You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Head and neck cancer is the sixth most common cancer worldwide,1 with 630,000 newly diagnosed cases and 350,000 deaths per year.1,2 Most cases of oral cancer are not diagnosed until they are in advanced stages (III or IV),2,3 resulting in a 5-year survival rate less than 30%.4,5 With early detection, prognosis can improve with 5-year survival rates increasing from 30% to over 80%.6 However, early detection depends on thorough and frequent comprehensive oral cancer examinations.
Dental hygienists are educated to perform these potentially life-saving comprehensive oral cancer examinations. Curricula of entry-level dental hygiene educational programs provide fundamental knowledge about oral cancer lesions, as well as the theoretical background and clinical experience performing oral cancer examinations. The Commission on Dental Accreditation requires that dental hygiene graduates be competent in performing oral cancer examinations. A comprehensive oral cancer examination includes the steps outlined in Table 1. Palpation of the head and neck lymph nodes and oral mucosa is integral to a comprehensive oral cancer examination.5,7 In clinical practice dental hygienists have the opportunity to document and frequently monitor any abnormalities of the oral soft tissues noted at their patients’ regular dental hygiene appointments. However, past research revealed 66% of surveyed dental hygienists reported conducting oral cancer examinations,6 and 50% reported employing bimanual neck palpation in their assessment.5
While past studies have examined dental hygienists’ oral cancer screening-related knowledge, attitudes, and behaviors, factors influencing detection of early-stage lesions by dental hygienists are still unknown. Therefore, the purpose of this study was to assess the knowledge, practices, attitudes, barriers, and facilitators of early-stage oral cancer detection by California dental hygienists using an electronic survey approach.
Methods and Materials
This quantitative, cross-sectional study was approved by the Institutional Review Board of the University of California, San Francisco. The study population consisted of dental hygienists whose email addresses were in the California Dental Hygienists’ Association (CDHA) database. The database included both members and nonmembers of CDHA. CDHA distributed an email message to potential participants, which included a recruitment cover letter, the study purpose, contact information, informed consent, and a link to the online survey.
The 20-item survey, which included conditional branching and multiple-choice questions, was developed by the authors based on previous related research. Questions from established surveys were examined for content and format and used when appropriate. The survey assessed the following: knowledge of visual appearance of lesions, oral cancer examination practices and attitudes, the barriers and facilitators of bringing a suspicious lesion to the attention of the dentist, and demographic information. The survey instrument was pilot tested by 15 dental hygienists for acceptability and feasibility, and modifications were made based on feedback received.
CDHA sent two follow-up email messages to all respondents 3 weeks and 6 weeks following the initial mailing, requesting nonresponders to complete the survey. Survey responses were recorded and compiled by Qualtrics online survey research suite.8
Descriptive statistics of the survey questions were calculated among the observed respondents and are presented as the frequency (percentage) for categorical variables and mean and standard deviation (SD) for variables measured on a continuous scale. A knowledge score of oral cancer was assessed for each respondent based on six images of oral lesions. Survey respondents were requested to view images of oral lesions and specify whether the lesions were suspicious or not. Each correct response to a knowledge question was awarded a single point with a maximum of six points. An average oral cancer knowledge score was calculated if at least half of the six questions relating to the knowledge assessment had responses; otherwise, the average cancer knowledge score was considered missing.
Logistic regression analysis was used to independently explore whether there was an association between respondents who reported conducting palpations of oral tissues (outcome) with respondents who knew someone with oral cancer (independent variable) or had previously detected a cancerous lesion (independent variable). Also explored was whether the combination of both knowing a person with oral cancer and previously detecting a cancerous lesion was associated with conducting palpations (outcome). Associations are reported as odds ratios (OR) with corresponding 95% confidence intervals (CI) among the observed data (n = 685/751 or 91%). Statistical analyses used SAS version 9.4 (SAS Institute, www.sas.com). All statistical tests provided two-sided P-values, and P-values (P) < .05 were considered statistically significant.
Results
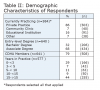
Of the 6,248 dental hygienists whose email addresses were in the CDHA database, 751 responded to the online survey, yielding a response rate of 12%. Almost all (91%) of the respondents were currently practicing. Most respondents reported graduating from an associate degree program, practicing in a private dental office, and were either early in their career (0 to 3 years), or had been practicing for over 15 years (Table 2).
