You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Dentistry is undergoing a rapidly growing technological expansion, with 3-dimensional (3D) printing processes playing a significant role. This advance has led to the integration of digital techno- logy into numerous dental treatments, including 3D-printed implant guides, periodontal surgery guides, 3D-printed partial denture frameworks, digital complete dentures, and orthodontic aligners.1-5 All of these applications have inspired an intellectual excitement that continues to expand and improve digital processes. The 3D printing industry has aided this stimulation by providing financially accessible and user-friendly materials and equipment for the production of innovative devices. One such recent innovation is the development of resins for 3D printing that offer remarkably flexible properties.6
Most 3D-printed dental devices are rigid, such as surgical guides, dental models, and removable prostheses. However, some applications, such as bite splints, require flexible devices for the comfort of the patient.7 Depending on the clinical situation and the patient's response to treatment, it is possible to deliver either a hard, soft, or dual splint.8 Unfortunately, 3D printing thus far has offered only a hard consistency for occlusal devices. To achieve soft or dual splints, 3D printing manufacturers have recommended printing the models and then fabricating the typical thermoformed splints. Recently, research and development has yielded a 3D printing resin that allows a torsion comparable to thermoformed splints.
3D Printing Processes
3D printing in dentistry involves three proc-esses: fused deposition modeling (FDM), stereolithography (SLA), and selective laser sintering (SLS). Occlusal devices are generally produced by SLA because of its high degree of accuracy and the wide selection of resins available. These resins are generally rigid due to a high modulus of elasticity. As a result, the need arose for the fabrication of flexible splints and innovative resins. Advances were made in 3D printing technologies, particularly in regard to continuous liquid interface production (CLIP) technology,9 with the key to success centered on material selection, ie, resins. Such resins must be able to deform under stress while maintaining the standard minimum requirements for occlusal devices: eg, biocompatible, wear- resistant, colorless, odorless, tasteless.
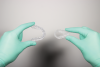
The organic phase of the resin contains metha- crylate monomers, which, after light-curing, form a stable 3-dimensional matrix. Viscosity stabilizers are needed to make these resins more flexible and less brittle. Aliphatic acrylate is the polymer of choice to create wear-resistant and flexible resins while avoiding discoloration, such as yellowing, over time.10,11 The modulus of elasticity of a flexible 3D-printed resin is approximately 115 MPa, which, on the one hand, is much lower than the 2.121 MPa of a non-flexible 3D-printed resin. On the other hand, it is close to the 175 MPa of flexible thermoforming plates. Visually, occlusal splints that are 3D-printed with flexible and non-flexible resins look identical (Figure 1); the difference in flexibility is only noticed when manually handling the splints (Figure 2). Clinically, flexible splints offer benefit to temporomandibular joint disorder patients in that they reduce muscle pain and do not cause occlusal changes, in addition to providing greater comfort than a rigid splint.12,13
Case Report
A 69-year-old male patient presented with a complaint of significant dental pain when chewing. His medical history was not relevant. Clinical examination and radiographs showed a defective restoration on vital tooth No. 3. Removal of the restoration revealed a mesiodistal crack line (Figure 3) as a result of a wedging effect provoked by the defective restoration (a fractured mesial-occlusal-distal [MOD] composite resin restoration) and amplified by a nocturnal parafunctional activity (clenching without joint derangement).
An immediate dentin sealing procedure was performed (Figure 4) and the tooth was prepared for a ceramic onlay restoration. At the subsequent appointment, a lithium-disilicate restoration was bonded to the tooth to allow a homogenous force distribution on the tooth (Figure 5). To prevent excessive wear and nocturnal parafunction, a full-contact permissive splint was indicated for the patient.
Two maxillary occlusal splints, one rigid and one flexible, without canine guidance were ordered. The goal was to give the patient the choice of both options, then have him subjectively determine which splint was the more comfortable of the two. The digital models were imported into the bite splint module of a dental software so they could be virtually mounted onto a digital articulator (Figure 6). In this clinical case, an incisal table inclination at 70 degrees and a bite opening at 3 mm were chosen. The splint was designed and adapted to the opposing arch (Figure 7).
