You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
In 1948, the World Health Organization redefined the term "health" to incorporate aspects of physical, mental, and social well-being.1 Physical well-being encompasses an individual's ability to perform everyday activities. Mental well-being suggests that an individual acknowledges their ability to manage stressors, anxieties, and undesirable emotions. Social well-being acknowledges an individual's capability to be involved in society and their connections with others.1 This expanded definition acknowledged health as a more complex concept, implying that it is more than simply being free of disease.1
Oral and craniofacial conditions or diseases can impact an individual's health. Any disorder or condition impacting an individual's oral health has the potential for physical, social, and physiological repercussions.2,3 Some individuals may experience physical pain associated with everyday activities such as eating, speaking, and sleeping. Others may feel embarrassed or insecure, leading to self-confidence issues which can hinder interactions with others in social environments. Research suggests that oral and craniofacial conditions or diseases can potentially diminish an individual's oral health-related quality of life (OHRQoL).3
Oral health-related quality of life is a complex model consisting of an individuals' perceptions of oral health in relation to their functional, psychological, and social well-being.3,4 Historically, researchers had focused on measuring oral health based on traditional clinical assessments, solely signifying disease or lack thereof.3,5 However, researchers have identified that traditional dental indices and clinical assessments of oral disease lack the ability to consider this multidimensional concept of health, as they overlook patients' subjective evaluation.6,7
To address this gap, self-assessment measurement instruments have been developed to analyze the physical, psychological, and social effects of oral conditions, known as oral health-related quality of life (OHRQoL). These OHRQoL instruments study the impact of numerous conditions, including but not limited to, dental caries, malocclusion, and craniofacial anomalies,8 and have been customized to measure OHRQoL in specific populations, including individuals with specific conditions.6 OHRQoL instruments have implications for clinical practice, oral health research, and public policy. Specifically, the OHRQoL instrument includes the patient in the decision-making process, potentially improving treatment outcomes. OHRQoL instruments can aid researchers in gaining a greater insight on how oral conditions may affect overall health in addition to impacting health policy by objectively examining oral health disparities.4,6 Although OHRQoL instruments were originally designed for adult populations, recently multiple instruments have been developed and validated to measure the OHRQoL of children.5,8,9
In 2000, the Surgeon General's workshop and conference, "The Face of The Child," recognized the many unmet oral health needs of children and the need to develop OHRQoL assessments for children.10,11 Pediatric and adolescent stages of life, characterized by rapid cognitive and physical growth, are crucial developmental periods, and it has been difficult for researchers to create suitable OHRQoL instruments for these populations.10 To create an appropriate instrument, the child's competence in reading and abstract thinking, as well as the World Health Organization's definition of health must be taken into consideration.11,12
The Child Oral Health Impact Profile (COHIP), developed in 2007, is a validated, self-reported instrument aimed to assess the OHRQoL of children ages 8-15 with various clinical conditions.12 The COHIP was the first instrument to assess both positive and negative impacts of oral conditions including five subscales as well as a parallel form for caregivers.11,12 A condensed version of the COHIP, the COHIP-short form (COHIP-SF), was developed to improve its efficiency and practical application in clinical settings.13 The COHIP-SF contains 20-items, and upholds the reliability and validity of the original questionnaire.13 The COHIP-SF displays a 3.2 grade reading level, and has been shown to be useful in clinical and epidemiological settings.13
Researchers have questioned whether children have the ability to accurately report their quality of life, and whether a caregiver's report regarding their child's OHRQoL should be used as a substitute or in addition to their child's report.13 Although previous studies have found that caregivers are aware of their children's OHRQoL, study results suggest low agreements between children and their caregivers.14,15 The literature suggests that these low agreements may be due to a variety of reasons including the hypothesis that children and caregivers may simply have dissimilar viewpoints.15 It has also been suggested that because caregivers do not observe their children while in school or at other social settings, that they may lack full awareness of their children's OHRQoL.15 Research also suggests there are other potential variables that may provide rationale for children and caregivers reporting different oral health-related OHRQoL scores. Caregivers may overrate or underrate specific aspects that are significant to a child, such as the way they look and how the child feels; in addition the gender of the child and caregiver may also influence OHRQoL scores.13,14