The percentage of respondents correctly identifying the oral lesions presented as suspicious for oral cancer or not ranged from 40% to 97% (Figure 1 through Figure 6 show respondents’ knowledge of cancerous lesions, based on identification of photographic images). Ninety-one percent (n = 684/751) responded to at least three of the six knowledge questions, and therefore an average knowledge score was calculated for those respondents with an average knowledge score of 77% (standard deviation = 16%). Figure 2 depicted an early, less pronounced lesion, erythroplakia, and resulted in only 40% of the respondents correctly identifying it as suspicious for cancer.
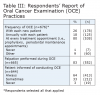
Most respondents reported that they conducted an oral cancer examination at every treatment appointment (Table 3). Only 1% of participants reported having never conducted an oral cancer examination. The most commonly reported factor associated with not conducting an oral cancer examination was that a supervising dentist conducted the OCE. A minority of respondents indicated that they never inform their patients that they are conducting an oral cancer examination. The inclusion of palpation during the OCE was reported by most participants.
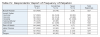
The frequency of palpation varied by region of the mouth and head/neck (Table 4). The labial mucosa was always palpated by 87% of the respondents. While 32% reported that they never palpate occipital lymph nodes, 97% of the respondents indicated palpation was important. The areas reported to be less important to palpate included the occipital lymph nodes and tongue. Respondents who conducted palpations were more likely to report knowing a person with oral cancer (OR = 1.3, 95% CI: 0.9 to 1.9, P = .24) and previously detecting an oral cancer lesion (OR = 1.2, 95% CI: 0.8 to 1.8, P = .3) than those who did not. Those who reported both knowing someone with oral cancer and previously detecting an oral cancer lesion were 3.3 (95% CI: 1.4 to 7.9, P = .006) times more likely to conduct palpations than those who did not.
Table 5 describes the self-reported frequency of visual examination. The majority of the respondents reported “always” as the frequency of examination of the oral regions included in OCE. For example, 98% indicated that they always examine the buccal mucosa. On the other hand, facial symmetry was never examined by 10% of the respondents.
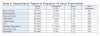
Factors that discouraged respondents from bringing suspicious lesions to the attention of the dentist were primarily related to the dentists’ behavior: for example, not referring a lesion for biopsy that the dental hygienist felt was suspicious (Table 6). Few respondents experienced patients becoming upset. The facilitating factors, ones that encouraged respondents to bring a suspicious lesion to the attention of a dentist, were the personal experiences of the respondents. More than half the respondents knew a patient with a history of oral cancer or had detected a cancerous lesion in the past.
Discussion
Detection of early-stage oral cancer is dependent upon the clinician’s knowledge of the visual appearance and tactile characteristics of the oral lesions and the features that differentiate malignant lesions from benign. Dental hygienists play a key role in the detection of precancerous and cancerous lesions.9 Do dental hygienists possess sufficient knowledge to detect early-stage oral cancer lesions? In our study we assessed this knowledge by asking survey respondents to view images of oral lesions and specify whether the lesions were suspicious or not. The respondents’ correct identification of the six images ranged from 40% to 97%. However, nearly 10% of the respondents did not respond to at least three of the six knowledge questions, and it is unclear if this was due to a lack of oral cancer knowledge.
Figure 2 was challenging for the respondents, with only 40% of the respondents correctly identifying the depicted lesion as erythroplakia, which has a high likelihood of malignant transformation. The other lesions may have been more obviously suspicious or benign. These data suggest that dental hygienists have the knowledge to detect obvious, or more advanced, lesions. However, due to the variety of benign lesions, such as bite trauma, or hyperkeratinization, less-obvious lesions may be difficult to distinguish as suspicious for oral cancer. Also, the difficulty in correctly identifying Figure 2 may have been due to the photographic image itself. It may have been ambiguous in its clinical presentation to some respondents.
Using images to test knowledge addresses the potential limitation present when knowledge is measured by self-report. Previous studies assessed other health care professionals’ oral cancer knowledge using various methods, usually multiple choice survey questions and self-report. For example, the survey reported by Applebaum et al included risks of oral cancer, signs symptoms, and characteristics of lesions.10 Questions on the impact of early detection on patient survival and the characteristics of lesions associated with smokeless tobacco were included in the knowledge score by LeHew et al.11 Because the surveys asked different questions, it is difficult to compare the results of the level of knowledge across the studies. Generally, survey respondents performed in the average range. In addition to assessing general oral cancer knowledge, investigators used a diagnostic ability scale to measure the correct identification of suspicious oral lesions.11 At least two previously published surveys addressed dental hygienists’ knowledge. Forrest et al found that 67% of the respondents correctly answered oral cancer questions relating to risk factors.6 Similarly, another study reported that the majority of respondents performed poorly on the knowledge portion of the survey (53% correct).9 The findings of these studies underline that there is no standardized, obvious visual sign of oral cancer, and that the variety in appearance of oral lesions makes early detection challenging.
