You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dental caries is an infectious, transmissible, bacterial disease affecting children and adults of all races, ethnicities, and socio-economic levels.1,2 It is a major public health problem both within the United States and around the world, and has devastating effects including pain, infection, nutritional insufficiencies, learning and speech problems, and even death.3 While disturbances in the balance between bacteria and host are the factors traditionally responsible for caries development, factors such as family, economic, and social conditions also have a substantial impact on the development of the disease.4,5 Current research has demonstrated that multiple risk factors are responsible for the occurrence and prevalence of caries, including frequent sugar consumption, improper oral hygiene, high levels of oral bacteria, cariogenic feeding practices, socio-economic status, minority status, and inconsistent oral healthcare access.3,4,6-10
Early childhood caries (ECC) is defined as caries in children younger than 72 months of age, and disproportionately affects low-income families.4,11-14 Populations with low-income levels and high utilization of Medicaid insurance have been shown to have an increased risk of ECC development.15 Preventive dental care and education is critical for parents of high-risk children to identify current dental health concerns and prevent future problems.12 However, within the United States, only 40% of low-income children have received preventive dental care compared to 54% of higher income children.16 Many barriers affect access to dental services for disadvantaged children including a lack of providers and cost of services, as well as culture and oral health beliefs.12,17 Consequently, the prevention of ECC in high risk, Medicaid-enrolled children remains a challenge for healthcare personnel in the fields of dentistry and medicine.5,8
An anticipatory approach emphasizing oral health promotion is likely to have the greatest positive effect on children’s oral health.5 Preventive care visits can be utilized to educate parents and caregivers on proper oral hygiene techniques as well as known behavioral and social risk factors for ECC development.6,9 Nutritional education should be provided during preventive care visits in order to ensure cariogenic feeding practices are avoided and proper dietary guidelines are being followed for optimal oral and overall heath. The goal of providing anticipatory guidance for the caregiver is to modify or eliminate practices and behaviors known to increase caries disease risk for the child.4,8
The American Academy of Pediatric Dentistry (AAPD) policy statement indicates the following should be provided by a dental home:18
• Comprehensive assessment
• Individualized preventive care based on caries and periodontal risk
• Anticipatory guidance related to growth and development including care of the child’s soft and hard tissues
• Education of parents/caregivers on management of acute dental trauma
• Nutrition assessment and counseling
• Comprehensive care including preventive services according to AAPD guidelines
• Referral as needed to specialists
There is a lack of evidence evaluating the impact of an established dental home (as defined by the AAPD as “an ongoing relationship between the dentist and the patient, including all aspects of oral healthcare delivered in a comprehensive, continuously accessible, coordinated, and family-centered way”) on ECC prevalence and risk, particularly in high-risk populations.19 The purpose of this cross-sectional study was to explore:
1. The association between the establishment of a dental home and ECC prevalence in Medicaid-enrolled preschool children.
2. Feeding practices associated with an increased prevalence of ECC in Medicaid-enrolled preschool children with an established dental home.
Methods and Materials
An observational, cross-sectional study using a survey instrument was conducted at a dental center providing care to primarily children and adolescents in Manchester, NH. Data from the 2010 Census estimates 13.8% of Manchester residents have incomes at or below the Federal Poverty Level (FPL).20 The New Hampshire Department of Health and Human Services (NHDHHS) indicates that of the 135,012 New Hampshire residents enrolled within the Medicaid program in 2010, 24,080 reside in Manchester, accounting for 12% of its total population.20 Overall, from 2009 to 2010, there was a 5% increase in Medicaid enrollments throughout the state and the percentage of children enrolled reached 60.2% of all enrollees.21
The dental center used for the present study adheres to the policy of the AAPD regarding the expectations of care within an established dental home. Patients receive a prophylaxis and examination on a bi-yearly basis during 45-minute appointment times. The four general dentists and five dental hygienists provide all aspects of this policy including:22
• Individualized preventive dental health plans, specific to a child’s caries risk assessment
• Anticipatory guidance about growth and development
• Education regarding proper oral hygiene techniques
• Individualized nutritional counseling
This study population consisted of a convenience sample of 132 Medicaid-enrolled male and female children between 2 and 5 years of age attending their scheduled preventive appointment at the dental center during the study period. The established dental home group (n = 101) inclusion criteria were those children who had preventive care and anticipatory guidance as outlined by the AAPD policy on a dental home within the last year at the dental center.19 The no dental home group (n = 31) inclusion criteria for children were those who had no history of preventive or restorative dental visits. Parental or guardian informed consent was obtained for the child’s participation. The institutional review board at the affiliated university approved and oversaw the administration of the study.
