You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Pain is a multidimensional experience; therefore, the perception of pain is a subjective and individual response. It is associated not only with physical stimulation, but with emotional and psychological factors as well. Pain is described as an “unpleasant sensory and emotional experience associated with actual or potential tissue damage.”1 A physical stimulus causes an impulse to travel through the body’s nerves and deliver a message of pain to the central nervous system. It has been suggested that psychological experiences, such as emotions, have an effect on the body’s perception of pain by altering the pain threshold.1,2 The result is that physical stimuli may feel more painful to an individual under stressful versus low-stress situations. Therefore, it would be expected that subjects with dental fear or anxiety would express higher levels of pain perception compared to patients who have no dental fear or anxiety.2-4
Endoscopic technology has been used in the medical field for years, but has only recently become available for use in dentistry. Currently, the use of periodontal endoscopy in dental practice is limited. Recent investigations have examined the use of periodontal endoscopy in an effort to improve the outcome of scaling and root planing. The bulk of this research has been conducted on sites that have been non-responsive to traditional therapy.5-7
A periodontal endoscope consists of a bundle of fiber optic strands measuring less than 1 mm wide through which light travels. The end of the fiber optic bundle is covered by a sterile, disposable sheath, which is attached to an “explorer.” This explorer is inserted below the gingival margin into the periodontal pocket to provide illuminated subgingival visualization. A water lavage flushes biofilm, blood and other subgingival debris out of the field of vision. This enables the clinician to visualize intra-pocket tissue in Flammarion, subgingival plaque, root surfaces, calculus deposits and other structures within a periodontal pocket that normally would not be visible. The images from a periodontal endoscope are displayed in real-time video on a monitor allowing the clinician to view subgingival structures 15 to 46 times their actual size.5,8
The goal of scaling and root planing is to remove calcified deposits, plaque biofilm and endotoxins from the root and soft tissue pocket. Studies have shown that incomplete deposit removal from the root surfaces impedes ideal healing of the periodontal tissues.9-13 Therefore, it is important for clinicians to remove as much subgingival deposit as possible to ensure optimum healing. Unfortunately, clinicians do not always achieve this complete level of deposit removal during traditional scaling and root planing procedures.11,14-22 With the aid of subgingival visualization provided by the periodontal endoscope, early research has shown the endoscope to enhance calculus removal by allowing the clinician to see the root structures during and after scaling procedures to see if and where calculus remains.5-7,9,23 However, a pilot study conducted at the University of North Carolina Chapel Hill examined treatment outcomes on subjects treated for non-responsive sites of periodontal disease by comparing the control group, which received scaling and root planing, and the experimental group, which received scaling and root planing with perioscopy. Subjects were followed for 3 months after treatment was completed. No statistically significant differences were found in the clinical and inflammatory assessments of subjects when the control sites and experimental sites were compared.24
Early users of the periodontal endoscope advocated the use of local anesthetics to ensure patient comfort.8 However, the required use of anesthetics could be a deterrent for both the subject and the clinician. For the clinician, injection of local anesthetics adds to treatment time and involves potential risks associated with its use. For the subject, the discomfort of the injection itself may be a deterrent. It would be beneficial to both the subject and clinician to be able to use the endoscope without routinely administering local anesthesia.
The purpose of this study was to determine the amount of perceived pain reported by subjects during subgingival visualization utilizing the periodontal endoscope compared with the use of a periodontal probe. If the periodontal endoscope is to become widely accepted in the practice of dentistry, with the intent of improving outcomes of scaling and root planing, clinicians should be aware of the patients’ perceptions of the device.
A review of the literature over the past 15 years was performed in order to find clinical research in the field of dentistry utilizing pain scales or surveys. Since the perception of pain is subjective, it can be difficult to get accurate or reliable measures of subjects’ pain levels. Several surveys and indicators have been developed in an attempt to achieve standardized measures of pain and pain intensity.
