You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Over the last twenty years, public and private health initiatives have reviewed the extensive barriers that prevent positive patient health outcomes.1-4 Due to the complexity of chronic conditions such as diabetes, cardiovascular disease, and obesity, collaborative teams of health care providers are needed to provide comprehensive patient care.5 Limited access to care, inadequate quality of care, patient health and safety concerns, and the overall cost of health care have been key drivers for the integration of interprofessional education (IPE) and the push for collaborative practices between health care providers.3,6 Interprofessional collaboration (IPC) is defined as health care providers from different professional backgrounds working as a team to deliver comprehensive care for patients.2,7 Increased awareness and active participation in interprofessional collaboration between dental hygienists and other health care providers are key to achieving optimal patient health. Dental hygienists have expertise in oral health combined with knowledge of the oral-systemic connection and have the ability to incorporate and monitor oral and systemic outcomes within dental hygiene care plans, to achieve common goals.8
Interprofessional Education Experiences
Interprofessional education is recognized worldwide for fostering teamwork and collaboration for members of the health care team as it enables students from differing professions to learn with, from, and about each other to improve collaboration and the quality of care.2 Interprofessional experiences have been shown to significantly improve providers' attitudes and behaviors to prevent medical errors and improve patient outcomes.9,10 Common IPE methods used in dental hygiene programs include case studies, on- and off- campus clinical activities, patient simulations, service learning, standardized patients, health mentors, or a combination of methods.11 One study of dental hygiene programs revealed that IPE was taught between one to four hours per week, and often in conjunction with nursing, occupational therapy, physical therapy, and dentistry programs.11 In dental schools, IPE designs included small groups from multiple professions, engaging students, and fundamentals introducing first-year students to IPE.12 Early interprofessional learning experiences have been shown to help students establish effective and collaborative working relationships within the health care team.13
Increased knowledge from interprofessional education experiences has been shown to lead to better skills and positive attitudes towards collaboration between health care providers.13-15 Physician assistant and pharmacy students increased collaborative behaviors after a year-long interprofessional clinical case study course.16 Nurse practitioner students increased confidence in oral assessment skills after IPE activity with dental students.17 Dental hygiene and physician assistant students advanced knowledge, communication, and confidence after participating in an IPE activity centered on the oral manifestations of menopause.18 IPE experiences lead to positive interprofessional communication skills and further understanding of the roles and responsibilities of other health care professionals.19-21 James et al. found IPE between physician assistant students and audiology students led to increased awareness of roles and responsibilities, provided opportunities to reflect on the benefits of IPC, and fostered interprofessional relationships.22 Dental, medical, and nursing students highlighted an increased knowledge of oral health from an IPE experience promoting teamwork, communication, and role and responsibility recognition.23 Interestingly, while both American and Canadian researchers found confidence and perceptions towards collaboration are increased by IPE, the findings on the long-term benefits of educational experiences have been inconclusive.24,25
Collaborative educational experiences are enhanced through exploration of the link between oral health and systemic disease. The 2000 Surgeon General's Report on Oral Health stresses the importance of all health care providers evaluating oral health as an indicator of overall well-being.1 The framework of the oral-systemic link serves to increase health care providers' comprehension of the roles and responsibilities within a health care team and enhances communication between providers.19,26 However, the curricula of non-dental health professionals does not adequately address oral conditions.1,17 Oral health care providers must work in conjunction with the patient and other health care professionals to reach the goal of improving oral health.