Additional research is needed to explore the relationship between caregiver and child OHRQoL responses to determine the influence of specific variables on their level of agreement. To date, few studies have been conducted in the United States using the COHIP-SF measure as a survey instrument. Despite the original assumptions that children were unable to accurately report their OHRQoL, the COHIP has been shown to be a valid and reliable OHRQoL assessment tool for children experiencing a variety of oral conditions.12,14 Assessing a child's OHRQoL is critical, as oral health issues have both short-term effects, including eating and sleeping, and long-term repercussions that can hinder social abilities and self-confidence.3
Identifying the specific aspects of oral health influencing a child's OHRQoL score can assist oral health professionals in creating a more comprehensive patient care plan to help improve a child's oral health and overall quality of life. Assessing a child's OHRQoL may also help identify emotional and social aspects that caregivers may not be aware of regarding their child's feelings about their oral health. The purpose of this study was to assess the perceived OHRQoL of children at a pediatric hospital and evaluate the level of agreement between child and caregiver reports of OHRQoL.
Methods
This study was approved by the Boston Children's Hospital Institutional Review Board (IRB #P0028991 and the Massachusetts College of Pharmacy and Health Sciences University (IRB #082518R). Non-probability, purposive sampling was used to recruit children, ages 8-15, and their caregivers from a dental clinic in a pediatric hospital for this quantitative, cross-sectional study. Inclusion criteria for the child sample was limited to children between the ages of 8-15; children identified as having intellectual or developmental disabilities, or children with orthodontic appliances, were excluded. Caregivers under the age of 18 or those with intellectual or developmental disabilities were also excluded from the study population. Children and caregivers who spoke languages other than English, were not excluded. However, they were required to utilize the hospital's interpreter services to complete the questionnaire in order to participate.
The validated COHIP-SF questionnaire was used with permission. The questionnaire was modified with two additional items at the end of the questionnaire. The parallel child and caregiver questionnaires were in English and contained a total of 22 items. The first 19 items encompassed three subscales: oral health (5 items), functional well-being (4 items), and social emotional well-being (10 items). Items 1-19 were scored using a 5-point Likert-scale ranging from "never" to "almost all of the time." Item 20 was scored using a 5-point Likert-scale with responses ranging from "poor" to "excellent." Item 20, a global health perception item, assessed the perceived overall oral health. Since this item was highly correlated with the previous COHIP items (1-19) it was excluded from the overall OHRQoL score. Overall scores ranged from 0-76 with higher scores is indicative of a more positive OHRQoL, and lower scores indicative of a lower OHRQoL.
Additional items, 21-22, assessed the level of child/caregiver agreement and were used as a focal point to draw assumptions and conclusions regarding levels of agreement. These questions were added to address the gaps suggested in the literature regarding possible variables impacting child-caregiver agreement, aiding researchers in gaining a better understanding of how much children and their caregivers believe that they are in agreement with one another.
COHIP-SF item 21 addressed how similar the child or caregiver thought their responses would be to one another. Caregivers were asked, "On a scale of 1-10 how similar do you think your child's responses will be to your responses on the questionnaire?" Caregiver responses were based on a numerical scale of 1-10, with 1 being no similarity, and 10 being the same. Similarly, children were asked, "Do you think that your caregiver (mom, dad, or legal guardian) gave the same answers as you on the COHIP questionnaire?" To adjust for age appropriate comprehension, child responses included: yes, no, maybe, and unsure. Item 22 questioned how confident the child or caregiver was regarding their response to the previous question. Children's responses ranged from "I'm extremely sure" to "I'm not sure at all." Caregiver responses ranged from "25% confident" to "100% confident." Caregivers were also asked to provide demographic information including their age, relationship to their child, and their ethnicity as well as their child's age, gender, and ethnicity.