The McGill Pain Questionnaire has shown high internal consistency and has been suggested that it is the best pain scale to use in research.25 Due to its length, however, it has also been recommended that the McGill Questionnaire should be used as an adjunct to other simpler and quicker pain assessments.26 The West Haven-Yale Multi-Dimensional Pain Inventory has also shown high internal consistency, but it was invented to assess general pain, not specific dental pain. Therefore, it has not been used frequently in dental studies.2,27,28 The Pain Anxiety Symptoms Scale (PASS) has shown high internal consistency and validity.4,29,30 The Descriptor Differential Scale (DDS) of Pain Intensity was developed to measure clinical pain by applying psychophysical components. The DDS has shown validity, reliability and consistency, yet its use in dental research has been limited to this point.31,32
The Heft-Parker Modified Visual Analogue Scale (VAS) is a variation of the original VAS. It is a 170 mm horizontal line that has verbal descriptors as end anchors, but also includes other verbal guides (faint, weak, mild, moderate, strong and intense) along the scale in order to aid an individual in best describing his or her level of pain. The subject is instructed to make a dash on the line indicating their current level of pain. The pain level is the distance, in millimeters, from the endpoint on the left to the dash marked on the scale. Both the original VAS and the Heft-Parker VAS have shown reliability, validity and sensitivity in numerous dental and non-dental pain studies.25,33-38 Due to the ease of administration of the VAS and its high validity and reliability, it has been used most commonly for pain measurements in dental research.
Over the years, various aspects of dental related pain have been studied. Several studies found no significant difference in levels of perceived pain using different instruments or even different modalities of treatment.1,39-42 One exception to these findings was a 2004 study in which subjects felt the Vector™ system scaler caused significantly less pain when compared to a traditional piezo-electric ultrasonic scaler during periodontal maintenance appointments.3
Pain experienced in relationship to treatment provided by different clinicians or in different office set tings has also been investigated.43 Several studies showed that levels of discomfort experienced decreased with an increase in age.42-44 Many study reports found women show more pain experience, more intense levels of pain and longer duration of pain as compared to men.33,44-48 Although most studies in this review of the literature support differences in pain perception between ages and genders, other reports show no difference between these groups.1,2,36,42,43
Several studies have shown that there is a difference in the amount of pain a subject feels depending on the area of the mouth being probed, the presence of gingival inflammation, differences in therapists’ probing force, higher blood pressure measurements, cigarette smoking, and presence of dental or general anxiety.1-3,30,33,34,42,49,50
A Belgian study conducted on 268 subjects found there was a high correlation between the perceived pain of the current treatment and pain experienced during previous appointments. Both treatment groups reported issues or discomfort associated with use of local anesthesia during previous scaling procedures. In fact, 33% of group 1, and 64% of group 2 reported they would be willing to endure moderate pain in order to avoid use of local anesthetic, and 35% of 1 group reported that the most bothersome part of the treatment was the injection.34 This supports findings of other research studies that show subjects experience high levels of pain or discomfort associated with dental injections, and one study where adults admitted that pain associated with dental injections is enough to make them avoid dental treatment altogether.51-55 These statistics are a strong argument for utilizing the periodontal endoscope without relying on administering anesthetics.
As mentioned previously, it has been found that a subject’s emotional status due to things such as stress, fear or anxiety can have an impact on the level or intensity of pain perceived.1 A study conducted by Karadottir et al sought to see if the degree of pain experienced by periodontal maintenance patients during probing and scaling could be predicted by other factors including dental anxiety.33 Prior to a periodontal maintenance appointment, the participants filled out 3 separate surveys. The first was the Dental Anxiety Question,56 followed by Corah’s Dental Anxiety Scale,57 and finally the Dental Fear Survey.58 Subjects reported their pain levels on a VAS and verbalized pain frequency during the treatment. After assessment of the data, 4 items were found as significant predictors of pain perception. The first predictor was gender; as supported by previous studies, females were found to have a higher pain response than males.33,44-48 The second predictor was a question from Corah’s Dental Anxiety Scale (“When you are waiting in the dentist’s office for your turn in the chair, how do you feel?”). The third and fourth predictors of pain perception were questions from the Dental Fear Survey (“How fearful are you about having your teeth cleaned?” and “In general, how fearful are you of having dental work done?”).33
This was one of the first studies published that suggested using fear or anxiety markers in an attempt to predict pain in dental patients. The goal of these findings was to identify those subjects who may be at highest risk for dental pain, and in turn make appropriate accommodations in order to make them comfortable through their treatment.59,60 In a follow up study to this one, it was found that a single question, “How fearful of having your teeth cleaned are you?” could be an effective predictor of pain perception. The review of the literature uncovered no research examining the perception of pain associated with the use of a periodontal endoscope. Therefore, the purpose of this study was to determine the amount of perceived pain reported by subjects undergoing treatment of periodontal disease with the assistance of a periodontal endoscope.