Oral cancer lesions are usually detected in the Oral Cancer Examination (OCE); Cotter et al found a significant positive correlation between the identification of a suspicious lesion and the performance of oral cancer screening.12 Visual examination and lymph node palpation are reported to be valued components of the OCE, yet are not always performed. The majority of our respondents reported conducting some type of palpation, with the lymph nodes and tongue reported to be the least commonly examined by palpation. According to Kujan et al, many dental hygienists are seriously misinformed of what constitutes a thorough examination.2
In the study by LeHew and colleagues, dentists were surveyed for their thoroughness conducting the OCE, an assessment of both skill and frequency of procedures.11 These factors were also incorporated into the early detection practice scale, reported by Hassona.13 Based on this scale, participating medical and dental professionals reported average early detection practice, and only 18% reported that they routinely performed OCE in their practices.10 On the other hand, in a study of dental hygienists, Cotter et al reported that 46% of their respondents “always” performed OCE, 24% performed OCE at the initial appointment, and 47% at the recall appointment.10 These percentages are lower than the values that our respondents reported: 80% conducting OCE at every treatment appointment and 82% performing palpation. The current results are also higher than the Forrest et al study in which 25% of the respondents reported routinely palpating lymph nodes of their patients 100% of the time, while 51% reported not doing it at all.6 The inconsistency in the data may be explained by the lack of one standardized, explicit method for comprehensive OCE. Without a consistent method, integral steps of the OCE are being skipped. There is a striking need to establish a global consortium on oral cancer screening that will oversee research and provide recommendations for health professionals at regular intervals.2
Previous experience in detecting an oral cancer lesion or knowing a patient having a history of oral cancer were reported as facilitators, experiences that encouraged dental hygienists to bring a suspicious lesion to the attention of a dentist. Both of these factors may motivate a dental hygienist to continue to conduct thorough, comprehensive OCE. In fact, the current findings demonstrated that the respondents who conducted palpations were more likely to have known a person with a history of oral cancer and had previously detected a cancerous lesion. Making a personal connection enhances one’s understanding of the value of OCE in early-stage lesion detection.
The respondents of the current study reported these barriers or factors that influenced their decision not to bring a suspicious lesion to the attention of the dentist: personal experience in detecting a lesion that came back with a negative biopsy, the dentist not referring the dental hygienist’s recommendations, as well as the supervising dentists conducting OCE themselves. Twenty-nine percent of our respondents reported that their supervising dentists wanted to conduct the OCE themselves. Similarly, Bigelow et al. reported that the patient does not perceive urgency without the support from a dentist.9 While not asked in the current study as a survey question, lack of public and dentists’ awareness of dental hygienists’ competence with OCE appears to be a barrier to early diagnosis. Postponement of oral cancer diagnosis is often caused by delays from both patients and health professionals, partially due to poor awareness regarding oral cancer among the public and health care professionals alike.
The delay in detection and diagnosis of lesions is often attributed to the asymptomatic nature and the difficulty in differentiating premalignant and malignant lesions from benign conditions.6 For example, the majority of respondents incorrectly identified Figure 2 as not suspicious for oral cancer, indicating the difficulty in differentiation and suggesting the need for more extensive education of visually ambiguous malignant lesions. Education in identifying the visual appearance of early lesions may improve the early detection ability of professionals and increase the awareness needed to reduce delays in treatment.10 Also, the lack of a standardized method for OCE examination may contribute to the low detection rate. Professionals may be using their experience and clinical judgment to decide which structures to examine and palpate rather than an examination based on evidence. Steps in one standardized method are illustrated in the sequential photographs in the dental hygiene textbook, Darby and Walsh.14 Having knowledge of the necessary steps in performing a thorough exam6 and implementing one consistent method with clear and realistic steps may be a positive step toward increasing the detection of oral cancer lesions at an early stage.