This study also included a review of dental chart records. Items assessed from chart data included number of decayed surfaces (DS), overjet (OJ), and overbite (OB). The number of DS at the most recent dental visit and the amount of OJ were chosen as clinical variables of interest to be consistent with one of the first reliability and validity studies of the COHIP questionnaire.16 The additional variable, OB, was added to the chart review as a means of assessing the impact of OB in relationship to a child's QoL score. Previous research has suggested that repercussions of oral and craniofacial conditions can impact children's overall well-being.11
Both children and their caregivers were approached for potential recruitment during their scheduled dental care appointments. A scripted dialogue was presented to eligible child patients and their caregivers to gain consent to participate. Documentation was obtained from caregiver's acknowledging their consent to take part in the study and providing permission to allow their child to participate. A separate assent procedure was used for child participants.
The respective forms of the COHIP-SF were then distributed to the child participant and their caregiver. All participants were provided with verbal and written instructions describing how to complete the questionnaires. Definitions of quality of life and oral health-related quality of life were explained to the participants. Children and their respective caregiver completed the questionnaires in the same room. However, all participants were required to complete the questionnaires independently. All participants were encouraged to ask the principal investigator (PI) for clarification, as necessary. Participants were directed to read each item and choose the most appropriate answer that represented their respective experiences in regard to their teeth, face, or mouth, over the past three months.
Data were analyzed using SPSS23 software (IBM; Armonk, NY). Tests of association included Pearson correlations. A test of internal reliability, Cronbach's alpha, assessed the interrelationships of the items for each subscale. A Wilcoxon Signed Rank test was used to compare caregiver and child OHRQoL responses. Alpha levels of .05 and 95% confidence intervals (95%CI) were used for hypothesis testing. Linear regression was used to determine the predictive relationship between subscales of caregiver and child responses.
Results
A total of 60 child-caregiver pairs participated in the study (n=120). Pediatric participants included males (n=27, average age of 10.7 years) and females (n=33, average age of 10.6 years) who primarily self-identified as Hispanic/Latino (45%) and African American (31%). The caregiver sample population was predominately mothers (n=46, average age of 41.7 years) and fathers (n=14), average age of 36.8 years.
COHIP-SF quality of life (QoL) Likert scales for each question were coded as: 0=almost all of the time, 1=fairly often, 2=sometimes, 3=almost never, and 4=never. Items 8 and 15 were reverse coded for interpretation to equate higher values with increased QoL. Internal reliability for each of the children's COHIP-SF subscales was found to be poor (oral health, Cronbach's=.60, functional well-being, Cronbach's=.61, socioemotional well-being, Cronbach's=.63), as well as the caregivers' subscales (oral health, Cronbach's=.66, functional well-being, Cronbach's=.36, socio-emotional well-being, Cronbach's=.63). Therefore, all analyses were conducted at the item level or for the total QoL score, which was normally distributed.
Slightly less than one-third of the children (n=18, 30%) said they had crooked teeth or spaces between their teeth and slightly more than one-third of the caregivers (n=21, 36%) agreed. One-third (n=20; 33%) of the children agreed they had been confident because of their teeth, mouth, or face almost all of the time or fairly often, while more than one-third of the caregivers (n=21, 39%) agreed. Similarly, a little more than one-third of the children (n=21, 36%) felt they were attractive because of their teeth, mouth or face as compared to over one-half of their caregivers (n=35, 58%). Nearly three-quarters of the caregivers rated their child's oral health as good or excellent, as compared a little more than one-half with their children. Frequencies associated with each COHIP-SF item response for children and caregivers are displayed in Table I.