Interprofessional Collaboration in Practice
Effective collaborative health care teams, including dental hygienists, recognize members' roles and responsibilities within the group while respecting the specific support each profession provides in treating the patient.27,28 In a study of oral health awareness among nephrology nurses, it was discovered that nurses lacked knowledge of the effects of oral health on kidney disease.29 Munz et al. found while medical students are aware of oral conditions, they lack the necessary skills to diagnose oral diseases and furthermore exhibit an overall lack of interest in oral care.15 In contrast, in a study by Luebbers et al., physicians recognized the value of the oral-systemic link and collaboration with dental hygienists as part of an interprofessional team.30 Kanji and Laronde found that dental hygienists collaborate most frequently with general dentists, dental specialists, physicians, pharmacists, and nurses.31 Internationally, a German study showed that collaboration between medical and nursing students contributed to improved clinical outcomes of patients.32 Collaboration between health care disciplines has also been shown to highlight missed treatment opportunities and increase referrals between providers.30,33 Collaborative clinical practices such as daily briefings, case presentations, and continuing education courses can result in better communication between providers and improved health for high-risk patients.34
Historically, health care professionals were taught and later practiced in silos - clusters of professionals in isolated groups within their institutions. This seclusion creates a health care system which provides care for patients in a poorly organized and complex manner.3 Over the last twenty years, multiple organizations have attempted to address this poor organization with IPE and collaborative practice recommendations.1,2,6,7 Dental hygienists are in a unique position to detect a multitude of oral and systemic diseases, contact necessary health care providers to communicate the health needs of the patient, and participate in creating a custom care plan as part of a collaborative team.1
The National Dental Hygiene Research Agenda of the American Dental Hygienists' Association has prioritized research on the ways IPE and collaboration are understood and carried out within the profession.35 Changes made to include interprofessional education in the dental hygiene education curricula can be complex.36,37 Investigating the ways IPE experiences influence the way clinical dental hygienists collaborate may lead to more effective teaching methods and improve collaborative efforts between health care professionals. The purpose of this study was to assess dental hygienists' attitudes towards IPE experiences and investigate how these experiences influenced collaboration with other health care professionals.
Methods
Survey instrument
The University of Bridgeport Institutional Review Board (IRB) approved this study and granted permission to send the survey electronically. A mixed-method approach using both qualitative and quantitative data was employed. Responses were based on the participants' perceptions; therefore, a blended approach was used to decrease response bias. The 23-item survey instrument included demographics, present collaborative behaviors, and IPE experiences. There were two open-ended items, two fill-in-the-blanks, six Likert-style questions and thirteen multiple-choice questions. Three of the Likert- style items were from the Readiness for Interprofessional Learning Scale (RIPLS) and were chosen to specifically address the hypothesis.38 The RIPLS was developed by Parsell and Bligh and has been used as a measuring tool to assess participants' attitudes towards interprofessional learning.18,26,39 However, IPE assessment scales been shown to have a range of questionable psychometric integrity.40-42 Due to the fallibility of the assessment tool, the RIPLS was modified. Four subject matter experts in research and IPE pilot-tested the modified RIPLS for functionality and clarity of the questions. Feedback was incorporated into the survey design prior to distribution. Qualitative questions allowed participants to further elaborate on feelings and knowledge towards IPE and IPC and verified the quantitative data. The survey instrument avoided evaluating IPE curricula, and prior IPE experiences were not part of the inclusion criteria.
Sample population and data collection
Dental hygienists licensed in the United States (US) were recruited to participate from social media sites and constituent websites of the American Dental Hygienists' Association (ADHA). Health care professionals outside of dental hygiene and dental hygiene students were excluded from participation. Forty-nine states and the District of Columbia received an independent request to distribute the survey link, and five states complied. Members of the ADHA were emailed a letter of introduction and an invitation to participate. Sixty-seven dental hygiene related Facebook groups were contacted and agreed to distribute the survey through group posts. Consent to participate was implied when the participants opted into the survey. An electronic survey platform (SurveyMonkey; San Mateo, CA) was used to collect data. To protect privacy, date of response and IP address were removed when exporting data.
Statistical analysis
Descriptive statistics were used to determine means, frequencies of responses, and ranges of responses from demographics, years of practice, and type of employment. A 2-sample t-test yielding p-value for inference determined the association between the attitudes and behaviors towards IPE and presence of IPE experiences. Non-parametric statistics Mann-Whitney U test evaluated the attitudes towards IPC against the presence or absence of IPE experiences. A Chi-square test evaluated the correlation between the number of IPE experiences with participants' IPC behaviors within the last six months.
A content analysis was conducted on the qualitative data derived from the open-ended response items. Two researchers reviewed the data and identified common themes. After agreement was reached on the response themes, two alternate researchers independently reviewed and confirmed the findings to increase interrater reliability. Inconsistencies were resolved by majority vote between the five researchers. Themes were coded and frequency of occurrences were calculated.
Results
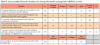
A total of 184 participants completed the survey. However, 19 respondents did not meet the inclusion criteria and were excluded from the data analysis for a sample of 165 licensed dental hygienists (n=165). A power analysis was conducted on the sample, and yielded a power of 90% (a=0.05). The majority of participants were employed in private practice settings (84.0%, n=137) and had graduated from a two-year program (76.0%, n=125). Half of the respondents came from the Northeastern US (n=83) and had between 16-25 years of clinical experience (n=81). Sample demographics are shown in Table I.