The design of the rigid and flexible splints is essentially the same, with the only difference lying in the larger interlocks needed for the flexible splint's undercuts. In order to be sent to the 3D printer, standard tessellation language (STL) files must first be imported into a nesting software (Figure 8). The occlusal devices in this case could then be 3D-printed (Figure 9).
Once the printing process was complete, the splints were detached from the platform and soaked in a 96% isopropanol bath. To complete the curing, the splints finally were placed in a light-curing device (Figure 10). They were carefully polished and repositioned on the models to assess the occlusion and remove any occlusal interferences (Figure 11). The result was two visually identical 3D-printed splints that differed only in flexibility (Figure 12 and Figure 13).
At the next appointment, the splints were tested in the mouth (Figure 14 and Figure 15) and the patient received wear and care instructions. He was told to wear them alternately for a week each at night, and a follow-up appointment was scheduled for 2 months later.
This was the patient's first experience with an occlusal device. Wearing the rigid splint gave him the odd feeling of having a foreign object in his mouth and tight pressure on his teeth. He felt the need to systematically open his bite during sleep, which led to a dry mouth and morning halitosis. Wearing the flexible splint, however, provided significantly more comfort. He reported that even his sleep improved and he felt restful during the night.
With the successful management of his bruxism, comprehensive care was now possible to replace his missing teeth (maxillary second premolars) while preserving the existing ones, as untreated bruxism can compromise the longevity of natural teeth and implant restorations.14
Discussion
Patients often fail to recognize occlusal diseases and, as a result, seek care only when the consequences become visible and/or the condition becomes painful in its later stages. However, simply showing the patient an intraoral image that demonstrates the damage to the teeth can often be an effective way to attain patient acceptance. Occlusal devices help prevent the excessive forces exerted in patients who are bruxers and increase the lifespan of teeth and restorations. To obtain the patient's compliance in wearing a nightguard regularly, thus, requires good communication. Indeed, patients may be reluctant if they have had experience with analog splints, which traditionally were not designed with comfort in mind.
In this clinical case report, allowing the patient to wear a flexible splint enabled both prevention of the harmful consequences of bruxism as well as comfort during night usage. This flexible splint generated advantages that were not previously possible with rigid splints. Clini- cians now have the means to 3D-print either a rigid or flexible splint depending on the clinical case.
The primary concern with 3D-printed occlusal splints is typically the fit accuracy. The comparison is generally made with milling discs or thermoformed splints. The precision of 3D-printed splints is generally equal to those milled.15 However, it is necessary to take into account the horizontal orientation of the device when 3D printing15 and the offset, which should be set to 0.1 mm to obtain the optimum fit.16
Secondary concerns of 3D-printed occlusal devices are their mechanical properties and long-term stability.17,18 3D printing resins show higher water sorption and solubility compared with pressed or milled resin.17 Moreover, they have shown lower and less-consistent surface hardness values.18 However, the newer generation of resins offers improved performance in compliance with current standards by maintaining their form without visible distortion after artificial aging.17
Yet another criticism of 3D-printed devices concerns health safety. It has been observed that with acrylic splints some substances have been shown to be a potential irritant with hyper- sensitivity or even allergy to dental resins.19The dental 3D printing industry has meticulously studied the composition and production methods involved in the making of occlusal devices. The elution of 3D printing resins can release potentially cytotoxic residues,20 but this is generally a result of incomplete polymerization.21 Manufacturers insist on strict observance of the post-processing steps and recommend post-exposure with a light-curing device. This intensive light radiation improves the material curing, reduces the remaining monomers, and increases the mechanical properties.21
Conclusion
The flexible 3D printing resin demonstrated in this case report was already an innovation in itself, but making it into a medical device is an even greater accomplishment. As shown, the deleterious effects of bruxism can now be counteracted to improve the longevity of restorations and tooth structure while enabling increased patient comfort. The digital splint design allows advantages such as high accuracy, fast production, and even simplified reordering. With a flexible 3D printing resin, practitioners can provide patients a comfortable splint to help increase compliance.
In this case report, the patient tried two different 3D-printed splints to assess for himself the advantages and disadvantages of each. This simple, non-invasive treatment was helpful in obtaining patient acceptance. A comprehensive rehabilitation can now be considered to restore biological, functional, and oral esthetics for this patient.
Acknowledgment
The author thanks Matthias Mehring, PhD, and his team at VOCO GmbH for intellectual and material support.
