You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
INTRODUCTION
Intimate Partner Violence (IPV) has long been a part of human history, but it was not until the 1960s that there was recognition in the United States of its prevalence, impact, and outcomes.1,2 IPV is defined by the World Health Organization (WHO) as physical, sexual, or psychological harm by an intimate partner.3
A WHO systematic review examined data from 79 countries and found the global lifetime prevalence of IPV among women who had ever had an intimate partner was 30%.4 In the United States, the Centers for Disease Control and Prevention’s (CDC) National Intimate Partner and Sexual Violence Survey (NISVS) found approximately 31% of women experience a lifetime prevalence of physical violence by an intimate partner, and more than 20 people per minute become victims of IPV.5 Women are not the only victims of IPV: the lifetime occurrence for men is 27.5%.5 Based on the global and national prevalence, IPV is undeniably a serious and pervasive public health issue for both men and women.4,5
Health Effects of IPV
The health effects of IPV include sexually transmitted disease, HIV infection, miscarriage, low birthweight and premature babies, mental illness, substance use, nonfatal physical injuries, and fatal injuries (homicide).6 In terms of mental illness, depression, generalized anxiety disorders, and posttraumatic stress disorder (PTSD) are significant comorbidities that may affect 50% of women who experience IPV.4,7-10 Evidence is more limited about the association of IPV and eating disorders, but it appears 60% of women and 34% of men with eating disorders have a history of experiencing IPV.11
Nonfatal physical injuries associated with IPV include injury to the head, neck, and face.12,13 One of the most common IPV injuries is to the head and neck region and ranges from 50% to 77% with most injuries being in the upper third of the maxillofacial region.12,13 Soft-tissue injuries such as abrasions, lacerations, and bruising are seen in approximately 88% of reported cases related to IPV.13 Recognition of nonfatal injuries as an aid in identifying IPV victims is essential to prevent homelessness and possible fatal injury (homicide).13-15
Research has shown many women leave their homes due to violence, and therefore IPV becomes a contributing factor to the beginning of homelessness among women.14 Women who experienced IPV in the last year had almost four times the odds of housing instability as those who did not experience IPV.15 However, for women who stay in an abusive relationship, there is a risk of escalation of the violence resulting in fatal injury.12 Homicide by an intimate partner is a significant issue and impacts women six times more often than men, with a global prevalence of 38% for all women who have experienced IPV.4,6
IPV remains a major public health problem that has a significant social impact at the individual, family, and community level, and healthcare providers are central to screening and identifying individuals experiencing intimate partner violence.4,16 The American Medical Association and American Dental Association encourage healthcare providers to recognize, treat, and respond to IPV.17,18 Additionally, the American Dental Hygienists’ Association (ADHA) Standards for Clinical Dental Hygiene Practice include risk assessment for domestic violence.19
Healthcare Providers’ Knowledge, Attitudes, and Management of IPV
In many cases, healthcare providers do not recognize IPV.20-23 Routine assessment for IPV by medical and dental professionals remains low,20-23 yet the healthcare system is a necessary part of identification and management of IPV victims.16
OHCPs have a unique opportunity to identify and refer victims of IPV to support services because of the high prevalence of injury to the head, neck, and face.12,13,24 Despite the important role OHCPs play in helping IPV victims, 50% to 87% never screen for IPV.23,25,26 In the presence of head, neck, or facial injuries, 19% to 35% report not screening, and less than 50% refer patients to social services when IPV is suspected.23,25 The percentage of providers screening and referring for services is remarkably a low number considering the national and global IPV prevalence rate.4,5 However, 69% of IPV victims who saw an OHCP with signs of abuse reported that they would have liked the dental provider to ask about the injuries.27 It is time for dental providers to get past their embarrassment and discomfort about addressing IPV head on.