Of the 56 respondents who reported IPE experience, two-thirds agreed or strongly agreed (66%, n= 37) that the IPE provided the necessary confidence to collaborate in a professional setting. Sixty-one percent (n=97) of all respondents felt communication skills with patients and other professionals were increased with IPE experiences regardless of whether they had IPE experiences while in school. Interprofessional education experiences and IPC behaviors are shown in Figure 1.
Participants were asked to identify types of IPE activities they had experienced from a given list. The most common experiences were case studies (n= 80), on- and off- clinical rotations (n=70), patient simulations (n=37), and service-learning activities (n=37). One third of the respondents (34%, n=56) reported learning alongside students in other health professions during their education. Respondents who experienced interprofessional learning activities valued IPE more than respondents who had no previous exposure to interprofessional education (p<0.001). No association was found between the number of inter-professional education experiences and presence of collaborative behaviors within a six-month period (X2=3.567, p=0.468). Similarly, the Mann-Whitney U test did not identify significant differences between respondents' attitudes towards IPC and the presence or absence of IPE experiences (p=0.16). Relative frequency of IPE experiences was highest in the 0-5 (54%, n=19), 6-10 (42%, n=10), and 16-20 (42%, n=5) years of practice groups, respectively.
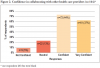
Participants' attitudes towards interprofessional collaboration adapted from the RIPLS scale38 are shown in Table II. Most respondents (90.0%, n=147) indicated that they believed collaboration between dental hygienists and other health care professionals was important. Over half of the participants (52%, n=85) strongly agreed providing collaborative care makes the dental hygienist a more effective team member in overall patient care, and two thirds of participants (63%, n=105) strongly agreed that patients would ultimately benefit if dental hygienists and health care professionals worked together. Most respondents (82%, n= 133) felt confident or very confident in collaborating with other health care professionals as shown in Figure 2. The relative frequency of collaborative encounters with other health care professionals was highest among participants who have been working for 11-15 years (80% ,n=13), followed by those who have worked for 6-10 years (70%, n=16) and those who worked for more than 25 years (63%, n=38).
Linear regression correlation revealed a significant relationship between respondents' IPC attitudes and corresponding IPE attitudes (t=3.922, p<0.001). Participants who had positive attitudes towards IPE also showed positive attitudes towards IPC (r=0.301). Fewer than ten percent of the observed variation of collaborative attitudes were explained by the relationship between IPC and IPE attitudes, suggesting attitudes towards IPC were largely related to variables other than attitudes related to IPE experiences (r2= 0.091). Data was then limited to respondents with previous IPE experience to further analyze the correlation between attitudes of these experiences and the frequency of IPC within a six-month period. IPE attitude scores of respondents who had previous IPE experiences showed a positive but weak correlation to the number of IPCs with other health care professionals within a six-month period (r=0.172, r2=0.03).
Measurements of IPC showed over one half of respondents (63%, n= 102) had collaborated with one or more health care professionals within the last six months; four times per month was the average frequency of collaboration. Frequency of collaborations were also analyzed in relation to the presence of IPE experiences. Respondents with IPE experiences tended to collaborate more on average (median 3.75) than respondents without IPE experiences. Participants who indicated a lack of IPC activities were asked to choose from a list of reasons for not collaborating with other health care professionals. Reasons cited as barriers to IPC included a "lack of need" (n=26), "lack of time" (n=13), and "not in the job description/not allowed" (n=7).
There were 133 responses to the open-ended question, "What is the most important factor for a dental hygienist to practice IPC?" Over one third of the respondents (37.0%, n=49) focused on patient care and better health outcomes as the most important factor for IPC. One participant mentioned confidence, communication, and patient care were particularly significant.
"To feel confident about my own knowledge concerning oral health and be able to communicate information to another health care professional concerning patient care situations in search of optimal patient health outcomes."
Respondents also mentioned respect (n=13) as a health care provider and the role of IPE as critical factors.
"For the dental hygiene profession to promote the strength of their education/knowledge so that they will be respected as serious health care providers. Furthermore, for dental hygiene programs to create more collaborations between their students and other medical professions' students so that they can understand the benefit of that collaboration."
Regarding the skills gained from previous IPE experiences, the value of collaboration and teamwork were recurring themes.
"Understanding each professional disciplines' unique specialized contribution to the overall positive patient outcome."
"I gained an understanding of what my role was, and what questions to ask the other students from different health care backgrounds. Knowing more about how oral health affects the overall health of patients helps me daily."