Sampling Procedure and Data Collection
A survey instrument was adapted from the demographic, diet, and nutritional sections of the National Health and Nutritional Examination Survey (NHANES) III.22 The instrument consisted of questions regarding the child’s demographics (two items), feeding practices (14 items), dental history (three items), and current parental knowledge of caries risk factors (one item). The survey instrument was completed by the parent or guardian during the child’s preventive appointment.
The validity of the questionnaire was assessed using a content validity index (CVI). Six experts in the fields of dentistry and nutrition evaluated the survey and determined the questions were an adequate representation of the study’s research questions. Each expert employed a 4-point scale to calculate a value on the individual content (I-CVI) as well as the overall content (S-CVI). The content validity was deemed excellent if the I-CVI was 0.78 or higher for three or more experts and the S-CVI was 0.90 or higher.23 For the study questionnaire, four or more experts agreed with each item giving an overall I-CVI of 0.97. The S-CVI for the questionnaire was 0.93 indicating an overall excellent content validity.
A pilot survey (n = 10) was conducted to pre-assess parent or caregiver survey completion time and ease of comprehension. Additionally, the pilot screenings were used to assess and implement standard practices for the dental hygienists providing the survey. The results of the pilot assessments were not included in the final study results.
The child’s current dental health status was coded using an examination meeting the guidelines from the dental center and forms adapted from the World Health Organization’s Basic Model of Oral Health Surveys.24 Documented information included active caries, treated caries, and oral hygiene status. All of the clinicians were calibrated prior to the beginning of the study to ensure accurate recording of data. Each clinician performed the data retrieval process on at least five patients and the results were compared and discussed, and methods modified until 100% agreement was attained to ensure consistent documentation. This training practice was modified from the CDC’s Dental Examiners Procedures Manual developed for the NHANES.22
During the prophylaxis appointment, the dental center’s odontogram was used to document any existing restorations and/or missing teeth. Throughout the clinical examination performed by the dentist, the areas of active caries were also recorded on the odontogram form. The data was then transferred from the odontogram to the decayed, missing, and filled teeth (DMFT) index at the end of the questionnaire. The DMFT index for primary teeth was employed due to the age of the study participants. The clinical assessment form was also used to document the child’s oral hygiene, indicating the presence of dental biofilm and/or gingivitis. The prophylaxis and examination was conducted using either the knee-to-knee technique with the parent or guardian or with the child in the dental chair, dependent upon patient behavior. A mouth mirror was used to identify dental biofilm, gingivitis, restored caries, and missing teeth. The dental examination was conducted using an explorer, mouth mirror, and radiographs, if possible, to diagnose active carious lesions.
The general dentists at the dental center employed visual, tactile (using an explorer), and radiographic (using bitewing and/or occlusal radiographs) means for caries detection. These techniques of caries detection are dependent upon patient behavior and, consequently, not all means were used for every patient. Surface demineralization or a white-spot lesion was not documented as a carious lesion but rather used as an educational tool for parents in terms of improving or modifying their child’s nutrition or oral hygiene. After the prophylaxis and examination, the child received a fluoride varnish application, oral hygiene instructions, and nutritional counseling.
