You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In an ever more digital world, digital radiography is rapidly replacing analog film-based methods.1 A growing number of US dentists—10% to 30% in 20112—have already incorporated the technology, which can offer numerous advantages over film-based radiography3,4,5,6,7 including: speed of viewing; image enhancement capabilities; ease of sharing digital files for second opinions and co-diagnosis; the potential for reduced patient radiation exposure in keeping with the ALARA (As Low As Reasonably Achievable) principle;8,9 and permitting better patient understanding of their oral conditions.7 It also requires less space and eliminates costs and inconvenience associated with maintaining and discarding processing fluids.10
Other reasons digital radiography is rapidly becoming the norm relate to pending government requirements and standards for information transfer. Electronic health records (EHR) are becoming a reality. CDC reported in 2009 that the EHR adoption rate among medical practitioners was 48.3%—up from 38.4 % in 2008.11 This rate will surely rise as those practitioners who are not using EHR by January 2015 will be subject to Congress-mandated payment adjustments, and these will be applied to Medicare-eligible professionals (EPs) who are not demonstrating meaningful use of Certified Electronic Health Record Technology under the Medicare EHR Incentive Programs. These payment adjustments will be applied beginning on January 1, 2015, for Medicare EPs.12 Then, too, to consider is the need for electronic file exchange using DICOM (Digital Imaging and Communication in Medicine), a standard advocated by the American Dental Association (ADA) for handling, storing, printing, and transmitting medical imaging information about patients, procedures, and the diagnostic images themselves, which enables the integration of scanners, servers, workstations, printers, and file exchange between DICOM-compatible offices.13,14
Options
Among digital technology options that are useful for the general practitioner are 2D intraoral and extraoral systems including panoramic imaging (both solid state or photostimulable phosphor), as well as 3D systems, mainly cone beam computed tomography (CBCT). All have their respective advantages and disadvantages, which—along with their features—are discussed below.3,7,10,15-25
Intraoral Radiography
Whether traditional film-based or digital, an intraoral radiography method is needed by virtually all general practices for diagnosing a variety of dental problems. Due to their ability to capture detail, intraoral digital imaging methods are especially suitable for diagnosing periapical lesions, caries, and periodontal disease.
The digital advantages of image enhancement capabilities (Figure 1) and transmission can be achieved either with one-step methods, where the image is sent from a solid-state digital sensor placed in the patient’s mouth to the computer monitor, or a two-step method, where first the image is taken using a photostimulated phosphor (PSP) plate that is processed using a laser scanner that sends the image to the computer monitor.
Solid-State Method
There are two main types of detectors presently in use for solid-state 2D dental radiography—charge-coupled device (CCD) and complementary metal-oxide semiconductor (CMOS). Both involve the placement of a digital sensor in the patient’s mouth, as described above. CMOS chips tend to provide a wider recording latitude and are not subject to picture element blooming, which can occur with overexposure and saturation of a CCD chip.
Advantages of solid-state intraoral radiography include high image quality, which is at least equivalent to analog film exposed and processed optimally, and to photostimulable phosphor images. Solid state sensors are robust and rarely need to be repaired or replaced, while film can only be used once, and the photostimulable phosphors used for intraoral imaging tend to wear and scratch over time with use. Disadvantages of solid-state intraoral x-ray sensors include greater expense initially to buy the sensor, possible patient discomfort caused by the rigid sensor, and the learning curve involved in its use, including achieving more patient-friendly placement. There are also issues involving disinfection of the sensor between uses and the placement of plastic barriers that are needed with solid-state intraoral sensors.
Photostimulable Phosphor Method
The use of photostimulable phosphors can be less expensive in an office that requires multiple detectors. It also involves less of a learning curve because they are placed in the mouth in a similar way to the film-based method. There is placement of a thin flexible phosphor plate in the patient’s mouth using a “film” holder, then the image is transferred from the plate to the computer using scanning by a solid-state red laser, photo multiplication, and digitization. The flexible plates can be more comfortable for patients compared to rigid oral sensors, and larger photostimulable phosphor plates also can be used with film-based panoramic systems where the image film intensifying screens are removed from the cassette. However, intraoral photostimulable plates do scratch and periodically require replacement. Also to consider is that the extra processing step with images means it is somewhat less “instant.”