Discussion
Findings from this study revealed that most dental hygienists surveyed were enthusiastic about collaborating with other health care professionals to provide comprehensive patient care. Data revealed more than half of the participants already collaborate with other health care professionals, regardless of a history of formal interprofessional education experiences. Most respondents indicated confidence in collaborating with other health care professionals, suggesting that dental hygienists recognize the immense value of collaborative teams of professionals and act based on those attitudes, independent of formal training.
A closer look at IPE teaching methodologies could expand on the qualities important to collaboration such as knowledge, values, communication skills, and resources. Since 2009, the Interprofessional Education Collaborative (IPEC) has focused on creating competencies to guide collaborative education experiences with a focus on engaging students of different health professions. The Interprofessional Education Collaborative divides collaborative practice into four domains used to assess effectiveness of IPE activities and foster health care teams, enhancing patient care and improving population health.7 More than half of dental hygiene schools in the US have indicated offering a form of IPE that meets the current accreditation standards.37 However, a survey of dental hygiene program directors showed that one quarter of dental hygiene programs in the US failed to incorporate interprofessional activities in the curricula.11 In addition, the IPE activities included in curricula may not meet the definition of IPE created by the IPEC.7,12 Students may not understand the value of interprofessional collaboration if the education received does not align with the IPEC competency model. Results from this study showed that two thirds of participants who had collaborated with other health care providers at a rate of five or more times within a six-month period held bachelor's degrees or higher. Further research is needed to determine a correlation between level of education and the frequency of IPC.
Participants who had experienced IPE in a collaborative setting presented higher positive attitudes towards IPE compared to those without interprofessional experiences. A significant relationship was found between respondents' IPC attitudes and corresponding IPE attitudes, suggesting as IPE attitudes increase, attitudes regarding collaboration with other health care providers increases. The statistical correlation may partially be due to greater understanding of IPE and IPC through the educational experience provided. Findings are consistent with research that noted students who experience IPE gain appreciation of roles and responsibilities in collaborative experience, teamwork, communication skills, and a greater value of collaborative efforts.11,43 However, application of linear regression as a statistical analysis provided a relatively weak way to predict IPC attitudes from the reported IPE attitudes. Approximately 9% of the observed variation of IPC attitudes is explained by the relationship to IPE attitudes. These findings suggest attitudes related to collaboration with other health care providers are largely related to variables outside of this study.
Nearly one quarter of the respondents who reported not collaborating with other health care providers indicated a lack of perceived need. Whether this lack of need means that the respondents do not value IPC as a means for improved patient outcomes or if they do not see the need to communicate with another health care provider in managing patient care is unknown. Future research could expand on this topic and further explore the correlation between IPC attitudes and patient health.
This study had limitations. While a representative sample of dental hygienists licensed in the US was sought, there were challenges. The invitation to participate that was distributed to the ADHA constituents was limited to those states who opted to forward the survey to their members. Additional participants were recruited through social media sites; however, users of social media are not representative of all demographics. While the generalizability of the results is limited, the power analysis deemed the sample size to be sufficient for statistical analysis. The modification of the RIPLS tool may have affected the validity. The retrospective nature of the survey items may be subject to self-report bias in the responses. Future research is necessary to explore the various of collaborative behaviors of dental hygienists along with previous IPE experiences.
Conclusion
Findings from this study show dental hygienists feel strongly about using IPE efforts to benefit patient health and are confident in interacting with other health care providers. While many dental hygienists were found to be collaborating with other health care professionals without formal IPE experiences, those with IPE experiences were found to collaborate at a higher frequency than those without previous IPE experiences. Promotion of the need and value of interprofessional collaboration could encourage increased collaborations between health care providers. Further research examining the best practices of interprofessional education could enrich future interactions between other health care providers and dental hygienists.
Acknowledgements
The authors would like to thank Scott Kennedy MA, EdD, professor and statistician, Fones School of Dental Hygiene, University of Bridgeport, for his assistance in the statistical analyses.
Jennifer R. Bagge, RDH, BSDH is an adjunct professor and clinical instructor at Springfield Technical Community College, Department of Dental Hygiene, Springfield, MA and a graduate of the Fones School of Dental Hygiene; Tammara C. Harbaugh, RDH, BSDH; Iris G. Tabora, RDH, BSDH; Melissa A. Aponte, RDH, BSDH; Adriana Hakobyan, RDH, CDA, BSDH are clinical dental hygienists and graduates of the Fones School of Dental Hygiene; Deborah Johnson, RDH-EA/EP, MS is an adjunct faculty member at Fones School of Dental Hygiene; all from the University of Bridgeport, Bridgeport, CT, USA.