Data Analysis
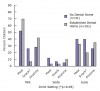
To investigate the association between ECC prevalence in Medicaid-enrolled preschool children and the establishment of a dental home, general and demographic characteristics data were compared between the two groups (established dental home vs. no dental home) (Table 1). Categorical and binary variables were compared using global chi-square tests of independence, with continuous variables compared using nonparametric Mann-Whitney U tests.25,26 Feeding practices were compared between the two groups using chi-square tests of independence (Figure 1 through Figure 3). Note that adjustments for multiple comparisons were not performed due to a priori specification of comparisons.27
As an indicator of the presence of caries, DMFT index was dichotomized into DMFT > 0 and DMFT = 0. Univariate logistic regression associating dichotomized DMFT index with establishment of a dental home was performed, with “Multivariate Model I” including age and gender as covariates using multivariate logistic regression (Table 2).28 For “Multivariate Model II,” a model selection procedure was performed among candidate covariates’ age; sex; child breastfed; age bottle usage ended; usage of a sippy-cup; daily servings of milk, soda, and juice; partaking in snacking; age of first dental appointment; presence of biofilm; and presence of gingivitis. To assess and control for potential confounding as well as identify strong predictors of outcome, inclusion in the “Multivariate Model II” required meeting one or more of the following criteria: whether inclusion or exclusion of the variable from the univariate model changed the adjusted odds ratio for established dental home by ≥10%, or inclusion in a stepwise logistic regression model met the pre-specified alpha threshold (alpha = 0.05).29,30 Variables that changed the adjusted odds ratio by ≥10% were forced into the stepwise model. The final model included age, gender, daily serving of juice, age of first dental appointment, presence of biofilm, and presence of gingivitis (Table 2). To investigate the associations of feeding practices on DMFT index in the established dental home group, over-dispersion corrected univariate Poisson regressions via a scaling factor were performed (Table III).31 Statistical analyses were performed in STATA® statistics/data analysis software version 11.2.
Results
As per the descriptive univariate analyses comparing the established dental home and no dental home groups, the mean age for the two groups were similar at 48.7 months and 47.7 months, respectively (Table 1). Additionally, both groups had comparable distributions by gender, with 53.5% male in the established dental home group and 54.8% male in the no dental home group. Questions regarding breastfeeding and bottle usage revealed multiplicative univariate differences. A larger percentage of children in the no dental home group were breastfed on-demand (45.2%) and were still using a bottle (12.9%) compared to the established dental home group (28.7% and 3%, respectively). In regards to age at first dental appointment, 66.3% of the established dental home group visited the dentist for the first time between 1 and 2 years of age, whereas the greatest percentage of the no dental home group had their first visit between 4 and 5 years of age, 45.2% (P < .05). A greater percentage of the no dental home group presented with dental biofilm (96.8%) and gingivitis (71%) compared to the established dental home group (79.2% and 44.6%, respectively) (P < .05). Mean DMFT index scores differed significantly, with index 5.19 for the no dental home group and 1.8 for the established dental home group (P < .05). A total of 57.4% of children with an established dental home had DMFT scores of zero, compared with 22.6% in the no dental home group (P < .05).
Comparing feeding practices in the two groups revealed statistically significant multiplicative differences. Children with no dental home were more likely to drink milk and juice during snack time (P < .05) (Figure 1), to have more than six servings of sodas per day and drink more than four servings of juice per day (P < .05) (Figure 2). Figure 3 illustrates those in the no dental home group more likely to consume three servings of sticky snacks, including dried fruit or gummy fruit snacks, per day (P < .05).
Univariate logistic regression associating dichotomized DMFT index (DMFT >0 vs DMFT = 0) with establishment of a dental home (yes vs no) produced a statistically significant odds ratio (OR) of 0.22 with 95% confidence interval (CI) 0.08 to 0.55 (Table 2), showing a very strongly associated protective effect of establishment of a dental home on presentation of caries. Adjustment for age and gender via multivariate logistic regression further lowered the OR for establishment of a dental home to 0.15 (95% CI: 0.05 to 0.42) shown as “Multivariate Model I” in Table 2. As per the model selection procedure to identify strong predictors of outcome and adjust for confounding, the OR for establishment of a dental home was further lowered to 0.10 (95% CI: 0.02 to 0.40) after adjusting for age, gender, daily serving of juice, age of first dental appointment, presence of biofilm, and presence of gingivitis, shown as “Multivariate Model II” in Table II.