Methods and Materials
Two study examiners were trained on the use and techniques of the periodontal endoscope by a periodontist who was experienced with the instrument. After training sessions were completed, the examiners were tested with a calibration session to determine both intra- and inter-examiner reliability. The examiners assessed 6 periodontal subjects with the presence of subgingival calculus using both the periodontal endoscope and an 11/12 explorer. The post-training calibration showed high intra- and inter-examiner consistency and reliability was achieved with both methods of calculus detection.
Existing prophylaxis or periodontal recall patients within the University of Minnesota dental clinics were screened for inclusion and exclusion criteria during appointments at the school. After potential subjects were identified, 1 of 3 study investigators reviewed the study protocols and procedures with the subjects, and obtained informed consent. A total of 30 subjects (n=30) were selected as part of a larger research study at the University of Minnesota. The primary objective of the larger research study was to determine if the use of a periodontal endoscope improves periodontal outcomes of scaling and root planing when compared to scaling and root planing alone.
Inclusion criteria required each subject to be at least 18 years of age and have 4 to 6 sites in each of 2 quadrants with pocket depths measuring 5 to 8 mm. The test sites were selected to receive scaling and root planing therapy regardless of the subject’s previous treatment history. Exclusion criteria included any antibiotic use within the past 30 days, the need for antibiotic premedication for dental procedures or any other significant chronic medical or health problems that would generally contraindicate dental treatment (example: uncontrolled hypertension).
In order to eliminate dental anxiety as a confounding factor in determining the expressed levels of pain, each subject’s level of dental anxiety was measured prior to treatment. The questions used to obtain this information were the Dental Anxiety Question,56 and modifications from Corah’s Dental Anxiety Scale60 as based on the finding from Karadottir et al study33 on pain experienced during periodontal maintenance treatment, which determined specific questions as significant predictors of pain.
The Heft-Parker Modified Visual Analogue Scale (VAS) was selected based on its established reliability, validity and sensitivity in numerous dental and non-dental pain studies.25,33-38 Additionally, it is easy to administer and it measures pain on a continuum.
The study was a randomized, split-mouth design to scale and root plane (S/RP) specified sites within quadrants with or without the use of the periodontal endoscope. Study quadrants were randomly assigned by utilizing the program S-PLUS 8.0. The benefits of using a one-time, split-mouth design when examining subjects’ pain perception are: both instruments are used during the same treatment session eliminating confounding effects that may occur from utilizing different subjects for different treatments, and the potential for the emotional status of the subject to change from one treatment day to the next is eliminated.1
Prior to treatment, subjects were given a pretreatment survey that consisted of a Single-Item Dental Anxiety Question, as well as 4 other questions pertaining to anxiety (modifications from Co rash’s Dental Anxiety Scale) to determine each subject’s level of dental fear or anxiety. Subjects were shown the periodontal endoscope and informed that it would allow the clinician to see the subgingival structures, which was otherwise not an option when scaling unless a flap surgery was performed. Baseline data was then collected, which included gingival indices, full mouth periodontal probing, clinical attachment levels, bleeding upon probing, tactile detection of subgingival calculus with an 11/12 explorer and visual detection of subgingival calculus using the periodontal endoscope in the randomly assigned endoscope quadrant.
Full mouth periodontal probing was completed by 1 of 2 calibrated examiners, using a UNC 15 probe to measure 6 sites on each tooth. After probing was complete, subjects were given a Heft-Parker Modified VAS to measure their perceived pain in response to the probing. This initial VAS served to determine the approximate level of pain each subject was experiencing during a “normal” component of the periodontal exam or treatment. Immediately after the examiner used the periodontal endoscope for subgingival calculus visualization, the subject was given a second identical Heft-Parker Modified VAS, in addition to specific questions relating to the use of the periodontal endoscope. The post-visualization survey was used to determine the amount of perceived pain participants felt while the endoscope was being used as compared to the perceived pain felt during probing.
Descriptive statistics were calculated using SAS V9.1.3 to analyze the data for the questions (counts and percentages) and the VAS pain scores (means, standard deviations and range). One-sample t-tests were used to compare the mean probe VAS pain score, the mean periodontal endoscope VAS score and their mean difference (within patient) to zero. Two sample t-tests were used to compare the mean VAS pain scores between levels of anxiety from the pre-treatment questions. P-values less than 0.05 were deemed statistically significant.