The barriers OHCPs face in screening IPV victims have been identified as lack of training, concern about offending patient, embarrassment about bringing up the topic, patient accompanied by partner or children, and concern about legal issues.23-26 Encouragingly, however, a recent survey found providers who received domestic violence education were more likely to have screened their patients (P < .0001) and more likely to take action when IPV was suspected (P = .0006).23
IPV research with OHCPs has consisted primarily of survey research with convenience sample sizes ranging from 359 to 536 (response rates 68.5% to 90%), and one study using a random sample (n = 321) with a 56% response rate.25 Mascarenhas et al conducted survey research that included dental hygienists.23 A major limitation to the survey research in OHCPs to date is use of instruments for which internal validity and reliability were not clearly described and no Cronbach α or internal consistency was reported.23,25,26
Dental hygienists, who typically spend the most one-on-one time with a patient, are in an ideal position to address this issue and ensure victims of IPV get the help and support they need. This study seeks to explore dental hygienists’ knowledge, attitudes, and readiness to manage IPV utilizing a survey instrument with good internal validity, reliability, and stable psychometric properties.28 The findings will assist in planning future education related to IPV.
METHODS AND MATERIALS
This cross-sectional, descriptive survey research was conducted using a web-based instrument with a convenience sample of dental hygienists. The study received approval from the university’s institutional review board (IRB) (protocol #IRB060914H).
Description of Setting
Participants were recruited at the ADHA annual session in June 2014. The principal investigator used a table in the exhibit hall for the purposes of conducting this survey. The ADHA conference was selected to recruit a national sample of participants.
Research Participants
Inclusion criteria were currently practicing dental hygienists and dentists. Exclusion criteria consisted of individuals attending the conference who were not dental hygienists or dentists. Participants recruited were provided with a postcard with the URL for the web-based survey. All participants gave implied consent by completing the online survey.
Instrument
Permission was obtained, and the Physician Readiness to Manage Intimate Partner Violence (PREMIS) tool was modified to meet the purpose of this study. Modifications were limited to the respondent profiles to make them more applicable to dental providers. The survey questions consisted of 37 questions grouped into five major sections: (1) respondent profiles (11 items); (2) background (education or training) in IPV, perceived knowledge, and perceived preparation to manage IPV (four items with multiple parts); (3) actual knowledge of IPV (eight items); (4) IPV opinions concerning attitudes and beliefs (one item with multiple parts); and (5) practice issues dealing with behaviors and office practice policies (13 items).
Construct Validity. The original PREMIS instrument was developed in conjunction with expert reviewers.28 Construct validity is based on the ability of a tool to measure what it claims to measure. The construct validity for PREMIS was based on the ability to measure attitudes, knowledge, and attitudes that contribute to healthcare providers responding effectively to victims of IPV. A final measure of construct validity for PREMIS was the extent to which knowledge, attitudes, and training predicted self-reported behaviors.28
Reliability. The PREMIS tool demonstrated good internal consistency among the items with a Cronbach’s α > 0.963.28 The tool has good stability in psychometric properties and a good correlation with the measured office practices of IPV.28 In addition, the correlation among the survey items relate to the OHCPs’ opinions about the adequacy of previous training, attitudes, and knowledge of IPV.28 The survey instrument also helps determine awareness of IPV.28
Statistical Analysis
All data obtained was entered into Microsoft Excel spreadsheets and imported into STATA 11.2 software for statistical/data analysis. Descriptive statistics were used for the respondent profiles and survey questions.
RESULTS
One hundred thirty-three participants met the study inclusion criteria and were given and submitted the survey. To account for large amounts of unanswered questions by participants, responses for participants who left one or more of the five major sections in the survey instrument entirely unanswered were excluded from the analysis. Following this exclusion for missing data, a total of 117 participants were included in the analysis. The participants were primarily 25 to 64 years of age, and predominately female (79%) with 20% male and 1% transgender (Table 1). The most common specialties in the primary field of dental practice included general dentistry (69%), periodontal practice (2%), public health (14%), pediatric (3%), and orthodontics (3%). The respondents had a mean of 19 years in practice.