Of the over-dispersion corrected univariate Poisson regressions performed to assess the associations of feeding practices on DMFT index in the established dental home group, several practices were found to be strongly statistically associated with a multiplicative increase in DMFT index. Such feeding practices include: drinking juice frequently during the day (eβ = 1.19, 95% CI: 1.04 to 1.36), eating candy frequently during the day (eβ = 1.21, 95% CI: 1.01 to 1.45) consuming milk at mealtime (eβ = 1.80, 95% CI: 1.25 to 2.59), having juice during snack time (eβ = 1.78, 95% CI: 1.33 to 2.38) and drinking from a glass (eβ = 1.82, 95% CI: 1.29 to 2.58), as shown in Table 3. Drinking from a sippy cup also showed a univariate multiplicative decrease in DMFT index (eβ = 0.44, 95% CI: 0.24 to 0.80).
Discussion
Oral health is essential to general health and well-being.32 However, significant oral health disparities remain among certain socioeconomic groups within the US population.3,32 The disparities in access to both medical and dental care have significant and lifelong effects on the oral and overall health of children and adolescents.32 Since family, economic, and social conditions have a substantial impact on the development of ECC, an approach emphasizing health-promoting behaviors at the individual level is likely to have the greatest positive effect on children’s oral health.4,5 Consequently, the establishment of a dental home, especially for high-risk, low-income children is critical for educating parents and caregivers on the known risk factors associated with ECC development, including frequent sugar consumption, inadequate oral hygiene, high levels of oral bacteria, and cariogenic feeding practices.3,4,6-10 The care provided through a dental home may also decrease the prevalence of recurrent caries. The current research has indicated over 50% of low-income children exhibit recurrent caries post restorative treatment.33 However, among the patients in the established dental home group with DMFT scores of 1 or higher, only 29.7% presented with new carious lesions.
This study explored the association of an established dental home on ECC prevalence and cariogenic feeding practices in high-risk populations. While it revealed significant consistencies with the current literature about specific feeding practices and ECC prevalence in high-risk populations,3,4,7 it also investigated the association of dental home establishment and oral hygiene, caries status, and cariogenic feeding behaviors. In accordance with the literature, the results demonstrated significant relationships between higher DMFT scores and a frequent consumption of sticky snacks (candy) and sugary drinks (juice), as well as prolonged drinking sessions.3,4,6,7,10 Children with an established dental home had a lower prevalence of caries, and lower rates of biofilm and gingivitis. Logistic regression analysis showed a very strong protective effect for establishment of a dental home on caries status. The above findings add further evidence for the effectiveness of oral hygiene education and anticipatory guidance provided at preventive care visits on prevention of adverse oral health outcomes.
The current study also revealed significant differences in specific feeding behaviors between the two groups, with the no dental home group exhibiting more cariogenic practices than the established dental home group. This finding suggests the anticipatory guidance and nutritional counseling implemented at the children’s’ routine preventive dental appointments may play an important role in feeding practices adopted by parents, particularly in high-risk populations.
However, there was one finding regarding a dietary practice that did not coincide with what has been demonstrated in the literature. The regression analysis showed consuming milk at mealtime was associated with a multiplicative increase in DMFT score (eβ = 1.82, 95% CI: 1.29 to 2.58). One possible explanation could be that the consumption of milk at mealtime had an added amount of sugar, such as flavored milk, soy, rice, or almond milk. This is an area that would benefit from further research and investigation.
It is important to address the limitations in this study. Like any observational study, structural biases including residual confounding, selection bias, and data misclassification and misspecification are a possibility. The present study may lack statistical power to identify important statistical associations due to the study’s limited sample size. The study cohort was created using a convenience sample, calling into question the generalizability of the study results to broader populations. The present study was also a cross-sectional study, greatly limiting the ability to “tease-out” the direction of causality and limiting the analysis to associational measures. Additionally, the definition of a dental home within the study population was operationalized as having made at least one previous visit to the dental center. The goals of the dental home may not be achievable with one visit to the dental office.
