You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
It can be challenging for most elderly nursing home residents to implement oral health care independently due to chronic disease, disabilities, or decreased cognitive function and assistance in performing activities of daily living are often required.1 Poor oral health can lead to oral diseases, which can decrease quality of life (QOL) and increase mortality risk.2 Moreover, the elderly, particularly those in nursing facilities, often have chronic illnesses requiring medications with adverse oral side effects, such as xerostomia.3 While regular oral health care is critical to maintain the QOL of the elderly in nursing homes, it often receives a low intervention priority.4
The lack of onsite dental clinics at Korean nursing homes is a barrier to dental care for elderly residents living in such facilities.5 Residents with oral health problems must visit the local clinic with the help of the nursing home staff, which can pose challenges. To address this access to care issue, the Korean government reformed the regulations to include dentists in the definition of "part-time visiting doctors" providing medical services in geriatric care facilities. However, general doctors and dentists are commissioned by the individual geriatric care facilities. Many of these facilities have chosen to extend their contract with the general medical practitioners who have been visiting the facility, rather than employ part-time visiting dentists. Hence, the oral health care of elderly residents is mostly managed by the institutional caregivers.
Caregivers often regard oral care provision for the residents as a minimal part of their overall work.6 Even when the caregiver is committed to the care of these individuals, proper oral health care provision is hindered by the caregiver's lack of professional education and training in geriatric oral health care.7 A recent qualitative study of caregivers revealed that methods and level of oral care provision for elderly residents varied across facilities, depending on the level of commitment of the facility head.8 Choi emphasized the need for an oral health intervention program run by oral health professionals within the facility in order to provide quality dental service.9
Most previous research on geriatric oral health care in nursing homes has targeted caregivers nursing the elderly.10-12 Some studies have utilized professional oral health care providers, but varied in terms of the method of care, intervention duration, and measurement index used.13,14 Lee et al.15 developed a one-week interval professional oral health care program based on the previous studies.13,14 Their findings demonstrated that elderly residents' oral health status improved based on the intervention duration (4 weeks and 12 weeks). However, the study failed to consider the effect of the intervention interval, as only a one-week interval was used, which is challenging at the practical level within in the context of almost non-existent professional oral health care.16
The purpose of this study was to investigate the effects of implementing a professional oral health care program at different intervals, one week or two weeks, on the oral health status and salivary flow rate (SFR) of the elderly living in nursing care facilities.
Methods
Sample population
The target population was elderly persons aged ≥ 65 years residing in nursing homes in the Gyeonggi and Chungcheong Provinces in the Republic of Korea. Nursing homes were selected through convenience sampling, and informed consent was obtained. Each participant was assigned to either a one-week interval group, two-week interval group, or control group; participants were either bed-ridden patients with complete dependence in activities of daily living (ADL) or demonstrated partial dependence in ADL. Inclusion criteria were individuals who had not received any dental care within the past 6 months. Individuals who refused to open their mouth due to severe cognitive impairment, those with Sjögren's syndrome, or those who were on salivation stimulation medication were excluded from the study.
A power analysis was performed to determine the minimum sample size required for the t-test and was calculated using G*Power 3.1 for Windows. For a significance level of 0.05, effect size of 0.5, and power of 0.85, at least 38 subjects per group were required, however, considering drop-out, 135 participants (45 per group) was set as the sample size. Shinhan University Institutional Review Board approved the study. Additionally, informed consent from all participants was obtained following the explanation of the study objective and method of participation. In cases of elderly patients with communication difficulties, consent from guardians was received.
To test for homogeneity of the group participants, data on general characteristics, long-term care insurance (LTCI) level, length of stay (LOS), cognitive function, ADL performance, and general health- and oral health-related characteristics were collected via a questionnaire. Initial information regarding gender, age, education level, and participant-partner living arrangement was received prior to starting the questionnaire. The Korean version of Mini-Mental State Examination (MMSE-K)17 was used to measure cognitive function. ADL performance was assessed using the modified Barthel index, which had been revised to reflect Korean culture and standardized by Jeong et al.18 Data were collected on the following categories: number of chronic illnesses, number of current medications, recent bouts of pneumonia, daily oral care, refusal of oral care, and xerostomia. General characteristics and cognitive function were asked directly to residents and answers were recorded accordingly. Activities of daily living performance and general health- and oral health-related characteristics were assessed by the nursing staff, social worker, or caregiver.