Extraoral Radiography Methods
Both solid-state and photostimulable phosphor radiography methods are available for extraoral use. Except for issues related to their placement in patients’ mouths, which is not a factor in extraoral radiography, their relative advantages and disadvantages are similar to those described above—ie, solid-state digital is more convenient and slightly more expensive; extraoral photostimulable phosphor imaging is less convenient and can be less expensive, especially because there is no need to replace the x-ray generator. For extraoral digital radiography using photostimulable phosphors, film cassettes can be simply modified by removing the film image intensifier screens.
Like intraoral digital imaging, extraoral methods eliminate the need for a darkroom; they also have the ability to readily enhance and analyze images, and they offer the convenience of image storage, duplication, and retrieval. With extraoral radiography, the image file size is larger than that generated by intraoral imaging, which can be reduced by lossless compression techniques that facilitate storage without compromising the diagnostic quality of the image.10,21 As computer power has grown and digital storage has come down in price, the need for compression of files has declined.
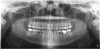
Panoramic
A digital panoramic radiograph (Figure 2) is indicated for circumstances in which intraoral imaging is not practical, as in patients who cannot open their mouth due to trismus or in those who cannot tolerate having a sensor or film in their mouth due to severe mucositis following radiation therapy for cancer. Advantages of panoramic imaging are that it quickly provides broad coverage of facial bones and teeth, it is convenient for both dental practitioner and patient, and is a helpful visual aid in patient education and case presentation.
Drawbacks of panoramic imaging are the cost—$25,000 to $85,00020 —and that vertical beam angulation is not adjustable. Also to keep in mind is that, like a traditional panoramic machine, the digital unit requires dedicated operatory space, so there is no space savings other than not needing a darkroom.
CBCT
CBCT is indicated implant planning; developing surgical guides; general observation; finding the correct number of canals in abscessed teeth requiring endodontic treatment; in some cases, for orthodontic planning for patients with asymmetries or who need surgical procedures; for evaluation of impacted teeth or TMJ; and as an adjunct for intraoral imaging. Perhaps the most important CBCT advantage is that it offers a “third dimension” for diagnostic accuracy (Figure 3).23
Other benefits include: its short scan time; nearly immediate availability of images; compatibility with practice management software; ability to identify a variety of incidental findings, such as carotid artery calcifications; and facilitation of patient communication/education. Like any imaging in dentistry, CBCT should only be used for dental purposes, but incidental findings should be recorded when they are present. CBCT should not be used specifically for screening for carotid calcification, as duplex Doppler ultrasound is the method of choice for inspecting blood clots in the carotids. When calcification is found in the carotids, or other conditions of general health importance are found, the patient should be referred to the appropriate physician for further follow-up and treatment if needed. While there is a learning curve for reading the full image volumes, there are services available for this. Like CBCT, it is extraoral, so its advantages include that it is more comfortable for patients and can be used in patients who cannot tolerate having a sensor or film in their mouth. It can also be used when intraoral scanning is not practical—eg, for a panoramic bitewing.
It should be emphasized that CBCT should not be considered a replacement for intraoral imaging in the general practice office.20,25 In that regard, pertinent disadvantages are that it offers insufficient detail for diagnosing caries, periodontal disease, and small lesions in the bone. This is due to CBCT beam hardening artifacts and streaking caused by metallic restorations. Additional considerations include its cost, that it requires dedicated operatory space, and that Centers for Medicare & Medicaid Services requires facility accreditation and continuing eduction for its reimbursement of Medicare or Medicaid patients.26 Also to consider is that it delivers a higher radiation dose than does the full-mouth series (FMX) performed with round collimation.25
Hybrid/Combinations
With the goal of providing comprehensive, custom care for every patient, costs and benefits of the above technologies can be weighed in determining an appropriate combination of available options (intra- and extra-orally).14 Hybrid systems made up of differing combinations of available options offer flexibility to enable the clinician to best address clinical situations. An example would be having a panoramic system—with either storage phosphor plates or a direct digital panoramic system—and using direct extraoral imaging with both direct sensors and a PSP system for intraoral use.
Purchase Considerations
Practice Scope and Finances
Also to factor into the purchase of new technology are future as well as current practice needs. This includes the task performed—eg, implants, caries detection, root canals—which may well be determined by the patient population. For example, practices with a large proportion of Medicare or Medicaid patients should be aware that CMS requires that private practices using point-of-care CT scanning devices obtain accreditation, which includes continuing education requirements, in order to be eligible for reimbursement by CMS.20,26
Budgetary considerations may include the flexibility of purchase, whether old and new technology will be used concurrently, and tax implications—eg, the Section 179 deduction27 that offers a tax break at the end of the fiscal year for purchase of equipment.