Results
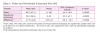
Six of the subjects did not completely answer all follow-up questions on the VAS administered after use of the periodontal endoscope, so the percentages are based on the total number of responses, not the total number of subjects for a few of the items on the post-treatment questionnaire. The mean VAS score during probing was 60.2 mm (Table I). This measurement falls closest to the verbal descriptor of “mild” discomfort as an aid on the VAS.
The mean VAS score for the periodontal endoscope was 33.0 mm (Table 1). This measurement falls closest to the verbal descriptor of “weak” discomfort as an aid on the VAS. The level of pain perceived was found to be significantly lower with the periodontal endoscope (p<0.0001) (Table 1).
Overall, 93.4% of the subjects experienced little or no pain during periodontal endoscope use (Table 2). A total of 37% of respondents reported no pain or discomfort with the use of the periodontal endoscope, 56.7% reported slight pain or discomfort and only 6.7% reported moderate pain or discomfort (Table 2). Of those that reported some pain for discomfort, 89.5% stated the pain was felt in the gums, while 10.5% felt it in the tooth being visualized with the endoscope. All of the subjects who experienced some pain or discomfort with the use of the periodontal endoscope felt that the potential benefits of enabling the clinician to visualize the subgingival area outweighed the discomfort felt. One subject (6.3%) stated that sight of the periodontal endoscope elicited slight levels of anxiety or fear, while 1 additional subject (6.3%) found the level of anxiety or fear elicited by the sight of the scope was more moderate. Overall, 75% of subjects said the level of pain felt was less with the periodontal endoscope than the probe, and 16.7% thought the two felt very similar. Only 2 respondents (8.3%) thought there was more pain experienced with the use of the scope versus the probe (Table 2).
Mean VAS scores for both the probe and the endoscope were compared with the subjects’ level of anxiety as assessed from the pre-treatment questionnaire. A total of 26.7% of subjects responded that they were afraid of going to the dentist (Table 3). With the exception of the compared VAS score for the probe and item #2 from the questionnaire (“If you had to go to the dentist tomorrow for a check-up how would you feel about it?”), all other mean VAS scores were higher for subjects who indicated some level of fear and/or anxiety (Table 4). The differences in VAS scores between the fear/anxiety and no fear/anxiety groups, however, were not found to be statistically significant.
Discussion
Periodontal endoscopy is an emerging technology in dental practice. There has been no previous research published examining the levels of perceived pain with the use of a periodontal endoscope. The results of this study may help expand the knowledge and use of this instrument in the fields of dentistry and dental hygiene.
Based on the findings from the current study, subjects did not find the periodontal endoscope to elicit significant anxiety or pain. Early users of the periodontal endoscope advocate the use of local anesthetics to ensure patient comfort.8 However, since the amount of discomfort expressed by the current study subjects was low, it may be possible for clinicians to use the periodontal endoscope for subgingival visualization without the use of local anesthetics. As revealed by the literature review, studies have shown many subjects find an injection of local anesthetic to be a stressful and painful experience.34,51-55 Therefore, the ability to use the endoscope throughout the mouth without the use of local anesthetics is of great advantage to the clinician.
Previous studies examining pain experience found that levels of perceived pain decreased as age increased, and that women expressed more perceived pain than men.33,42-48 The current study, however, showed no significant difference in reported pain experience between ages or sexes. This supports several other previous studies, which showed no difference in pain experience among such groups.1,2,36,42,43 It appears that past findings are conflicted on the issue of age and gender playing a role in pain perception. More definitive statistics need to be obtained in the future in order to determine if either of these items is of significant impact on pain perception.
It has also been previously suggested that a subject’s emotional status due to stress, fear or anxiety can have an impact on the level or intensity of pain perceived.1 The current study based a portion of the subject questionnaire on findings from a study conducted by Karadottir et al, which found specific questions from Corah’s Dental Anxiety Scale and the Dental Fear Survey to be effective predictors for increased pain perception.33 The current study found that all individuals that expressed some level of fear and/or anxiety did, in fact, report higher levels of perceived pain than those with no fear or anxiety. Although the current findings supported the concept of predictors of pain experience, the findings were not, however, deemed statistically significant. The ability to identify those individuals who may express a higher pain experience would be an important tool for clinicians; this is an issue that future research could expand upon in an effort to improve treatment experience for both subject and clinician.