The focus of this article was OCEs for all patients. Factors encouraging OCEs were based on the dental hygienists’ experiences with lesions and relationships, not on patients being high or low risk. It is unknown whether dental hygienists may not routinely do an OCE, but do at least conduct one when the patient is at high risk. In Table 2, 9% of the respondents selected “other” as frequency of OCE. Perhaps it can be speculated that the “other” was selected based on the respondents conducting OCEs only on high-risk patients. An ongoing study is assessing whether dental hygienists are more diligent in performing OCE when potentially treating high-risk patients. The danger of that philosophy is that early-stage lesions may be missed on patients without any risk factors, so OCE for all patients is recommended.
This study and many other studies of OCE conclude that there is a need for continued or mandatory continuing education on oral cancer knowledge and practices to make a difference in prevention and early detection of oral cancer in our patient population.4,6,9-13,15-18 Specifically, continuing education courses that include hands-on technique workshops were found to positively change attitudes and behaviors of OCE.4 These workshops should focus on palpation technique for specific areas to comprise a comprehensive OCE.9 The results from the current study suggest that continuing education courses, as well as entry-level education, should focus on the visual appearance of early-stage oral cancer lesions and one standardized method of OCE to ensure all valuable steps are performed thoroughly.
Limitations of this study include selection bias: respondents who completed the survey may have greater interest in the topic due to personal experience with oral cancer or oral cancer detection. Also, the low response rate (12%) yielded a response bias, which would affect the ability to generalize the results to all dental hygienists in California. The study population was limited to California dental hygienists whose email addresses were in the CDHA database. Although this database included both members and nonmembers, it is presumed that more members than nonmembers were in their database, as our data (Table 1) indicates that 79% of the respondents were CDHA members. That value would not be representative of the California dental hygienists. However, the remainder of the demographic characteristics does appear similar to the California dental hygiene population. Another limitation was that OCE practices were based on self-report, which often results in a social desirability bias.
Conclusion
This study indicates that dental hygienists have the knowledge to conduct OCE effectively. The majority of respondents reported conducting comprehensive OCE, although some omitted palpation of the lymph nodes and tongue. The lack of one clear, standardized method of OCE by health care professionals may be related to the low rate of early oral cancer detection. Establishing a standardized method for OCE could provide the knowledge health care professionals need to perform every integral step of a comprehensive OCE. Conventional oral examination still constitutes the gold standard screening method to identify potentially malignant oral lesions. The detection of early-stage oral cancer lesions by dental hygienists may be enhanced through more extensive education of visual appearances of lesions and the importance of palpation in a comprehensive OCE during both entry-level and continuing education programs.
Further research is indicated to improve the knowledge and practice of OCE, which may in turn increase the rate of early detection and decrease the life-altering and life-threatening experience of oral cancer in our patients.
ACKNOWLEDGMENTS
The authors express their appreciation to the California Dental Hygienists’ Association for its support of this study and distribution of the survey.
ABOUT THE AUTHORS
Dayna M. Hashimoto Barao, RDH, BS, MS, is a graduate of the Master of Science Program in Dental Hygiene at the University of California, San Francisco. Gwen Essex, RDH, MS, EdD, is a Clinical Professor in the Department of Preventive and Restorative Dental Sciences at the University of California, San Francisco and Co-Director of the Virtual Dental Home Clinics at the University of the Pacific Arthur A. Dugoni School of Dentistry. Ann A. Lazar, PhD, is an Assistant Professor and Dorothy J. Rowe, RDH, MS, PhD, is an Associate Professor Emeritus in the Department of Preventive and Restorative Dental Sciences at the University of California, San Francisco.
REFERENCES
1. Nadarajah V, Williams MD. Epidemiologic trends in head and neck cancer and aids in diagnosis. Oral Maxillofac Surg Clin North Am. 2014;26(2):123-141.
2. Kujan O, Sloan P. Dilemmas of oral cancer screening: an update. Asian Pac J Cancer Prev. 2013;14(5):3369-3373.
3. Paulis M. The influence of patient education by the dental hygienist: acceptance of the fluorescence oral cancer exam. J Dent Hyg. 2009;83(3):134-140.
4. Walsh MM, Rankin K, Silverman S. Influence of continuing education on dental hygienists’ knowledge and behavior related to oral cancer screening and tobacco cessation. J Dent Hyg. 2013;87(2):95-105.
5. Regezi JA, Sciubba JJ, Jordan RCK. Oral Pathology: Clinical Pathologic Correlations. St. Louis, MO: Saunders Elsevier; 2008:66-68.