All questions were summed for children and caregivers to create new variables for the total QoL score and then averaged to create the mean QoL per question. Overall, the children's total QoL mean score was 59.1 (SD=9.5), with an average of 3.1 (SD=.5). The caregiver's total QoL score was higher than their child's (M=63.0, SD=7.81), with an average QoL of 3.3 (SD=.4). A Wilcoxon Signed Rank test of means showed that the mean total QoL score between caregivers and children was significantly different (z=-.2.4, p=.02). Spearman's rank order test was used to test the relationship between each indication of oral health percentage, overbite OB, OJ, and number of decayed surfaces DS, and the average QoL scores for children, parents, and agreement. Children with no oral health problems reported similar OHRQoL as compared to those with oral health problems. All tests of correlation were non-significant (p>0.05), indicating no relationships were found between oral health indicators and QoL scores.
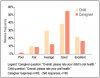
When asked how often they believed that their caregiver agreed with their responses on the COHIP-SF, 27% of the children (n=16) indicated fairly often, 7% (n=4) said sometimes, 48% (n=29) said almost never, and 18% (n=11) said never. Caregivers were asked to rate how similar they thought their answers would be to those of their child on a range from 1 (not similar at all) to 10 (very similar). On the average, caregivers thought that their answers would be similar to their child's (M=7.5, SD=2.3). Spearman's rank order test was used to test the relationship between responses to overall oral health questions, as well as OB, OJ, DS, and average QoL scores for children, parents, as well as agreement. Children with no oral health problems had reported similar OHRQoL compared to those with oral health problems. All tests of correlation were non-significant (p>0.05), indicating no relationships between oral health indicators and QoL scores. Child and caregiver responses to the questions about regarding oral health are shown in Figure 1.
Caregiver/Child agreement
Caregiver and child agreement on COHIP-SF items were assessed by exploring the bi-variate relationships with correlations, item level, and overall differences. Participant responses were positively correlated with the following items: "Had difficulty eating foods you would like to eat because of your teeth, mouth or face" (r=.41, p<.001), "Missed school for any reason because of your teeth, mouth, or face" (r=.42, p<.001), and "Overall, please rate your/your child's oral health" (r=.40, p<.001). Caregiver and child correlations between COHIP-SF items and the overall oral health item are shown in Table II.
The amount of difference between a caregiver and child score was calculated as Scored = Scorep - Score. Overall differences between caregivers and children across all 19 items were calculated by using the absolute value. The overall difference is a normally distributed variable, with an average of 14.5 (SD=6.8). The average total QoL score for caregivers (M=63.0, SD=7.8) was higher than the children's (M=59.1, SD=9.5) score (Wilcoxon Signed Rank, z=-2.4, p=.02, r=.33). The effect size indicated a medium effect according to Cohen's convention. The degree of the caregivers over or underestimation of their child's responses was further examined at the item level. Evaluating differences using the original value instead of the absolute value allowed identification of items caregivers tended to overestimate, underestimate, or agree with their children on average. Figure 2 shows the total differences for each item.
Potential predictors of differences between caregiver and child responses were evaluated using linear regression. The sum total differences between items was regressed onto caregiver age, gender of child, child's rating of how similar their caregivers' responses would be to theirs, and the caregiver's rating of the same. The model was a good fit for the data (R2=.26, F(4, 58)=4.7, p=.002) with gender (β=.32, p=.01), child similarity (β=-.24, p=.05), and caregiver similarity (β=.37, p=.003) as significant predictors. Caregiver age was not a significant predictor (β=.08, p=.53).
A Wilcoxon sign rank test was conducted to further explore the role of gender in relationship to differences in caregiver/child responses. Females had significantly higher (z=-2.4, p=.02) average difference scores (M=6.5, SD=8.3) than male children (M=.81, SD=10.5), with a medium effect size r=.30. The positive value from the average female difference indicates caregivers responded with a higher rating of quality of life than their female children, possibly overestimating their child's self-reported QoL.