Limitations
This was a pilot study with a relatively small sample of the population (n=30). It is a preliminary step in expanding the knowledge base of how periodontal endoscopes could be more widely utilized in periodontal and general dental practice. However, further research with larger populations should be performed in the future to determine patient acceptance and pain experience of this tool among a greater variety of individuals.
Achieving an accurate measurement of anxiety is extremely difficult, and therefore may also skew research outcomes. Since pain and anxiety are subjective, it is difficult to measure in quantitative terms. A subject may express anxiety to one aspect of treatment, but not to another - it is not necessarily a consistent level. With that in mind, although the periodontal endoscope did not elicit significant pain or anxiety during subgingival visualization, if calculus is detected and scaling and root planing is recommended, the use of local anesthetics may be necessary, therefore, eliciting different levels of anxiety.
An additional limitation is that this study compared the pain perception felt with simple visualization with the periodontal endoscope to that of periodontal probing. These both have similar methods of subgingival “instrumentation,” however, they are not performing the same task. Also, pain measurements were taken for full mouth periodontal probing, but the pain measurements for the periodontal endoscope were obtained after use in only 2 quadrants, not the entire mouth.
Due to the nature of the study, there was no way to blind the subjects or the examiners. There is no placebo for the periodontal endoscope, so both subjects and examiners knew if it was used or not. Lack of blinding could potentially cause bias among examiners.
Conclusion
The subjects of this study expressed the level of perceived pain or discomfort with the periodontal endoscope was significantly less than that experienced during periodontal probing. Therefore, administration of a local anesthetic was not necessary for subgingival visualization of the pocket environment during this study.
Kjersta Poppe, RDH, MDH, is the Director, Dental Hygiene at Lake Superior College.
Christine Blue, BSDH, MS, is an Associate Professor and Director, Division of Dental Hygiene, School of Dentistry, at the University of Minnesota.
References
1. Guzeldemir E, Toygar HU, Cilasun U. Pain perception and anxiety during scaling in periodontally healthy subjects. J Periodontol. 2008;79(12):2247-2255.
2. Newton JT, Buck DJ. Anxiety and pain measures in dentistry: a guide to their quality and application. J Am Dent Assoc. 2000;131(10):1449-1457.
3. Kuscu OO, Akyuz S. Is it the injection device or the anxiety experienced that causes pain during dental local anaesthesia? Int J Paediatr Dent. 2008;18(2):139-145.
4. McCracken LM, Zayfert C, Gross RT. The pain anxiety symptoms scale: development and validation of a scale to measure fear of pain. Pain. 1992;50(1):67-73.
5. Stambaugh RV, Meyers G, Ebling W, Beckman B, Stambaugh K. Endoscopic visualization of submarginal gingiva dental sulcus and tooth root surfaces. J Periodontol. 2002;73(4):374-382.
6. Geisinger ML, Mealey BL, Schoolfield J, Mellonig JT. The effectiveness of subgingival scaling and root planing: an evaluation of therapy with and without the use of the periodontal endoscope. J Periodontol. 2007;78(1):22-28.
7. Wilson TG Jr, Carnio J, Schenk R, Myers G. Absence of histologic signs of chronic inflammation following closed subgingival scaling and root planning using the dental endoscope: human biopsies: a pilot study. J Periodontol. 2008;79(11):2036-2041.
8. Kwan JY. Enhanced periodontal debridement with the use of micro ultrasonic, periodontal endoscopy. J Calif Dent Assoc. 2005;33(3):241-248.
9. Wilson TG, Harrel SK, Nunn ME, Francis B, Webb K. The relationship between the presence of tooth-borne subgingival deposits and inflammation found with a dental endoscope. J Periodontol. 2008;79(11):2029-2035.
10. Cobb CM. Non-surgical pocket therapy: mechanical. Ann Periodontol. 1996;1(1):443-490.
11. Kepic TJ, O’Leary TJ, Kafraway AH. Total calculus removal: an attainable objective? J Periodontol. 1990;61(1):16-20.
12. Sherman PR, Hutchens LH Jr, Jewson LG. The effectiveness of subgingival scaling and root planing. II. Clinical responses related to residual calculus. J Periodontol. 1990;61(1):9-15.