Staff
Staff should also be included in the decision-making process. Practitioners should solicit their input, assess how new equipment will impact their responsibilities; and discuss training requirements—especially with significantly advanced technology and techniques. Together, the team should evaluate training options. They should also focus on existing skill sets. Is the staff technology/computer savvy? Is the staff strong on insurance coding/management?14
Space
The office layout, too, must be considered. Although saving space is a benefit of digital systems, which do not require the chemicals and processing needed by film-based systems, that is only the case if film-based systems are eliminated entirely. Some things to keep in mind: panoramic and CBCT units need a dedicated area and workstation to control the acquisition device, and the digital scanner that acquires and processes images with indirect system using PSP must be attached to a computer workstation.28
Information Gathering
Information Sources
Researching products that meet the practice’s needs with the above factors in mind should be multifaceted, and may involve online sources, journals, or CE courses. Especially valuable is discussion—by all team members, including assistants and hygienists—with study groups, professional societies, and colleagues. Of course, the practitioner and key personnel should also speak to and meet with manufacturers’ representatives prepared to address crucial questions. It is critical to find objective data and unbiased resources to determine the best system for the individual practice.
Practices considering a particular system may be able to take it for a “trial run” to determine if it is appropriate for their needs prior to purchasing. This enables the dental team to ask questions and express their concerns, as they also can during initial training by the company after system purchase and installation.29
What You Need to Know
Before purchasing a system, it is important to learn in advance as much as possible—especially about the issues that may not come immediately to mind.14
Some questions to ask:
• Will existing technology need to be upgraded or replaced?
• Is the software compatible with the current practice management system?
• Does the manufacturer provide training? (This is especially important with CBCT due to CMS requirements of 4 hours from the manufacturer as well as 20 hours from elsewhere initially.)
• What type of hardware or software support is available?
• Does it include technical support? Equipment maintenance? Software upgrades?
• Is it provided by the manufacturer or is it outsourced?
• Is there 24/7 support or is access limited?
It is also important to find out if the system is Digital Imaging and Communications in Medicine (DICOM)-compliant to ensure that images can be acquired, saved, and transferred properly.24 Digital radiographic systems that are DICOM-compliant use file formats that are universally accepted, thus permitting image transfer or teleradiography for a variety of purposes.24 When it comes to storing and sharing data with digital radiographic systems, it is essential to follow Health Insurance Portability and Accountability Act (HIPAA) regulations. All patient health information and data, especially radiographic images, need to be maintained and protected.24The ADA Standards Committee on Dental Informatics has prepared a Technical Report outlining the protocol on how DICOM-conformant images can be securely emailed in a HIPAA-compliant manner.29,30
Installation
Three key considerations when installing new technology are wiring, space, and equipment location.28
Although wireless technology is advancing, the fastest, most reliable, and most secure method today is a wired connection for solid-state digital scanners. Space considerations revolve largely around workflow of patients and staff. (Switching to digital can improve workflow because digital radiography systems can be integrated into imaging and practice management software. Patients can receive a faster diagnosis, and professionals can spend more time with their patients.)
As for equipment location, it should facilitate ease of use and efficient workflow and stored to enable convenient access. Monitor location for image viewing depends on where and when images are viewed and by whom—eg, by the dentist while performing a procedure or by the patient for education and consultation purposes. A 21-inch or larger monitor allows for better viewing of radiographs, compared to the standard No. 2- size film.28 The recommended minimum contrast ratio of the monitor should be 500:1,28 and because solid-state intraoral sensor systems are used in multiple operatories, they should have a quick connect/disconnect interface and be located and stored appropriately.28 They should also be easily disinfected.
It is prudent to plan for space and wiring in anticipation of future technology and equipment purchases.
Integration
Your Network
A properly designed and installed network enables movement of files between operatories, workstations, offices, practices, and insurers (Figure 4). Viewing the same information on different computers or workstations requires a computer network that enables sharing information on multiple machines. The value of a properly designed and secured network cannot be overstated. An improperly designed and installed network is the cause of many of the problems reported in daily system use.
The Server
The place where images are saved and stored for use on workstations should be a central location to facilitate retrieval, data protection, simultaneous access to data stored on multiple drives, and backup.7
Practitioners should be aware that Redundant Array of Independent Discs (RAID), a backup system commonly used in companies and practices, will not protect against catastrophic loss (eg, fire, flood, etc). Therefore, it is necessary to have offsite backup, which is easily facilitated by digital technology.28
Offsite Backup
For offsite backup, practitioners must choose between storage-based online—ie, in the “cloud”—or removable via an external hard drive that is removed from the office each day.28
HIPAA-level security is necessary for all protected health information, including diagnostic images.