Intervention
The professional oral health care program was implemented for 12 weeks; at one-week intervals in the one-week interval group, and at two-week intervals in the two-week interval group. In the control group, no professional oral health care program was implemented. The intervention was designed based on the research method used previously by Lee et al.,15 and was further modified and supplemented through expert consultation with a dentist, two dental hygiene professors, and two clinical dental hygienists. Professional oral care was performed by four dental hygienists and lasted about six minutes per participant. To avoid any experimenter bias, the study participants were randomly assigned to the same dental hygienist each time. Dental hygienists were blinded to group selection.
The professional oral health care intervention was carried out according to the following procedures. The lip area was first cleaned with gauze soaked in a disinfectant mixture of saline and mouth rinse (Listerine, McNeil Consumer Healthcare; Fort Washington, PA, USA). Vaseline Petroleum jelly was then applied to the lips. For participants with dentures, each denture was removed and cleaned of debris via a suction device. The teeth and tongue were cleaned using a combination of rolling brushing, Watanabe brushing, and Bass brushing methods. Interdental brushes were used to clean the interproximal areas in the posterior region. The participant was then asked to rinse with water. If the participant had difficulty with rinsing, a suction device was used to remove the water. After removing debris in the oral cavity, the tongue was wiped using a sponge brush soaked in chlorhexidine and squeezed to remove excess. A moisturizer was then applied. The buccal mucosa was massaged using either the handle of a toothbrush or a finger, the upper/lower lips were stretched outwards for five seconds for each of three cycles, and the buccal and lingual gingivae were massaged using the thumb and index finger. Areas of the parotid, submandibular, and sublingual glands were massaged ten times each. Each participant was provided with an interdental brush and a sponge brush, which were replaced once every two months and at each visit, respectively. Patients wearing dentures were provided with denture cleansers.
Outcome measures
The oral health status pre- and post-intervention was examined to evaluate the effects of the professional oral healthcare program. The O'Leary index,19 Winkel Tongue Coating Index,20 Löe & Silness gingival index,21 and salivary flow rate (SFR),22 were measured. Additionally, an oral examination was performed by a single dentist and post-intervention oral health status was assessed in all groups, three days after program termination.
The O'Leary index19 is a quantitative measurement of individual oral status. Disclosing agent was applied to all teeth. Each tooth was first divided into four surfaces (mesial, distal, buccal, lingual) and the coloring on each surface was recorded as a score of 0 for "No plaque" or 1 for "With plaque," indicating poorer hygiene control. The occlusal and incisal surfaces and any missing teeth were excluded from measurement.
Tongue coating was evaluated using the Winkel Tongue Coating Index (WTCI).20 With the patient's mouth wide open, the tongue was divided into six sections, two vertical sections from tip to base and three horizontal sections. Tongue coating for each section was rated as 0 for "No coating," 1 for "Light coating," or 2 for "Heavy coating." The sum of these scores (range: 0-12) indicated the total amount of coating.
The Löe & Silness gingival index21 is widely used for measuring the level of periodontal disease by examining four sections (mesial, distal, buccal, lingual) of the gingival margin. For each section, the level of inflammation was evaluated as 0 for "No inflammation," 1 for "Mild inflammation with slight changes in color and edema, but no bleeding on probing," 2 for "Moderate inflammation with redness, edema, and bleeding on probing," and 3 for "Severe inflammation with redness, hyperplasia, and spontaneous bleeding." The total sum of the scores was then divided by the total number of gingival margins examined, with 0 indicating healthy gingiva.
Salivary flow rate was measured using the swab method.22 Without having brushed their teeth for two hours following breakfast, participants were asked to swallow to void the mouth of saliva prior to measurement. Dental cotton rolls were placed in the mouth (1.3 x 3.2 cm, Richmond Dental Company; Charlotte, NC, USA): one under the ventral surface (sublingual salivary gland) and one each in the left and right maxillary buccal regions (submandibular salivary glands). After five minutes without any movement, the cotton rolls were removed and their weight was measured using a CB Series (CB-200) digital scale with a resolution of 0.01 g (A&D Co., Ltd., Jinchoen, Korea).