13. Robertson PB. The residual calculus paradox. J Periodontol. 1990;61(1):65-66.
14. Buchanan SA, Robertson PB. Calculus removal by scaling/root planing with and without surgical access. J Periodontol. 1987;58(3):159-163.
15. Caffesse RG, Sweeney PL, Smith BA. Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol. 1986:13(3):205-210.
16. Fleischer HC, Mellonig JT, Brayer WK, Gray JL, Barnett JD. Scaling and root planing efficacy in multirooted teeth. J Periodontol. 1989:60(7):402-409.
17. Rabbani GM, Ash MM Jr, Caffesse RG. The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol. 1981;52(3):119-123.
18. Sherman PR, Hutchens LH Jr, Jewson LG, Moriarty JM, Greco GW, McFall WT Jr. The effectiveness of subgingival scaling and root planning. I. Clinical detection of residual calculus. J Periodontol. 1990;61(1):3-8.
19. Nagy RJ, Otomo-Corgel J, Stambaugh R. The effectiveness of scaling and root planing with curets designed for deep pockets. J Periodontol. 1992;63(12):954-959.
20. Stambaugh RV, Dragoo M, Smith DM, Carasali L. The limits of subgingival scaling. Int J Periodontics Restorative Dent. 1981;1(5):30-41.
21. Jones SJ, Lozdan J, Boyde A. Tooth surfaces treated in situ with periodontal instruments. Scanning electron microscopic studies. Br Dent J. 1972;132(2): 57-64.
22. Jones WA, O’Leary TJ. The effectiveness of in vivo root planing in removing bacterial endotoxin from the roots of periodontally involved teeth. J Periodontol.1978; 49(7): 337-342.
23. Stambaugh RV. A clinician’s three year experience with perioscopy. Compend Contin Educ Dent. 2002;23(11A):1061-1070.
24. Avradopoulos V, Wilder RS, Chichester S, Offenbacher S. Clinical and inflammatory evaluation of perioscopy on patients with chronic periodontitis. J Dent Hyg. 2004;78(1):30-38.
25. Newton JT, Buck DJ. Anxiety and pain measures in dentistry: a guide to their quality and application. J Am Dent Assoc. 2000;131(10):1449-1457.
26. Grushka M, Sessle BJ. Applicability of the McGill pain questionnaire to the differentiation of “toothache” pain. Pain. 1984;19(1):49-57.
27. Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain. 1985;23(4):345-356.
28. Reisine ST, Fertig J, Weber J, Leder S. Impact of dental conditions on patients’ quality of life. Community Dent Oral Epidemiol. 1989;17(1):7-10.
29. Osman A, Barrios FX, Osman JR, Schneekloth R, Troutman JA. The pain anxiety symptoms scale: psychometric properties in a community sample. J Behav Med. 1994;17(5):511-522.
30. Burns JW, Mullen JT, Highdon LJ, Wei JM, Lansky D. Validity of the pain anxiety symptoms scale (PASS): prediction of physical capacity variables. Pain. 2000;84(2-3):247-252.
31. Gracely RH, Kwilosz DM. The descriptor differential scale: applying psychophysical principles to clinical pain assessment. Pain. 1988;35(3):279-288.
32. Doctor JN, Slater MA, Atkinson JH. The descriptor differential scale of pain intensity: an evaluation of item and scale properties. Pain. 1995;61(2):251-260.
33. Karadottir H, Lenoir L, Barbierato B, et al. Pain experienced by patients during periodontal maintenance treatment. J Periodontol. 2002;73(5):536-542.
34. van Steenberghe D, Garmyn P, Geers L, et al. Patients’ experience of pain and discomfort during instrumentation in the diagnosis and non-surgical treatment of periodontitis. J Periodontol. 2004;75(11):1465-1470.
35. Seymour RA. The use of pain scales in assessing the efficacy of analgesics in post-operative dental pain. Eur J Clin Pharmacol. 1982;23(5):441-444.
36. Stoltenberg JL, Osborn JB, Carlson JF, Hodges JS, Michalowicz BS. A preliminary study of intra-pocket topical versus injected anesthetic for scaling and root planing. J Clin Periodontol. 2007;34(10):892-896.