Discussion
Caregiver and child ratings correlated on almost all questions with a medium effect, a finding consistent with previous studies comparing caregiver/child agreement using the standard COHIP questionnaire.13,14 Items with the strongest correlations were considered to be more objectively verifiable, such as missing school for any reason or having difficulty eating foods you would like to eat, because of your teeth, mouth or face. In contrast, some items related to social or emotional aspects of QoL did not show any correlation, such as being confident or feeling that you are attractive (good looking) because of your teeth, mouth or face. These findings are of interest as it may be possible that caregivers respond more accurately to their child's responses on items that are portrayed as more physical versus emotional, or regarding the child's own feelings.
Caregivers in this study were more likely to overrate their child's OHRQoL. The greatest areas of disagreement were noted in regard to confidence and feeling attractive because of one's teeth, mouth and face. This lack of correlation may be due to dissimilar viewpoints between children and caregivers. Furthermore, caregivers may be unaware of the specific aspects of oral health that are impacting their child's well-being. Caregivers may also overestimate the social elements of their child's OHRQoL, while they have agreement regarding aspects that can be visibly seen (i.e. spaces, or discolorations).
There were significant differences of agreement between caregivers and the gender of their child. Male children and their caregivers had a fairly high agreement; however, female children and their caregivers had significantly lower levels of agreement. Caregivers overestimated their female child's QoL by an average of 6.46 points of difference, meaning that female children rate their own QoL significantly lower than their caregiver's, as compared to their male cohorts. This finding is similar to those of a study by Broder et al. suggesting that female children with craniofacial clefts may report a lower OHRQoL during adolescence due to body image and self-esteem issues.15 Although the inclusion criteria for this study differed from that of Broder et al,15 the findings associated with gender are similar. Gender disagreement is likely impacted by female children reporting a significantly lower OHRQoL, as consistency was demonstrated with male child and caregiver agreement. Additional studies should focus on female children and on psychological changes throughout childhood and into adolescence (i.e. body image, self-esteem), to further analyze discrepancies found between female and male children, and their caregivers.
This study indicated that children with multiple DS and greater amounts of OB and OJ reported similar OHRQoL as compared to those with no DS and lesser amounts of OB and OJ. No significant differences were found regarding OB, OJ, and DS in relation to QoL variables, including caregiver and child ratings and caregiver/child overall agreement. These findings are in contrast to those of Broder et al, who found that children with higher numbers of DS and greater OJ reported lower OHRQoL.16 No significant differences were identified between the clinical variables in this study, suggesting that dental issues such as DS, OB, and OJ do not strongly influence a child's reported QoL. This finding may support the conclusion that OHRQoL reports from children may rely more on psychological and emotional elements versus physical disease or irregularities. However, because this study did not assess other clinical variables, such as filled surfaces or missing teeth, it is unknown if other significant differences exist. Future studies to investigate psychological/emotional versus physical associations with OHRQoL among children should be explored.
This study had limitations. Data was only collected from one location site, lending itself to purposive sampling and a smaller sample size. Additionally, self-reporting and volunteer bias may have occurred, limiting the external reliability of findings. This was the first study to assess child/caregiver agreement specifically with the COHIP-SF; therefore, the results could only be compared to previous studies utilizing the original COHIP survey instrument. Unlike previous COHIP research, this study focused on pediatric children in general, rather than children with craniofacial and orthodontic conditions. The use of dental charts to assess oral conditions was another limitation. Oral examinations conducted by calibrated examiners may have produced more accurate and comprehensive clinical data. The exclusion of clinical variables such as filled and missing teeth limited the study findings. However, this was not an oversight, but a decision based on limitations found in the dental chart review process.
Conclusion
Results from this study suggest that caregivers may not accurately report their child's actual OHRQoL. The moderate level of agreement found between children and caregivers reinforces the importance of including the child, as well as the caregiver, when assessing OHRQoL. Gender differences and clinical variables should be further explored to determine their impact on OHRQoL and caregiver/child concordance. Assessing the level of agreement between the child and caregiver should be considered for inclusion in future studies utilizing the COHIP-SF.
