oral soft tissue produced by a diode laser in vitro. Lasers Surg Med. 1999;25(5):401-406.
74. Jin JY, Lee SH, Yoon HJ. A comparative study of wound healing following incision with a scalpel, diode laser or Er,Cr:YSGG laser in guinea pig oral mucosa: A histological and immunohistochemical analysis. Acta Odontol Scand. 2010;68(4):232-238.
75. Arroyo HH, Neri L, Fussuma CY, Imamura R. Diode Laser for Laryngeal Surgery: a Systematic Review. Int Arch Otorhinolaryngol. 2016;20(2):172-179.
76. Tracey S. Lasers in orthodontics. Academy of Dental Therapeutics and Stomatology. 2011. www.ineedce.com/courses/2028/PDF/1103cei_laser_ortho_web3.pdf. Accessed June 23, 2016.
77. Kravitz ND. The application of lasers in orthodontics. In: Krishnan V, Davidovitch Z, eds. Integrated Clinical Orthodontics. West Sussex, UK: John Wiley & Sons, Ltd.; 2012:422-443.
78. Colluzzi DJ. Fundamentals of dental lasers: science and instruments. Dent Clin North Am. 2004;48(4):751-770.
79. Prabhu M, Ramesh A, Thomas B. Treatment of orthodontically induced gingival hyperplasia by diode laser - case report. Nitte Univ J Health Sci. 2015;5(2):66-68.
80. Kravitz ND, Graham JW, Nicozisis JL, Gill J. Compunded topical anesthetics in orthodontics. J Clin Orthod. 2015;49(6):371-377.
81. To TN, Rabie AB, Wong RW, McGrath CP. The adjunct effectiveness of diode laser gingivectomy in maintaining periodontal health during orthodontic treatment. Angle Orthod. 2013;83(1):43-47.
82. Hempton TJ, Dominici JT. Contemporary crown-lengthening therapy: a review. J Am Dent Assoc. 2010;141(6):647-655.
83. Kloehn JS, Pfeifer JS. The effect of orthodontic treatment on the periodontium. Angle Orthod. 1974;44(2):127-134.
84. Palomo L, Palomo JM, Bissada NF. Salient periodontal issues for the modern biologic orthodontist. Semin Orthod. 2008;14(4):229-245.
85. Camargo PM, Melnick PR, Pirih FQ, et al. Treatment of drug-induced gingival enlargement: aesthetic and functional considerations. Periodontol 2000. 2001;27:131-138.
86. de Oliveira Guare R, Costa SC, Baeder F, et al. Drug-induced gingival enlargement: biofilm control and surgical therapy with gallium–aluminum–arsenide (GaAlAs) diode laser-A 2-year follow-up. Spec Care Dentist. 2010;30(2):46-52.
87. Sarver DM, Yanosky M. Principles of cosmetic dentistry in orthodontics: Part 3. Laser treatments for tooth eruption and soft tissue problems. Am J Orthod Dentofacial Orthop. 2005;127(2):262-264.
88. Lee EA. Laser-assisted gingival tissue procedures in esthetic dentistry. Pract Proced Aesthet Dent. 2006;18(9):suppl 2-6.
89. Ericson S, Kurol J. Radiographic assessment of maxillary canine eruption in children with clinical signs of eruption disturbance. Eur J Orthod. 1986;8(3):133-140.
90. Pini-Prato G, Mancini EA, Papini O, Crescini A. Mucogingival approaches in young orthodontic patients: Combined strategies for success. Semin Orthod. 2014;20(3):150-169.
91. Bedoya MM, Park JH. A review of the diagnosis and management of impacted maxillary canines. J Am Dent Assoc. 2009;140(12):1485-1493.
92. Kanning NC, Curtice SA, Haggerty CJ. Exposure and bonding of an impacted tooth. In: Haggerty CJ, Laughlin RM, eds. Atlas of Operative Oral and Maxillofacial Surgery. Hoboken, NJ: John Wiley & Sons, Inc.; 2015:7-13.
93. Wriedt S, Jaklin J, Al-Nawas B, Wehrbein H. Impacted upper canines: examination and treatment proposal based on 3D versus 2D diagnosis. J Orofac Orthop. 2012;73(1):28-40.
94. Hitchin AD. The impacted maxillary canine. Dent Pract Dent Rec. 1956;2(4):100-103.
95. Counihan K, Al-Awadhi EA, Butler J. Guidelines for the assessment of the impacted maxillary canine. Dent Update. 2013;40(9):770-777.
96. Fornaini C, Merigo E, Sozzi M, et al. Four different diode lasers comparison on soft tissues surgery: a preliminary ex vivo study. Laser Therapy. 2016;25(2):105-114.
97. Fornaini C, Merigo E, Rocca JP, et al. 450 nm blue laser and oral surgery: Preliminary ex vivo study. J Contemp Dent Pract. 2016;17(10):795-800.
98. Fornaini C, Rocca JP, Merigo E, et al. Low energy KTP laser in oral soft tissues surgery: A 52 patients clinical study. Medicina Oral, Patología Oral y Cirugía Bucal. 2012;17(2):e287-e291.