Previous Intimate Partner Violence Training
Of those participants who provided information on their previous IPV training, 58% attended some form of lecture or talk about IPV training, 14.5% attended a skill-based training or workshop, 14.5% attended other classroom training, 5% attended school-clinical setting training, and 8% received no previous training. The mean number of training hours was ≤ 6.66 hours (Table 1).
Perceived Preparation for Managing Intimate Partner Violence
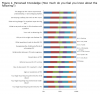
In the questions related to Perceived Preparation, 50% to 63% of participants felt slightly, minimally, or not prepared except in relation to documenting IPV history or physical examination findings in the patient chart (45%) (Figure 1). The items with the highest percentages of participants feeling slightly, minimally, or not prepared were creating a safety plan and conducting a safety assessment (62.4%). Fifty-nine percent felt slightly, minimally, or not prepared to respond to a disclosure of abuse. For the second question related to Perceived Knowledge 44% to 62% reported knowing a little, very little, or nothing about each of the items with the exception of legal requirements for reporting child abuse (39%) (Figure 2). Approximately 14% to 27% of respondents reported knowing quite a bit or very much about the items. The items participants felt most knowledgeable about were the legal reporting requirements for IPV (20.5%), child (26.5%), and elder abuse (24.7%); how to document IPV in a patient’s chart (21.4%); determining danger for a patient experiencing IPV (19.7%); why a victim might not disclose IPV (20.5%); and signs and symptoms of IPV (21.4%).
Actual Knowledge of Intimate Partner Violence
The Actual Knowledge was scored based on correct responses. Fifty percent to 83% of respondents answered correctly for a majority of items (Table 2). The items the respondents answered correctly least often included persons who have experienced domestic violence are able to make appropriate choices about how to handle their situation (12%) and the most appropriate way to ask about IPV: are you a victim of intimate partner violence? (20%).
Opinions
The opinion scale represented the OHCPs’ attitudes and beliefs about IPV.
Understanding Victims Experiencing Abuse. Results showed participants had a fairly good understanding of IPV victims with the exception of relationship of drug and alcohol abuse to IPV (30.8% to 32.5%) (Figure 3).
Self-Preparation. Fifty percent or more of respondents somewhat disagreed, disagreed, or strongly disagreed that healthcare providers didn’t have the skills and knowledge to address IPV with all items except the last one (Figure 4). More than 45% somewhat agreed, agreed, or strongly agreed with the statement: I do not have sufficient training to assist individuals in addressing situations of IPV.
Self-Efficacy. Respondents were evenly divided in their response to the items related to self-efficacy (Figure 5). The items that respondents more strongly disagreed, disagreed, or somewhat disagreed with included the following: I am too busy to participate on a multidisciplinary team that manages IPV cases (70.9%); I ask all new patients about abuse in their relationships (76%); I am capable of identifying IPV without asking my patient about it (57.3%); and I can recognize victims of IPV by the way they behave (62.4%).
Workplace Issues. Approximately 50% of respondents strongly disagreed, disagreed, or somewhat disagreed with all but two items related to workplace issues (Figure 6). The responses were evenly divided between agreed and disagreed with the statement: my practice setting allows me adequate time to respond to victims of IPV. Fifty percent disagreed with the item: I can make appropriate referrals to services within the community for IPV victims, and another 64% disagreed with the statement: I have contacted services within the community to establish referrals for IPV victims.
Practice Issues
Clinical Management. A majority of respondents (89%) reported not identifying IPV in the last 6 months, but only 7% screen all new patients, and 9% screen patients when abuse indictors on history or exam are noted (Table 3). When IPV had been identified, 14% reported referring the patient to a local domestic violence/IPV hotline, and 21% provided information to the patient.