The results suggest the establishment of a dental home, especially among high-risk, low-income populations, is strongly associated with a decreased prevalence of ECC and reduced cariogenic feeding practices. Consequently, the collaboration between dentistry and medicine is a significant aspect in the prevention and management of ECC and the education of its risk factors. Therefore, in accordance with recommendations from the CDC, the AAPD, and the American Academy of Pediatrics (AAP), all children should establish a dental home no later than 1 year of age.34-37 The AAP also advises that a child’s first caries risk assessment be completed by their health professional at 6 months of age, especially if they are considered high risk for dental caries.35,36 Pediatricians and physicians must also be aware of the clinical manifestations of dental disease and be prepared to educate families on its risk factors and consequences.4 It is also beneficial for pediatric healthcare professionals to understand the etiological caries process, including enamel demineralization, and have the ability to identify the behavioral and dietary habits putting a child at higher risk of dental disease.4
Conclusion
The findings of this study will not only aid in developing a stronger partnership between medicine and dentistry in promoting oral health, but also in the implementation of new policies regarding protocols of preventive dental care. General and pediatric dentists can use the current research to design policies specific for their pediatric population to strengthen their preventive program’s nutritional counseling, parental anticipatory guidance, and oral hygiene instruction.
About the Authors
Erin A. Kierce, RDH, MS, MPH, is Manager of Clinical Hygiene Practice and Professional Development at New England Family Dentistry in Marlborough, Massachusetts. Linda D. Boyd, RDH, RD, EdD, is Dean and Professor at Forsyth School of Dental Hygiene at MCPHS University. Lori Rainchuso, RDH, MS, is an associate professor at Forsyth School of Dental Hygiene at MCPHS University. Carole A. Palmer, EdD, RD, LDN, is a professor at Tufts University, School of Dental Medicine and Friedman School of Nutrition Science and Policy. Andrews Rothman, MS, EIT, is a doctoral candidate at Harvard School of Public Health and adjunct faculty in Forsyth School of Dental Hygiene at MCPHS University.
Acknowledgments
The authors would like to acknowledge and recognize the following individuals for their willingness to cooperate with participant recruitment for this study: Delphine Severe, DDS; Danette Manzi, Chief Compliance Office, CSHM; and Dental Center staff. Much appreciation is also extended to the experts who were instrumental in survey development and validation: Lisa F. Harper Mallonee, BSDH, MPH, RD, LD; and Cyndee Stegeman, EdD, RDH, RD, LD, CDE.
References
1. Guideline on perinatal oral health care. American Academy of Pediatric Dentistry [Internet]. 2011 [cited 2016 February 5]. Available from: http://www.aapd.org/media/policies_guidelines/g_perinataloralhealthcare.pdf.
2. Bader JD, Rozier G, Harris R, Lohr KN. Dental caries prevention: The physician’s role in child oral health systematic evidence review. Agency for Healthcare Research and Quality (US); 2004 Apr.
3. Nunn ME, Braunstein NS, Krall Kaye EA, et al. Healthy eating index is a predictor of early childhood caries. J Dent Res. 2009;88(4):361-366.
4. Kawashita Y, Kitamura M, Saito T. Early childhood caries. Int J Dent. 2011;1-7.
5. Harrison R. Oral health promotion for high-risk children: Case studies from British Columbia. J Can Dent Assoc. 2003;69(5):292-296.
6. Mobley C, Marshall TA, Milgrom P, Coldwell SE. The contribution of dietary factors to dental caries and disparities in caries. Acad Pediatr. 2009;9(6):410-414.
7. Palmer CA, Kent R Jr, Loo CY, et al. Diet and caries-associated bacteria in severe early childhood caries. J Dent Res. 2010;89(11):1224-1229.
8. Kagihara LE, Niederhauser VP, Stark M. Assessment, management, and prevention of early childhood caries. J Am Acad Nurse Pract. 2009;21(1):1-10.
9. Warren JJ, Weber-Gasparoni K, Marshall TA, et al. A longitudinal study of dental caries risk among very young low SES children. Community Dent Oral Epidemiol. 2009;37(2):116-122.