37. Hoffman A, Marshall RI, Bartold PM. Use of the Vector™ scaling unit in supportive periodontal therapy: a subjective patient evaluation. J Clin Periodontol. 2005;32(10):1089-1093.
38. Gallagher EJ, Bijur PE, Latimer C, Silver W. Reliability and validity of a visual analog scale for acute abdominal pain in the ED. Am J Emerg Med. 2002;20(4):287-90.
39. Kocher T, Rodemerk B, Fanghanel J, Meissner G. Pain during prophylaxis treatment elicited by two power-driven instruments. J Clin Periodontol. 2005;32(5):535-538.
40. Kocher T, Fanghanel J, Schwahn C, Ruhling A. A new ultrasonic device in maintenance therapy: perception of pain and clinical efficacy. J Clin Periodontol. 2005;32(4):425-429.
41. Aslund M, Suvan J, Moles DR, D’Aiuto F, Tonetti MS. Effects of two different methods of non-surgical periodontal therapy on patient perception of pain and quality of life: a randomized controlled clinical trial. J Periodontol. 2008;79(6):1031-1040.
42. Canakci CF, Canakci V. Pain experienced by patients undergoing different periodontal therapies. J Am Dent Assoc. 2007;138(12):1563-1573.
43. Fardal O, Johannessen AC, Linden GJ. Patient perceptions of periodontal therapy completed in a periodontal practice. J Periodontol. 2002;73(9):1060-1066.
44. Liddell A, Locker D. Gender and age differences in attitudes to dental pain and dental control. Community Dent Oral Epidemiol. 1997;25(4):314-318.
45. McGrath PA. Psychological aspects of pain perception. Arch Oral Biol. 1994;39:55S-62S.
46. Pihlstrom BL, Hargreaves KM, Bouwsma OJ, Myers WR, Goodale MB, Doyle MJ. Pain after periodontal scaling and root planing. J Am Dent Assoc. 1999;130(6):801-807.
47. Miaskowski C. Women and pain. Crit Care Nurs Clin North Am. 1997;9(4):453-458.
48. Unruh AM. Gender variations in clinical pain experience. Pain. 1996;65(2-3):123-167.
49. Heft MW, Perelmuter SH, Cooper BY, Magnusson I, Clark WB. Relationship between gingival inflammation and painfulness of periodontal probing. J Clin Periodontol. 1991;18(3):213-215.
50. Hassan MA, Bogle G, Quishenbery M, Stephens D, Riggs M, Egelberg J. Pain experienced by patients during periodontal recall examination using thinner versus thicker probes. J Periodontol. 2005;76(6):980-984.
51. Nanitsos E, Vartuli R, Forte A, Dennison PJ, Peck CC. The effect of vibration on pain during local anesthesia injections. Aust Dent J. 2009;54(2):94-100.
52. Kumar PS, Leblebicioglu B. Pain control during nonsurgical periodontal therapy. Compend Contin Educ Dent. 2007;28(12):666-669.
53. Krekmanova L, Bergius M, Robertson A, et al. Everyday- and dental-pain experiences in healthy Swedish 8-19 year olds: an epidemiological study. Int J Paediatr Dent. 2009;19(6):438-447.
54. Vika M, Raadal M, Skaret E, Kvale G. Dental and medical injections: prevalence of self-reported problems among 18-yr-old subjects in Norway. Eur J Oral Sci. 2006;114(2):122-127.
55. Jacobs S, Haas DA, Meechan JG, May S. Injection pain: comparison of three mandibular block techniques and modulation by nitrous oxide-oxygen. J Am Dent Assoc. 2003;134(7):869-876.
56. Neverlien PO. Assessment of a single-item dental anxiety question. Acta Odontol Scand. 1990;48(6):365-369.
57. Corah NL. Development of a dental anxiety scale. J Dent Res. 1969;48(4):596.
58. Hakeberg M, Berggren U. Dimensions of the denta1 fear survey among patients with dental phobia. Acta Odontol Scand. 1997;55(5):314-318.
59. Heins PJ, Karpinia KA, Maruniak JW, Moorhead JE, Gibbs CH. Pain threshold values during periodontal probing: assessment of maxillary incisor and molar sites. J Periodontol. 1998;69(7):812-818.
60. Huskisson EC. Measurement of Pain. Lancet.1974;2(7889):1127-1131.