General Practice Resources. Nineteen percent of practices reported having a protocol for dealing with adult IPV, 46% reported no protocol, and another 18% were unsure or felt it is not applicable to their patient population. See Table 4 for the results of resources available for victims of IPV in practice settings.
DISCUSSION
In this study, 92% of participants reported attending some form of IPV education or training as compared to Love et al, who found over 70% of dentists had not received any education related to domestic violence.25 In this study, the average IPV education or training was just over 6.5 hours for participants, which is twice as much as that reported by Ramsey et al among primary healthcare providers in the United Kingdom.29 Other literature has reported on whether healthcare providers have had training, but most did not gather information on the number of hours OHCPs had received regarding IPV education or training.23,25,26,30
IPV Knowledge. In this study, 50% to 83% of respondents had correct responses, and the survey identified areas for improvement to help identify individuals who are at risk or victims of IPV. This is lower than seen in studies with other healthcare providers, which is of concern given that 60% to 77% of IPV injuries are to the head and neck area and OHCPs acknowledge a role in reducing the prevalence of IPV.12,23,25,26,31
Preparation. The areas where OHCPs feel most prepared to manage IPV was documenting it in patient charts and requirements for legal reporting, which is consistent with research found in other healthcare professions.23,25,30
Opinion, Attitudes, and Beliefs About IPV. Lack of training was reported as a barrier by 45% of respondents in this study, which is lower than seen in other studies. Love et al reported 61% of dentists would like more IPV training, and similarly Mascarenhas et al reported 82%, which may be related to the high percentage of respondents in this study who had previous IPV training or education.23,25 Workplace issues noted in this study were consistent with other research and included: lack of time, lack of training to screen for or identify IPV, and ability to make appropriate referral to community services for IPV.23,25,26,29,30
Clinical Management. The literature on screening for IPV has shown 50% to 87% never screen for IPV, which is consistent with the findings in this study where 93% do not screen new patients.23,25,26,29 In the presence of head, neck, or facial injuries, 19% to 40% report not screening in the literature, while this study found only 9% screened in the presence of abuse indicators.23,25,26,30 IPV research has found less than 50% of healthcare providers and OHCPs refer patients to social services when IPV is suspected, and this study found 28% refer to IPV hotlines, battered women’s shelters, and other local and national domestic violence resources.23,25,30 The percentage of providers screening and referring for services is a low number considering the national prevalence of IPV.4,5 However, 69% of victims of IPV reported that they would have liked the dental provider to ask about the visible injuries.27
Implications for Research and Practice
This study highlights the areas of inadequate OHCP knowledge and preparation for responding to the needs of women and men experiencing IPV. In particular, enhancing OHCPs knowledge of IPV along with protocols for screening and referral to domestic violence services could make a significant impact on this major public health issue.23 Preliminary research was done by Hsieh et al in 2006 using an interactive multimedia tutorial on domestic violence with a focus on Asking, Validating, Documenting, and Referring (AVDR), but little follow-up or implementation of this model has occurred in the dental professions.26,31
Strengths and Limitations
The strengths of this cross-sectional survey included the use of a validated questionnaire to explore the knowledge, attitudes, and practices of OHCPs in relationship to intimate partner violence with a national sample of OHCPs. However, a limitation of this study is the lack of correlation with actual IPV clinical practices since self-reporting may introduce bias. Another limitation was the use of a convenience sample, which limits generalizability even though the survey did include a national sample of OHCPs. A further limitation of the study was the length of the modified PREMIS tool that specified it would take about 15 minutes to complete; however, respondents reported that it actually took 30 minutes to complete the survey. This may have caused the missing or incomplete answering of items found within the survey.