References
1. U.S. Department of Health and Human Services. Oral health in America: a report of the surgeon general [Internet]. Rockville (MD): U.S. Department of Health and Human Services; 2000. [cited 2020 Feb 10]. Available from: hck1ocv.@www.surgeon.fullrpt.pdf
2. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva (CH): World Health Organization; 2010 [cited 2019 Mar 30]. 64 p. Available from: http://www.who.int/hrh/resources/framework_action/en/
3. Institute of Medicine (US) Committee on quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press (US); 2001. PMID: 25057539.
4. Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. Washington (DC): National Academies Press (US); 2015 Dec 15. PMID: 26803876.
5. Gilbert JH. Interprofessional learning and higher education structural barriers. J Interprof Care. 2005 May;19 Suppl 1:87-106.
6. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost, the remaining barriers to integrated care are not technical; they are political. Health Aff [Internet]. 2008;27(3):759-69.
7. Interprofessional Education Collaborative. Core competencies for interprofessional collaborative practice: 2016 update [Internet]. Washington, DC: Interprofessional Education Collaborative; 2016. [cited 2019 Oct 17]. Available from https://hsc.unm.edu/ipe/resources/ipec-2016-core-competencies.pdf
8. Theile CW, Strauss SM, Northridge ME, Birenz S. The oral health care manager in a patient-centered health facility. J Evid Based Dent Pract. 2016 Jun;16 Suppl(Suppl):34-42.
9. McGregor MR, Lanning SK, Lockeman KS. Dental and dental hygiene student perceptions of interprofessional education. J Dent Hyg. 2018 Dec 1;92(6):6-15.
10. Reeves S, Perrier L, Goldman J, et al. Interprofessional educational materials: effects on professional practice and healthcare outcomes (update). Cochrane Datab Syst Rev. 2013 Mar 28;2013(3):CD002213.
11. Tolle SL, Vernon MM, McCombs G, De Leo G. Interprofessional education in dental hygiene: attitudes, barriers and practices of program faculty. J Dent Hyg. 2019;93(2):13-22.
12. Formicola AJ, Andrieu SC, Buchanan JA, et al. Interprofessional education in U.S. and Canadian dental schools: an ADEA team study group report. J Dent Educ. 2012;76(9):1250-68.
13. Ateah CA, Snow W, Wener P, et al. Stereotyping as a barrier to collaboration: does interprofessional education make a difference? Nurse Educ Today. 2011;31(2):208-13.
14. Allen HB, Gunaldo TP, Schwartz E. Creating awareness for the social determinants of health: dental hygiene and nursing student interprofessional service-learning experiences. J Dent Hyg. 2019;93(3):22-8.
15. Munz SM, Kim RY, Holley TJ, et al. Dental hygiene, dental, and medical students' OMFS/hospital dentistry-related knowledges/skills, attitudes, and behavior: an exploration. J Dent Educ. 2017 Feb;81(2):149-61.
16. Mazur Z, Hanes SD, Kern D. Effect of a clinical case-study course on physician assistant and pharmacy students' interprofessional care competencies. J Physician Assist Educ. 2019 Dec;30(4):223-7.
17. Estes KR, Callanan D, Rai N, et al. Evaluation of an interprofessional oral health assessment activity in advanced practice nursing education. J Dent Educ. 2018 Oct;82(10):1084-90.
18. Rothmund WL, O'Kelley-Wetmore AD, Jones ML, Smith MB. Oral manifestations of menopause: an interprofessional intervention for dental hygiene and physician assistant students. J Dent Hyg. 2017;91(6):21-32.
19. Haber J, Hartnett E, Allen K, et al. The impact of oral-systemic health on advancing interprofessional education outcomes. J Dent Educ. 2017 Feb;81(2):140-8.
20. Ritchie C, Dann L, Ford P. Shared learning for oral health therapy and dental students: enhanced understanding of roles and responsibilities through interprofessional education. Eur J Dent Educ. 2013 Feb;17(1):e56-63.
21. Reddington AR, Egli AJ, Schmuck HM. Interprofessional education perceptions of dental assisting and radiologic technology students following a live patient experience. J Dent Educ. 2018 May 2;82(5):462-8.