6. Forrest J, Horowitz A, Shmuely Y. Dental hygienists’ knowledge, opinions, and practices related to oral pharyngeal cancer risk assessment. J Dent Hyg. 2001;75(4):271-281.
7. National Institute of Dental and Craniofacial Research. The oral cancer exam: NIH Publication. Bethesda, MD [Internet]. 2013 [cited 2014 Aug 27]. http://www.nidcr.nih.gov/OralHealth/Topics/OralCancer/TheOralCancerExam.htm. Accessed February 1, 2017.
8. Qualtrics software, Version 60526, of Qualtrics Research Suite. Copyright © 2015. Provo, UT, USA. http://www.qualtrics.com. Accessed February 1, 2017.
9. Bigelow C, Patton L, Strauss R, et al. North Carolina dental hygienists’ view on oral cancer control. J Dent Hyg. 2007;81(4):1-14.
10. Applebalm E, Ruhlen TN, Kronenberg FR, et al. Oral cancer knowledge, attitudes and practices: a survey of dentists and primary care physicians in Massachusetts. J Am Dent Assoc. 2009;140(4):461-467.
11. LeHew C, Epstein J, Kaste L, et al. Assessing oral cancer early detection: clarifying dentists’ practices. J Pub Health Dent. 2010;(70):93-100.
12. Cotter J, McCann A, Schneiderman E, et al. Factors affecting the performance of oral cancer screenings by Texas dental hygienists. J Dent Hyg. 2011;85(4):326-334.
13. Hassona Y, Scully C, Shahin A, et al. Factors influencing early detection of oral cancer by primary health-care professionals. J Cancer Educ. 2016;31(2):285-291.
14. Fehrenbach MJ. Extraoral and intraoral clinical assessment. In: Darby ML, Walsh MM, ed. Dental Hygiene: Theory and Practice. 4th ed. St. Louis, MO: Saunders/Elsevier Publishing; 2015:221-225,228-231.
15. van der Waal I, de Bree R, Brakenhoff R, et al. Early diagnosis in primary oral cancer: is it possible? Med Oral Patol Oral Cir Bucal. 2011;12(3):e300-e305.
16. Silverman S, Kerr A, Epstein J. Oral and pharyngeal cancer control and early detection. J Canc Educ. 2010;(25):279-281.
17. Maybury C, Horowitz A, Goodman H. Outcomes of oral cancer early detection and prevention statewide model in Maryland. J Public Health Dent. 2012;72 suppl 1:S34-S38.
18. Gajendra S, Cruz G, Kumar J. Oral cancer prevention and early detection: knowledge, practices, and opinions of oral health care providers in New York State. J Cancer Educ. 2006;21(3):157-162.
19. New York University Oral Cancer Center. Erythroplakia [Internet]. [Cited 2014 Nov 15]. http://www.nyuoralcancer.org/oral_cancer/oral_precancer.html. Accessed February 1, 2017.
20. Crutchfield Dermatology. Case of the month from Crutchfield dermatology [Internet]. [Cited 2014 November 15]. http://www.crutchfielddermatology.com/caseofthemonth/studies/2010/m_2010_006.asp. Accessed February 1, 2017.


![Fig 1. Lesion description: Leukoplakia. Most common precancerous lesion (89%: 618/695) (% = number of respondents who answered correctly/total respondents). [Ref. 20]](/media/thumbnail/13233)
![Fig 2. Lesion description: Erythroplakia. Highest potential for becoming malignant (40%: 272/684) (% = number of respondents who answered correctly/total respondents). [Ref. 19]](/media/thumbnail/13234)
![Fig 3. Lesion description: Leukoplakia. Precancer, smallest chance of developing into cancer (72%: 490/678) (% = number of respondents who answered correctly/total respondents). [Ref. 19]](/media/thumbnail/13235)
![Fig 4. Lesion description: Geographic Tongue. Benign migratory glossitis (89%: 600/676) (% = number of respondents who answered correctly/total respondents). [Ref. 20]](/media/thumbnail/13236)
![Fig 5. Lesion description: Erythroleukoplakia. Highest potential for becoming malignant (97%: 659/679) (% = number of respondents who answered correctly/total respondents). [Ref. 19]](/media/thumbnail/13237)
![Fig 6. Lesion description: Hypekeratinization. Benign (72%: 471/652) (% = number of respondents who answered correctly/total respondents). [Ref. 20]](/media/thumbnail/13238)