CONCLUSION
This study explored OHCPs’ attitudes and knowledge of IPV, and provided insight into IPV screening practices and management in dental care settings. A much higher percentage of participants in this study reported some education or training in IPV than in previous IPV literature; however, nearly half still felt they were inadequately prepared to assist victims of IPV.25,30 Knowledge about identifying victims of IPV needs improvement as well as a defined office screening protocol for IPV. The other major barrier that must be addressed includes resource and referral information to provide to individuals who are identified as victims of IPV. OHCPs who do not let embarrassment or discomfort be a barrier in professionally addressing the issue have the opportunity to play a pivotal role in managing the “silent epidemic” of IPV.
ACKNOWLEDGMENTS
The authors thank Lynn M. Short, PhD, MPH, for giving permission to modify the PREMIS tool.
ABOUT THE AUTHORS
Chris Marie Harris, RDH, MS, is a practicing Dental Hygienist and graduate student at Massachusetts College of Pharmacy and Health Sciences (MCPHS) University, Boston Massachusetts. Linda D. Boyd, RDH, RD, EdD, is Dean of Forsyth School of Dental Hygiene at MCPHS University, Boston, Massachusetts. Lori Rainchuso, RDH, DHSc, is an Associate Professor at Forsyth School of Dental Hygiene at MCPHS University, Boston, Massachusetts. Andrew Rothman, MS, EIT is adjunct faculty at Forsyth School of Dental Hygiene at MCPHS University, Boston, Massachusetts.
REFERENCES
1. Bradley D. The beginning of domestic violence—domestic violence prevention month: part one of four. Dyess Air Force Base [Internet]. 2007 Oct 3 [updated 2007 October 3]. https://www.dyess.af.mil/news/story.asp?id=123070512.
2. Centers for Disease Control and Prevention. Intimate partner violence: definitions 2013. [Internet]. www.cdc.gov/ViolencePrevention/intimatepartnerviolence/defintions.
3. World Health Organization, Pan American Health Organization. Intimate partner violence: understanding and addressing violence against women 2012. Geneva, Switzerland: WHO; 2012. [Cited 2015 Oct 01]. http://www.paho.org/hg/inde.php?option=com_content & view=article & ed=865%3.
4. World Health Organization. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and nonpartner sexual violence. Geneva, Switzerland: WHO; 2013. [Cited 2015 Oct 01]. http://apps.who.int/iris/bitstream/10665/85239/1/9789241564625_eng.pdf.
5. Breiding MJ, Smith SG, Basile KC, et al. Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization—national intimate partner and sexual violence survey, United States, 2011. MMWR Surveill Summ. 2014 Sep 5;63(8):1-18.
6. Stöckl H, Devries K, Rotstein A, et al. The global prevalence of intimate partner homicide: a systematic review. Lancet. 2013;382(9895):859-865.
7. Mason R, O’Rinn SE. Co-occurring intimate partner violence, mental health, and substance use problems: a scoping review. Global Health Action. 2014;7:10.3402/gha.v7.24815.
8. Du Mont J, Forte T. Intimate partner violence among women with mental health-related activity limitations: a Canadian population based study. BMC Public Health. 2014;14:51. doi:10.1186/1471-2458-14-51.
9. Salom CL, Williams GM, Najman JM, Alati R.Substance use and mental health disorders are linked to different forms of intimate partner violence victimisation. Drug Alcohol Depend. 2015;151:121-127.
10. Devries KM, Mak JY, Bacchus LJ, et al. Intimate partner violence and incident depressive symptoms and suicide attempts: a systematic review of longitudinal studies. PLOS Med. 2013;10(5):e1001439.
11. Bundock L, Howard LM, Trevillion K, et al. Prevalence and risk of experiences of intimate partner violence among people with eating disorders: a systematic review. J Psychiatr Res. 2013;47(9):1134-1142.
12. Wong JY-H, Choi AW-M, Fong DY-T, et al. Patterns, aetiology and risk factors of intimate partner violence-related injuries to head, neck and face in Chinese women. BMC Women’s Health. 2014;14:6.
13. Saddki N, Suhaimi AA, Daud R. Maxillofacial injuries associated with intimate partner violence in women. BMC Public Health. 2010;10:268.