Acknowledgments
The authors would also like to thank Dr. Hillary L. Broder, PhD, Med, for the permission to use the COHIP-SF 19 in this study.
About the Authors
Renee Wall, MS, RDH is a graduate of the Forsyth School of Dental Hygiene, MCPHS University, Boston, MA; Lori Rainchuso, DHSc, MS, RDH is an associate professor, School of Healthcare Business, Doctor of Health Sciences Program, MCPHS University, Boston, MA; Jared Vineyard, PhD is a post-doctoral fellow at St. Lukes Applied Research, Boise, ID and adjunct faculty member at MCPHS University, Boston, MA; Lory Libby, MS, RDH is an assistant professor, Forsyth School of Dental Hygiene, MCPHS University, Boston, MA.
Corresponding author: Lori Rainchuso, DHSc, MS, RDH; Lori.rainchuso@mcphs.edu
References
1. U.S. Department of Health and Human Services. Oral health in America: a report of the Surgeon General [Internet]. Rockville (MD): U.S. Department of Health and Human Services. 2000 [cited 2019 June17]. Available from: https://profiles.nlm.nih.gov/ps/access/NNBBJT.pdf
2. McGrath C, Broder H, Wilson-Genderson M. Assessing the impact of oral health on the life quality of children: implications for research and practice. Community Dent Oral Epidemiol. 2004 Apr 4; 32(2):81-5.
3. Alzoubi E, Hariri R, Mulligan K, Attard N. An evaluation of oral health related quality of life in orthodontic patients treated with fixed and twin blocks appliances, J Orthod Sci. 2017 Apr-Jun;6(2):65-70.
4. Shisco L, Broder HL. Oral health related quality of life-what, why, how, and future implications. J Dent Res. 2011 Mar 21;90(11):1264-70.
5. Piovesan C, Batista A, Ferreira FV, Ardenghi TM. Socioeconomic inequalities in the distribution of dental caries in Brazilian preschool children. J Public Health Dent 2010 Fall:70(4):319-26.
6. Bennadi D, Reddy CVK. Oral health related quality of life. J Int Soc Prev Community Dent. 2013 Jul 26; 3(1):1-6.
7. Allen PF. Assessment of oral health related quality of life. Health Qual Life Outcomes. 2003 Sep 8;1:40.
8. Gilchrist F, Rodd H, Deery C, Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014 Apr 23;14:1.
9. Genderson M, Sischo L, Markowitz K, et al. An overview of children's oral health-related quality of life assessment: from scale development to measuring outcomes. Caries Res. 2013 Oct 7;47(s1):13-21.
10. Broder HL. Children's oral health related quality of life. Community Dent Oral Epidemiol. 2007 Jul 3;35(S1):5-7.
11. Mouradian WE. The face of a child: children's oral health and dental education. J Dent Educ. 2001 Sep;65(9):821-31.
12. Broder HL, McGrath C, Cisneros GJ. Questionnaire development: face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent Oral Epidemiol. 2007 Jul 3;35(s1):8-19.
13. Wilson-Genderson M, Broder HL, Phillips C. Concordance between caregiver and child reports of children's oral health-related quality of life. Community Dent Oral Epidemiol. 2007 Jul 3;35(s1):32-40.
14. Vashisth S, Devi A. An assessment of agreement between child and caregiver's report of child's oral health related quality of life. JCMD. 2015; 4(1):12.
15. Broder HL, Wilson-Genderson M, Sischo L, Norman RG. Examining factors associated with oral health-related quality of life for youth with cleft. Plast Reconstr Surg Glob Open. 2014 Jun;133(6):828e-834e.
16. Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child's version). Community Dent Oral Epidemiol 2007 Aug;35(s1):20-31.