Ongoing Maintenance
Practitioners should also have a plan in place for ongoing maintenance concerning how the system will be maintained and supported as well as installed. It is important that the manufacturer be able to provide information technology as well as hardware support. Annual contract agreements are particularly important to protect the investment in upper-level items such as CBCT units.
Employee Training/Continuing Education
While only a dentist or specialist can diagnose radiographs, the taking of radiographs may involve roles and responsibilities for the entire team, all of whom should receive training to familiarize them with new equipment and its appropriate uses.14 Personnel who will be using the equipment should receive training on how to use it properly for patient comfort, safety, and maximum effectiveness —including physical positioning of the patient (extraoral), positioning of the sensor (intraoral), software operation (image adjustment, etc), and minimizing patient radiation exposure in keeping with the ALARA principle.9
Transitioning to a digital system can seem daunting, and early training with the technology is the key to overcoming fear and hesitation. But the advantages of having a properly planned system cannot be understated. They include: integrated storage with access to images through practice management software systems; security of available backup and off-site archiving; perfect radiographic duplicates to accompany referrals; security mechanisms to identify original images and differentiate them from altered images; the ability to tag information such as a patient identifier, date of exposure and other relevant details; and interoperability of the DICOM file format.30,31
Conclusion
To prepare for future technology, practitioners should periodically re-evaluate the needs of the practice and available technology and consider phasing out and replacing traditional technology with digital options. They should also make an effort to remain abreast of technology that can improve efficiency, patient care, and adherence to compliance requirements.
Because every practice is different, new technology should be assessed in terms of how it can improve current methods or resolve problems such as bottlenecks and inefficiencies in the practice workflow.
As oral healthcare evolves into a medical and wellness model, and all healthcare records turn digital, the clinician’s ability to stay current with high-quality diagnostic information will be central to the next level of patient care.
About the Author
Allan G. Farman, BDS, PhD, DSc (Odont)
Dr. Allan G. Farman holds doctorates in oral and maxillofacial pathology (PhD) and in oral and maxillofacial radiology (DSc), both from the University of Stellenbosch, South Africa. He has graduate degrees in education (EdS, higher education administration) and business administration (MBA with distinction) from the University of Louisville, Kentucky, where he was a professor of radiology and imaging science in the Department of Surgical and Hospital Dentistry, School of Dentistry, and an adjunct professor of anatomical sciences and neurobiology and clinical professor of diagnostic radiology in the School of Medicine until last year.
A diplomate of the American Board of Oral and Maxillofacial Radiology, Dr. Farman is the founder of the International Congress on Computed Maxillofacial Imaging, and was the 11th president of the International Association of DentoMaxilloFacial Radiology. He was the First Honorary President for the Latin American Congress on DentoMaxilloFacial Radiology, held in Brazil in 1996. He is a member of the DICOM International Congress Organizing Committee.
References
1 Eshraghi T, McAllister N, McAllister B. Clinical applications of digital 2-D and 3-D radiography for the periodontist. J Evid Based Dent Pract. 2012;12(3 Suppl):36-45.
2. Univeristy of Rochester Medical Center. Digital X-Rays Give Dentists the Big Picture. www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=1&ContentID=4060. Accessed January 11, 2014.
3. Wenzel A. A review of dentists' use of digital radiography and caries diagnosis with digital systems. Dentomaxillofac Radiol. 2006;35(5):307-314.
4. White SC, Pharoah MJ. Oral Radiology: Principle and Interpretation. 6th ed. St. Louis: Mosby-Year Book Inc; 2009:78-80.
5. Parissis N, Kondylidou-Sidira A, Tsirlis A, Patias P. Conventional radiographs vs digitized radiographs: image quality assessment. Dentomaxillofac Radiol. 2005;34(6):353-356.
6. Christensen GJ. Why switch to digital radiography? J Am Dent Assoc. 2004;135(10):1437-1439.
7. Watson JA. A perspective on digital radiography. Inside Dentistry. 2011;7(6):100-104.
8. Bahreyni Toossi MT, Akbari F, Bayani Roodi S. Radiation exposure to critical organs in panoramic dental examination. Acta Med Iran. 2012;50(12):809-813.