About the Author
Yassine Harichane, DDS, MSc, PhD
Private Practice, Les Sables d'Olonne, France
Queries to the author regarding this course may be submitted to authorqueries@broadcastmed.com.
References
1. Kim T, Lee S, Kim GB, et al. Accuracy of a simplified 3D-printed implant surgical guide. J Prosthet Dent. 2020;124(2):195-201.e2.
2. Deliberador TM, Weiss SG, Neto AT, et al. Guided periodontal surgery: association of digital workflow and piezosurgery for the correction of a gummy smile. Case Rep Dent. 2020;2020:7923842.
3. Tasaka A, Shimizu T, Kato Y, et al. Accuracy of removable partial denture framework fabricated by casting with a 3D printed pattern and selective laser sintering. J Prosthodont Res. 2020;64(2): 224-230.
4. Anadioti E, Musharbash L, Blatz MB, et al. 3D printed complete removable dental prostheses: a narrative review. BMC Oral Health. 2020;20(1):343.
5. Jindal P, Juneja M, Siena FL, et al. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am J Orthod Dentofacial Orthop. 2019;156(5):694-701.
6. Bae JH, Won JC, Lim WB, et al. Highly flexible and photo-activating acryl-polyurethane for 3D steric architectures. Polymers (Basel). 2021;13(6):844.
7. Piedra-Cascon W, Sadeghpour M, Att W, Revilla-Leon M. A vat-polymerized 3-dimensionally printed dual-material occlusal device: a dental technique. J Prosthet Dent. 2021;126(3):271-275.
8. Okeson JP. The effects of hard and soft occlusal splints on nocturnal bruxism. J Am Dent Assoc. 1987;114(6):788-791.
9. Tumbleston JR, Shirvanyants D, Ermoshkin N, et al. Additive manufacturing. Continuous liquid interface production of 3D objects. Science. 2015;347(6228):1349-1352.
10. Lee BH, Choi JH, Kim HJ. Coating perform- ance and characteristics for UV-curable aliphatic urethane acrylate coatings containing Noorish type I photoinitiators. J Coat Technol Res. 2006;3(3): 221-229.
11. Ping T, Zhou Y, He Y et al. Preparation and characterization of yellowing resistance and low volume shrinkage of fluorinated polysiloxane urethane acrylate. Prog Org Coat. 2016;97:74-81.
12. Seifeldin SA, Elhayes KA. Soft versus hard occlusal splint therapy in the management of temporomandibular disorders (TMDs). Saudi Dent J. 2015;27(4):208-214.
13. Wright E, Anderson G, Schulte J. A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J Orofac Pain. 1995;9(2):192-199.
14. Zhou Y, Gao J, Luo L, Wang Y. Does bruxism contribute to dental implant failure? A systematic review and meta-analysis. Clin Implant Dent Relat Res. 2016;18(2):410-420.
15. Marcel R, Reinhard H, Andreas K. Accuracy of CAD/CAM-fabricated bite splints: milling vs 3D printing. Clin Oral Investig. 2020;24(12):4607-4615.
16. Ye N, Wu T, Dong T, et al. Precision of 3D-printed splints with different dental model offsets. Am J Orthod Dentofacial Orthop. 2019;155(5):733-738.
17. Berli C, Thieringer FM, Sharma N, et al. Comparing the mechanical properties of pressed, milled, and 3D-printed resins for occlusal devices. J Prosthet Dent. 2020;124(6):780-786.
18. Prpic V, Slacanin I, Schauperl Z, et al. A study of the flexural strength and surface hardness of different materials and technologies for occlusal device fabrication. J Prosthet Dent. 2019;121(6):955-959.
19. Weaver RE, Goebel WM. Reactions to acrylic resin dental protheses. J Prosthet Dent. 1980;43(2):138-142.
20. Wedekind L, Güth JF, Schweiger J, et al. Elution behavior of a 3D-printed, milled and conventional resin-based occlusal splint material. Dent Mater. 2021;37(4):701-710.
21. Perea-Lowery L, Gibreel M, Vallittu P, Lassila L. Evaluation of the mechanical properties and degree of conversion of 3D printed splint material. J Mech Behav Biomed Mater. 2021;115:104254.