10. Prakash P, Subramaniam P, Durgesh BH, Konde S. Prevalence of early childhood caries and associated risk factors in preschool children of urban bangalore, india: A cross-sectional study. Eur J Dent. 2012;6(2):141-152.
11. Definition of early childhood caries (ECC). American Academy of Pediatric Dentistry [Internet]. 2003 [cited 2013 February 17]. Available from: http://www.aapd.org/assets/1/7/D_ECC.pdf.
12. Bugis BA. Early childhood caries and the impact of current U.S. Medicaid program: An overview. Int J Dent. 2012;1-7.
13. Mouradian WE, Wehr E, Crall JJ. Disparities in children’s oral health and access to dental care. JAMA. 2000;284(20):2625-2631.
14. Vargas CM, Ronzio CR. Disparities in early childhood caries. BMC Oral Health. 2006;6(Suppl 1):S3.
15. Reisine ST, Psoter W. Socioeconomic status and selected behavioral determinants as risk factors for dental caries. J Dent Educ. 2001;65(10):1009-1016.
16. Edelstein BL, Chinn CH. Update on disparities in oral health and access to dental care for america’s children. Acad Pediatr. 2009;9(6):415-419.
17. Brown JG. Children’s dental services under Medicaid: Access and utilization. Office of Inspector General, Department of Health and Human Services. 1996.
18. Definition of a Dental Home. American Academy of Pediatric Dentistry [Internet]. 2015 [cited 2016 February 5]. Available from: http://www.aapd.org/media/policies_guidelines/d_dentalhome.pdf.
19. Policy on the dental home. American Academy of Pediatric Dentistry [Internet]. 2015 [cited 2016 February 5]. Available from: http://www.aapd.org/media/policies_guidelines/p_dentalhome.pdf.
20. State quick facts. U.S. Census Bureau [Internet]. 2011 [cited 2013 March 24]. Available from: http://quickfacts.census.gov/qfd/states/33/3345140.html.
21. New Hampshire Medicaid Annual Report, 2011. New Hampshire Department of Health and Human Services. 2011.
22. National Health and Nutritional Examination Survey: Dental examiners procedures manual. Centers for Disease Control and Prevention. 2003.
23. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? appraisal and recommendations. Res Nurs Health. 2007;30(4):459-467.
24. World Health Organization. Oral health surveys—basic methods. 4th Edition ed. Geneva: World Health Organization; 1997.
25. McHugh ML. The chi-square test of independence. Biochem Med (Zagreb). 2013;23(2):143-149.
26. Mann HB, Whitney DR. On a test of whether one or two random variable is stochiastically larger than the other. Ann Math Statist. 1947;18(1);50-60.
27. Rothman KJ. Six persistent research misconceptions. J Gen Intern Med. 2014;29(7):1060-1064.
28. Schervish MJ. A review of mulitvariate analysis. Stat Sci. 1987;2(4):396-413.
29. Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993;138(11):923-936.
30. Harrell FE. Regression Modeling Strategies with Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer-Verlag: New York. 2001.
31. Hayat MJ, Higgins M. Understanding poisson regression. J Nurs Educ. 2014;53(4):207-215.
32. Patrick DL, Lee RS, Nucci M, et al. Reducing oral health disparities: A focus on social and cultural determinants. BMC Oral Health. 2006;6(Suppl 1):S4.
33. Almeida AG, Roseman MM, Sheff M, et al. Future caries susceptibility in children with early childhood caries following treatment under general anesthesia. Pediatr Dent. 2000;22(4):302-306.
34. American Academy of Pediatric Dentistry. Oral health policies. Pediatr Dent. 1999;21:18-37.
35. Healthy living-oral health. American Academy of Pediatrics [Internet]. 2007 [cited 2013 January 27]. Available from: https://www.healthychildren.org/English/healthy-living/oral-health/Pages/default.aspx.
36. Establishing a dental home: Using the American academy of pediatric dentistry’s caries risk assessment tool (CAT) as a first step. American Academy of Pediatric Dentistry Foundation [Internet]. 2002 [cited 2013 January 27]. Available from: www.aapd.org/foundation.
37. Children’s oral health. Centers for Disease Control and Prevention. 2011.