Data analysis
Data was analyzed using SPSS Statistics software (version 22.0, IBM Corporation, Armonk, NY, USA) and the significance level was set to 0.05. A chi-square test was conducted for categorical variables, For continuous variables, one-way analysis of variance (ANOVA) with Scheffe's post-hoc test was performed. Analysis of covariance (ANCOVA) was conducted to compare post-intervention-measured values between groups. However, SFR was not identified as a significant interaction term for ANCOVA. Therefore, the homogeneity of pre-intervention measurement values was first verified. Then, inter-group comparison of post-intervention measurements was then performed using one-way ANOVA. To identify pre-to-post changes, a paired t-test was performed.
Results
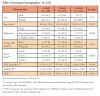
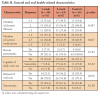
Evaluation of the general characteristics, LTCI level, LOS, cognitive function, and ADL performance revealed that all variables except for cognitive function were not significantly different among the groups (Table I). No general health or oral health-related characteristics differed significantly among the groups, confirming their homogeneity (Table II). The one-week interval group and the control group mostly had two illnesses; all three groups typically used one to three medications. Most had no recent history of pneumonia, performed daily oral care, did not refuse oral care, or reported having xerostomia.
The results of the paired t-tests comparing the effects of the professional oral care program are displayed in Table III. After intervention, the O'Leary index decreased by 0.90 and by 0.47 in the one week and two-week interval groups, respectively (p < 0.001). There was no statistically significant change in the control group. The Winkel Tongue Coating Index decreased by 3.81 post-intervention in the one-week interval group (p < 0.001), but there was no significant change in the two-week interval or control groups.
The Löe & Silness gingival index decreased post-intervention by 2.18 and 1.09 in the one-week and two-week interval groups, respectively (p < 0.05), with no significant change in the control group. The SFR increased post-intervention by 0.42 and 0.26 in the one-week and two-week interval groups, respectively (p < 0.05), and decreased by 0.08 in the control group (p < 0.05).
The plaque index, gingival index, and tongue coating index decreased most significantly in the one-week interval group, followed by the two-week interval and lastly the control groups; while SFR increased most significantly in the one-week interval group, followed by the two-week interval group (p < 0.001).
Discussion
This study aimed to assess the effects of an oral health care intervention program on the oral health status and salivary flow of elderly residents living in a long-term care facility. Prior to the intervention, homogeneity across the one-week and two-week interval groups, as well as the control group, was confirmed; only cognitive function differed between the groups. Elderly residents in long-term care facilities frequently have difficulty performing oral care independently as a result of impaired cognition, mobility, or hand joint micromotion and are generally at high risk for oral diseases.23 Patients with impaired cognitive function tend to forget about personal oral health care, display resistant behavior to oral care performed by nursing staff, and have difficulty expressing oral pain or discomfort, if present.24 Although participants' cognitive function differed significantly across groups, the MMSE-K score was < 19 (dementia) in all groups, indicating general impairment. Moreover, the ADL score was 25-49 in all groups, indicating maximum dependence.18 Since most of the participants required assistance, this study concluded that there was no problem with the homogeneity between groups.
Pre- and post-evaluation revealed that plaque levels significantly decreased post-intervention in both of the intervention groups, consistent with previous findings.15 According to recent studies, oral health care is critical to preventing aspiration pneumonia in the elderly and oral function maintenance, muscle strength recovery, and mental health.16,25 The present study demonstrated the effect of using a combination of various brushing methods to clean the tooth surface and an interdental brush to wipe the interdental and posterior surfaces.
Elderly residents of nursing care homes can suffer hyposalivation due to adverse effects of multiple medications and the resultant increase in tongue coating can lead to increased risk of malodor, caries, periodontal disease, and fungal infections (e.g., oral candidiasis).26 A sponge brush containing chlor-hexidine was used to wipe the oral mucosa and tongue followed by the application of moisturizer. Tongue coating significantly decreased in the one-week interval group, which was consistent with a previous study.15 Tongue coating decreased slightly in the two-week interval group, but not significantly. Reduction effects on tongue coating can vary depending on the intervention interval.