9. Paulhamus C. The ALARA principle in practice. Inside Dentistry. 2013;9(Spec Iss 4):26-31.
10. Freedman G. Wireless digital sensors. July 2013. http://www.oralhealthgroup.com/news/wireless-digital-sensors/1002445816/?&er=NA. Accessed May 16, 2014.
11. Hsiao C-J, Hing E, Socey TC, Cai B. December 2010 Electronic Medical Record/Electronic Health Record Systems of Office-based Physicians: United States, 2009 and Preliminary 2010 State Estimates. Division of Health Care Statistics. http://www.cdc.gov/nchs/data/hestat/emr_ehr_09/emr_ehr_09.pdf. Accessed May 16, 2014.
12. Payment Adjustments & Hardship Exceptions Tipsheet for Eligible Professionals.Updated: March 2014. http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/PaymentAdj_HardshipExcepTipSheetforEP.pdf. Accessed May 16, 2014.
13. DICOM. Wikipedia. http://en.wikipedia.org/w/index.php?title=Digital_Imaging_and_Communications_in_Medicine&oldid=154283703. Accessed May 16, 2014.
14. Benjamin S. Planning for success: Moving forward with digital dental radiography. Inside Dentistry. 2013;9(Spec Iss 4):2-6.
15. Dias da Silva PR, Martins Marques M, Steagall W Jr, et al. Accuracy of direct digital radiography for detecting occlusal caries in primary teeth compared with conventional radiography and visual inspection: an in vitro study. Dentomaxillofac Radiol. 2010;39(6):362-367.
16. Borg E, Gröndahl H-G. Image plate systems differ in physical performance. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(1):118-124.
17. Hintze H, Wenzel A. Influence of the validation method on diagnostic accuracy for caries. A comparison of six digital and two conventional radiographic systems. Dentomaxillofac Radiol. 2002;31(1):44-49.
18. Digital Radiography Systems: Comparison of Sensor Technologies.
http://www.ada.org/sections/scienceAndResearch/pdfs/0607_digital_sensors.pdf
19. Dale Miles. Learn Digital. http://learndigital.net/articles/part1.htm. Accessed May 16, 2014.
20. Tuleya S. Breaking down today’s radiographic systems. Inside Dentistry. 2013;9(Spec Iss 4):8-11.
21. Williamson GF, Scarfe WC. Practical panoramic radiography. www.dentalcare.com/en-US/dental-education/continuing-education/ce71/ce71.aspx?ModuleName=coursecontent&PartID=0&SectionID=-1. Accessed May 16, 2014.
22. Alshehri MA, Alamri HM, Mazen MM. CBCT applications in dental practice: A literature review. Dec 6, 2010. http://www.dental-tribune.com/articles/specialities/general_dentistry/3615_cbct_applications_in_dental_practice_a_literature_review.html. Accessed May 16, 2014.
23. Braun X, Ritter L, Jervøe-Storm PM, Frentzen M. Diagnostic accuracy of CBCT for periodontal lesions. Clin Oral Investig. 2014;18(4):1229-1236 [Abstract].
24. Williamson GF. Digital radiography in dentistry: moving from film-based to digital imaging. www.dentalcare.com/en-US/dental-education/continuing-education/ce350/ce350.aspx?ModuleName=coursecontent&PartID=7&SectionID=-1. Accessed May 16, 2014.
25. Lorenzoni DC, Bolognese AM, Garib DG, et al. Cone-beam computed tomography and radiographs in dentistry: aspects related to radiation dose. Int J Dent. 2012;2012:813768. doi: 10.1155/2012/813768. Epub 2012 Apr 4.
26. Obtaining Accreditation for CT Scanning Devices (PDF).www.carestream.com/WhitePaper-Accreditation-7615. Accessed May 16, 2014.
27. IRS Section 179 Tax Deduction—Should You Invest in New Dental Equipment? Inside Dentistry. 2013;9(11):34-36.
28. Benjamin S. Installation and integration of radiographic technology. Inside Dentistry. 2013;9(Spec Iss 4):12-14.
29. DiMatteo AM, Latanyshyn KA. Training for and implementing digital radiography systems. Inside Dentistry. 2013;9(Spec Iss 4):16-19.
30. Paulhamus C. Conforming and protecting image transfer. Inside Dentistry. 2013;9(Spec Iss 4):21-24.
31. ADA Technical Report No. 1048. Attachment of DICOM Datasets Using E-Mail in Dentistry. Chicago: American Dental Association; 2011. http://www.ada.org/en/science-research/dental-standards/standards-committee-on-dental-informatics/standards-technical-specifications-and-technical-reports. Accessed May 16, 2014.