22. James J, Chappell R, Mercante DE, Gunaldo TP. Promoting hearing health collaboration through an interprofessional education experience. Am J Audiol. 2017 Dec 12;26(4):570-5.
23. Farokhi MR, Muck A, Lozano-Pineda J, et al. Using interprofessional education to promote oral health literacy in a faculty-student collaborative practice. J Dent Educ. 2018 Oct;82(10):1091-7.
24. Curran VR, Sharpe D, Flynn K, Button P. A longitudinal study of the effect of an interprofessional education curriculum on student satisfaction and attitudes towards interprofessional teamwork and education. J Interprof Care. 2010 Jan;24(1):41-52.
25. Lapkin S, Levett-Jones T, Gilligan C. The effectiveness of interprofessional education in university-based health professional programs: a systematic review. JBI Libr Syst Rev. 2011;9(46):1917-70.
26. Nash WA, Hall LA, Lee Ridner S, et al. Evaluation of an interprofessional education program for advanced practice nursing and dental students: the oral-systemic health connection. Nurse Educ Today. 2018 Feb; 66:25-32.
27. Canadian Interprofessional Health Collaborative. A national interprofessional competency framework [Internet]. Vancouver: University of British Columbia; 2010. [cited 2020 May 03]. Available from: http://ipcontherun.ca/wp-content/uploads/2014/06/National-Framework.pdf
28. Bollen A, Harrison R, Aslani P, van Haastregt JCM. Factors influencing interprofessional collaboration between community pharmacists and general practitioners-a systematic review. Health Soc Care Community. 2019 Jul;27(4):e189-e212.
29. Blue C, Isringhausen K, Dils E. Raising oral health awareness among nephrology nurses. J Dent Hyg. Spring 2011;85(2):151-7.
30. Luebbers J, Gurenlian J, Freudenthal J. Physicians' perceptions of the role of the dental hygienist in interprofessional collaboration: a pilot study. J Interprof Care. Jan-Feb 2021;35(1):132-5. Epub 2020 Mar 4.
31. Kanji Z, Laronde DM. Career outcomes of dental hygiene baccalaureate education: a study of graduates' professional opportunities, further education, and job satisfaction. J Dent Educ. 2018 Aug;82(8):809-18.
32. Braun B, Grünewald M, Adam-Paffrath R, et al. Impact of interprofessional education for medical and nursing students on the nutritional management of in-patients. GMS J Med Educ. 2019 Mar 15;36(2):Doc11.
33. Jackson JT, Quinonez RB, Kerns AK, et al. Implementing a prenatal oral health program through interprofessional collaboration. J Dent Educ. 2015 Mar;79(3):241-8.
34. Nagelkerk J, Thompson ME, Bouthillier M, et al. Improving outcomes in adults with diabetes through an interprofessional collaborative practice program. J Interprof Care. 2018 Jan 2;32(1):4-13.
35. ADHA Council on Research. National dental hygiene research agenda. J Dent Hyg 2016 Jun;90:43-50.
36. Casa-Levine C. The value of interprofessional education: assessing the attitudes of dental hygiene administrators and faculty. J Dent Hyg. 2017 Dec;91(6):49-58.
37. Furgeson D, Inglehart M. Interprofessional education in U.S. dental hygiene programs: program director responses before and after introduction of CODA standard 2-15. J Dent Educ. 2019 Jan;83(1)5-15.
38. Parsell G, Bligh J. The development of a questionnaire to assess the readiness of health care students for interprofessional learning (RIPLS). Med Educ. 1999 Feb;33(2):95-100.
39. Evans JL, Henderson A, Johnson NW. Interprofessional learning enhances knowledge of roles but is less able to shift attitudes: a case study from dental education. Eur J Dent Educ. 2012 Nov;16(4):239-45.
40. Kerry MJ, Wang R, Bai J. Assessment of the Readiness for Interprofessional Learning Scale (RIPLS): an item response theory analysis. J Interprof Care. 2018 Sep;32(5):634-7.
41. Oates M, Davidson, M. A critical appraisal of instruments to measure outcomes of interprofessional education. J Interprof Care. 2015 Apr;49:386-98.
42. Schmitz CC, Brandt BF. The Readiness for Interprofessional Learning Scale: to RIPLS or not to RIPLS? That is only part of the question. J Interprof Care. 2015 Dec; 29:6, 525-6.
43. Singer Z, Fung K, Lillie E, et al. Interprofessional education day-an evaluation of an introductory experience for first-year students. J Interprof Care. 2018 May;32(3):399-402.