The gingival index score also significantly decreased post-intervention in both intervention groups. According to Matthews et al.,27 66-74% of elderly residents in nursing homes have comorbid gingivitis and 32-49% require treatment for periodontal disease, a known risk factor of cardiovascular disease.28 Efforts to prevent progression from gingivitis to periodontitis is necessary. The reduction of gingivitis and improvement of periodontal condition through oral hygiene care were confirmed in this study.
Salivary gland hypofunction disrupts the normal homeostasis of the oral cavity, contributing to a range of oral diseases including dental caries, taste disturbances, candidiasis, and difficulties with swallowing, chewing, and speaking.29 Ohara et al. reported that oral health care, facial and tongue muscle exercises, and salivary gland massage can increase salivation in elderly patients with xerostomia.30 This study demonstrated that SFR significantly increased in both experimental groups after massaging the salivary glands and oral muscles, with a greater effect observed in the one-week interval group. This finding has important implications for stimulating salivary function.
Across all measurement indices, the effects were two-fold greater in the one-week versus two-week interval group, which confirms that a shorter intervention interval more markedly improves the oral health status and SFR in the elderly, which has implications for the implementation of a professional oral health care program. However, this study only lasted 12 weeks, and as such, does not reflect the results of continued care. Future studies should evaluate the effects of implementing the program over a longer time frame. Limitations of this study include the small sample size and the possible inaccuracy of participant information related to general and oral health-related characteristics as obtained from the nursing staff responsible for the elderly resident. Future research should aim to enhance the sample both in size and representativeness.
Conclusion
Results from this study demonstrated that the implementation of a professional oral health care program enhances the oral health and salivation in the elderly. Accordingly, oral health professionals, dentists, and dental hygienists, should monitor and manage oral health of the elderly in long-term care facilities. Relevant guidelines for institutions need to be established requiring daily oral hygiene care and regular dental care to elderly residents in nursing homes.
Disclosure
This study was supported by a National Research Foundation of Korea grant funded by the Korean government (Ministry of Science and ICT; No. 2018R1A2B6006701). The funders had no role in the study design, data collection and analysis, or preparation of the manuscript.
Kyeong Hee Lee, RDH, PhD, is an associate professor, Department of Dental Hygiene, College of Bioecological Health, Shinhan University, Republic of Korea; Keun Yoo Lee, RDH, PhD, is a medical consultation team leader, Asan-si Public Health Center, Republic of Korea; Yoon Young Choi, DDS, PhD, is a research professor, Artificial Intelligence Big Data Medical Center, Yonsei University Wonju College of Medicine, Republic of Korea; Eun Seo Jung, RDH, PhD, is an adjunct professor, Department of Dental Hygiene, College of Bioecological Health, Shinhan University, Republic of Korea. Corresponding author: Eun Seo Jung, RDH, PhD; dentalmien@hanmail.net
References
1. Sung, K. Predictive factors associated with death of elderly in nursing homes. Asian Nurs Res. 2014 Jun;8:143-9.
2. Zenthöfer A, Rammelsberg P, Cabrera T, et al. Determinants of oral health-related quality of life of the institutionalized elderly. Psychogeriatrics. 2014 Dec;14:247-54.
3. Tanigawa T, Yamashita J, Sato T, et al. Efficacy and safety of pilocarpine mouthwash in elderly patients with xerostomia. Spec Care Dentist. 2015 Feb;35:164-9.
4. Kwak JS, Woo SH, Lee JR. Recognition towards oral health care and plaque removal in the elderly people. J Korean Soc Dent Hyg. 2015 Aug;15:727-33.
5. Ko SM, Lim SR. Oral hygiene care for elderly in care facility. J Korean Dent Assoc. 2015 Oct;53:678-87.
6. Joen HS, Han SY, Chung WG, et al. Knowledge, attitude and behavior status on oral health care of geriatric care workers in long-term care facilities. J Dent Hyg Sci. 2015 Oct;15:569-76.
7. Kim GH, Kwon YS. A study on oral health perception and oral health-related quality of life of the elderly patients in a geriatric hospital. J Korean Soc Dent Hyg. 2016 Jun;16:363-71.