14. Bassuk EL, Weinreb LF, Buckner JC, et al. The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA. 1996;276(8):640-646.
15. Pavao J, Alvarez J, Baumrind N, et al. Intimate partner violence and housing instability. Am J Prev Med. 2007;32(2):143-146.
16. O’Doherty L, Hegarty K, Ramsay J, et al. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2015 Jul 22;7:CD007007.
17. American Medical Association. AMA Code of Ethics: Opinion 2.02-Physicians’ obligation in preventing, identifying, and treating violence and abuse. AMA: Chicago, IL; 2008. [Cited 2015 Oct 02]. http://www.ama-assn.org/ama/pub/physicianresources/medical-ethics/code-medical-ethics/opinion202.page.
18. American Dental Association. ADA principles of ethics and code of professional conduct: abuse and neglect. ADA: Chicago, IL; 2012. [Cited 2015 Oct 02]. http://www.ada.org/en/about-the-ada/principles-of-ethics-codeof-professional-conduct/.
19. American Dental Hygienists’ Association. Standards for clinical dental hygiene practice. ADHA: Chicago, IL; Updated 2014. [Cited 2015 Oct 02]. https://www.adha.org/resourcesdocs/7261_Standards_Clinical_Practice.pdf.
20. Sundborg E, Törnkvist L, Saleh-Stattin N, et al. To ask, or not to ask: the hesitation process described by district nurses encountering women exposed to intimate partner violence. J Clin Nurs. 2015 Sep 30. doi:10.1111/jocn.12992.
21. Nicolaidis C, Curry M, Gerrity M. Health care workers’ expectations and empathy toward patients in abusive relationships. J Am Board Fam Med. 2005;18(3):159-165.
22. Beynon CE, Gutmanis IA, Tutty LM, et al. Why physicians and nurses ask (or don’t) about partner violence: a qualitative analysis. BMC Public Health. 2012;12:473.
23. Mascarenhas AK, Deshmukh A, Scott T. New England, USA dental professionals’ attitudes and behaviours regarding domestic violence. Br Dent J. 2009;206(3):E5; discussion 152-153.
24. Coulthard P, Yong SL, Adamson L, et al. Domestic violence screening and intervention programmes for adults with dental or facial injury. Cochrane Database Syst Rev. 2010 Dec 8;(12):CD004486.
25. Love C, Gerbert B, Caspers N, et al. Dentists’ attitudes and behaviors regarding domestic violence. The need for an effective response. J Am Dent Assoc. 2001;132(1):85-93.
26. Mythri H, Kashinath KR, Raju AS, et al. Enhancing the dental professional’s responsiveness towards domestic violence: a cross-sectional study. J Clin Diag Res. 2015;9(6):ZC51-ZC53.
27. Nelms AP, Gutmann ME, Solomon ES, et al. What victims of domestic violence need from the dental profession. J Dent Educ. 2009;73(4):490-498.
28. Short LM, Alpert E, Harris JM, Surprenant ZJ. A tool for measuring physician readiness to manage intimate partner violence. Am J Prev Med. 2006;30(2):173-180.
29. Ramsay J, Rutterford C, Gregory A, et al. Domestic violence: knowledge, attitudes, and clinical practice of selected UK primary healthcare clinicians. Br J Gen Pract. 2012; DOI: 10.3399/bjgp12X654623.
30. Roelens K, Verstraelen H, Van Egmond K, Temmerman M. A knowledge, attitudes, and practice survey among obstetrician-gynaecologists on intimate partner violence in Flanders, Belgium. BMC Public Health. 2006;6:238.
31. Hsieh NK, Herzig K, Gansky SA, et al. Changing dentists’ knowledge, attitudes and behavior regarding domestic violence through an interactive multimedia tutorial. J Am Dent Assoc. 2006;137(5):596-603.