8. Jung ES, Choi YY, Lee KH. A qualitative study on the present conditions and problems of oral health care in senile dementia patients. J Korean Soc Dent Hyg. 2019 Aug;19:601-14.
9. Choi JS. Oral health status of long-term care facility residents. J Korean Soc Dent Hyg. 2017 Jun;17:527-37.
10. Hoben M, Hu H, Xiong T, et al. Barriers and facilitators in providing oral health care to nursing home residents, from the perspective of care aides-a systematic review protocol. Syst Rev. 2016 Apr;7:53.
11. Kim KM, Park YN, Lee MK, et al. Oral health knowledge level on oral care and elder oral hygiene care of the nursing home staff in long-term care facilities. J Korean Soc Dent Hyg. 2014 Oct;14:723-30.
12. Baek JH, Lee HJ, Choi HJ, et al. Content analysis of daily tooth cleaning service records by caregivers in a long-term care facility. J Korean Soc Dent Hyg. 2014 Dec;14:903-13.
13. Choi SM. The effects of professional oral health care on oral health states of long-term care patients in geriatric hospital [dissertation]. Gyeongsan: Yeungnam University; 2012.
14. Jeon YJ, Choi JS, Han SJ. The effect of dry mouth improvement by oral exercise program in elderly people. J Korean Soc Dent Hyg. 2012 Apr;12:293-305.
15. Lee KY, Lim SR. Effect of professional oral healthcare program on the oral status of elderly residents in long-term care facilities. J Dent Hyg Sci. 2016 Dec;16:432-41.
16. So JS. A study on the amendments of long-term care-related legislations for the introduction of part-time facility dentists. J Korean Dent Assoc. 2015 Oct;53:696-704.
17. Park JH, Kwon YC. Standardization of Korean version of mini-mental state examination (MMSE-K) for use in the elderly. Part II. Diagnostic validity. J Korean Neuropsychiatr Assoc. 1989 Mar;28:508-13.
18. Jeong HY, Park BG, Shin HS, et al. Development of the Korean version of modified Barthel index (K-MBI): Multi-center study for subjects with stroke. Ann Rehabil Med. 2007;31:283-97.
19. O'Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972 Jan;43:38.
20. Winkel EG, Roldán S, Van Winkelhoff A, et al. Clinical effects of a new mouth rinse containing chlorhexidine, cetylpyridunium chloride and zinc-lactate on oral halitosis. A dual-center, double-blind placebo-controlled study. J Clin Periodontol. 2003 Apr;30:300-6.
21. Löe H, Silness J. Periodontal disease in pregnancy I. Prevalence and Severity. Acta Odontol Scand. 1963 Dec;21:533-51.
22. Navazesh M, Christensen CM. A comparison of whole mouth resting and stimulated salivary measurement procedures. J Dent Res. 1982 Oct;61:1158-62.
23. Vanobbergen JN, De Visschere LM. Factors contributing to the variation in oral hygiene practices and facilities in long-term care institutions for the elderly. Community Dent Health. 2005 Dec;22:260-5.
24. Zuluaga DJ, Ferreira J, Montoya JA, Willumsen T. Oral health in institutionalised elderly people in Oslo, Norway and its relationship with dependence and cognitive impairment. Gerodontology. 2012 Jun;29:e420-6.
25. Shi Z, Xie H, Wang P, et al. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2013 Aug;8:CD008367.
26. Benn AM, Thomson WM. Saliva: an overview. N Z Dent J. 2014 Sep;110:92-6.
27. Matthews DC, Clovis JB, Brillant M, et al. Oral health status of long-term care residents: A vulnerable population. J Can Dent Assoc. 2012;78:c3.
28. Liccardo D, Cannavo A, Spagnuolo G, et al. Periodontal disease: a risk factor for diabetes and cardiovascular disease. Int J Mol Sci. 2019 Mar;20:E1414.
29. Villa A, Wolff A, Aframian D, et al. World Workshop on Oral Medicine VI: a systematic review of medication-induced salivary gland dysfunction: prevalence, diagnosis, and treatment. Clin Oral Investig. 2015 May;19:1563-80.
30. Ohara Y, Yoshida N, Kono Y, et al. Effectiveness of an oral health educational program on community-dwelling older people with xerostomia. Geriatr Gerontol Int. 2015 Apr;15:481-9.