You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
The increasing prevalence of childhood obesity is a major public health concern in the United States (U.S.) as well as globally.1-5 Obesity prevalence in children and adolescents in the U.S. aged 2 to 19 years of age was 17% and extreme obesity was 5.8% in 2014.2,4 Causes for obesity are complex and multifactorial and include contributing factors such as genetics, environmental, behavioral, poor diet, and a sedentary lifestyle.1,3 In children, feeding practices by caregivers are a modifiable risk factor for prevention of overweight and obesity in the early years of life.6 A modifiable risk factor for obesity in particular, is the intake of sugar-sweetened beverages (SSBs), which increases the odds of being overweight and obese by 1.55 and is a determinant of body weight.7 Added sugars also increase the risk for dental caries; a systematic review suggests the intake of added sugars must be below 5% to lower caries risk.8
The American Association of Pediatric Dentistry (AAPD), American Dental Association (ADA), and American Dental Hygienists' Association (ADHA) all have policies related to use of national guidelines to encourage healthy food choices and reduce added sugars, especially those found in SSBs such as soft drinks, sports drinks, and energy drinks.9-11 Dental hygienists (DHs) provide nutritional counseling for caries prevention and control along with overall wellness as a key educational component of the preventative dental appointment.12 Because children 3 to 12 years of age have more dental visits (51%-55%) than medical visits (34%), they build a trusted patient/clinician relationship, and place DHs in a favorable position to provide nutritional counseling and education on childhood obesity.12
Obesity and Systemic Health
Childhood obesity has both physical and psychological effects, leading to chronic medical conditions, such as the accelerated onset of type-2 diabetes mellitus. Insulin resistance/hyperinsulinemia is believed to be an important link to metabolic abnormalities, obesity, risk for cardiovascular disease, and place the child at risk for adult obesity, ultimately impacting mortality and morbidity.1,4,13,14 In addition, childhood obesity can lead to social stigma having a direct impact on the child's and adolescent's social, behavioral, and emotional well-being.2
Obesity and Oral Health
Since caries detection is a routine part of oral health assessment in the dental office, several studies have been carried out to evaluate the relationship between obesity and dental caries but the findings were inconsistent.15-19,20 However, a systematic review and meta-analysis by Hayden et al reported a statistically significant relationship (p=0.049) between dental caries and childhood obesity.15
Birth weight, infant obesity, nutritional risk factors, and socio-economic factors demonstrate associations with the prevalence of early childhood caries (ECC) and obesity in a number of studies.16,18,19 Since childhood obesity is a multifactorial issue, caloric intake and the types of foods consumed, such as SSBs, are an area for further investigation to fully determine the association between dental caries, nutrition, and obesity.
The evidence suggests an association between obesity and periodontitis in adult populations.21 A recent systematic review and meta-analysis suggests an association between childhood obesity and signs of periodontal disease including bleeding on probing, probing depth, and plaque index.21 Further research is needed in this area to clarify the relationship.22
Medical Professionals
Health care professionals provide health services to young children and adolescents and can have an impact on addressing childhood obesity. Studies indicate that although Primary Care Providers (PCPs) face many barriers in providing intervention such as parental involvement, patient motivation, lack of time, and support services, they understand the importance of managing childhood obesity for short- and long-term disease prevention.23-27 PCPs feel more comprehensive training and education would be needed to adequately address this sensitive issue.27
Dental Professionals
Several studies to assess knowledge, attitudes, beliefs, and barriers of dental professionals to addressing obesity have been conducted.28-31 Curran et al and Lee et al in separate studies surveyed general and pediatric dentists about their role in providing obesity education in adults and children.28,30 Respondents felt they would only consult the patient on obesity when an established link between oral and systemic health had been verified.28,30 Major barriers were lack of training to properly educate and assist patients; and fear of offending the parent/patients; and having them leave the practice.28,30
Kading et al surveyed North Carolina dental hygienists (DH) regarding factors affecting confidence in providing obesity education and counseling in adult populations.29 Survey results showed that 95% of respondents felt DHs had a role in improving patient nutrition, while only 36% considered assisting patients in achieving their weight loss goals was part of the DH role and 82% were more apt to educate and counsel patients regarding oral health issues.29 In regards to confidence in obesity education and counseling, a primary focus of the study, 65% of respondents expressed a level of confidence in discussing obesity-related health risks.29 Of note were 17% of the respondents reporting negative attitudes about overweight people, suggesting that obese individuals lack willpower.29 While DHs reported learning nutrition counseling during their educational program, assessments for overweight or obesity were not part of the curriculum.29
Additional research in dental and DH students conducted by Magliocca et al found that 92% percent of students reported fewer than five hours of obesity education.31 Even though 96% of the respondents considered assessing dietary habits an important component of preventive oral care, 31% reported discomfort in addressing nutrition with obese patients.31 About one-third of students held negative stereotypes regarding obese patients including lack of willpower and laziness and 11% felt overweight/obese patients lacked will power.31 These findings suggest the need to address obesity and approaches in supporting patients in behavior change to improve oral and general health.31
Childhood obesity is a public health concern both in the U.S. and around the world.3 The purpose of this study was to assess DHs knowledge, beliefs, attitudes, and barriers in educating patients/parents about childhood obesity in the dental setting to update and expand on the research of Kading et al.
Methods
A cross-sectional survey research design with a random sample of DHs was utilized for this study. Massachusetts College of Pharmacy and Health Sciences (MCPHS) University's Institutional Review Board granted the study an exempt status under 45 CRF 46.101(B) (2) protocol number IRB062716C.
Survey design
The questionnaire was developed by combining survey instruments from the studies of Curran et al and Ip et al.30,32 The Nutrition, Exercise and Weight Management (NEW) Attitudes Scale was developed and validated by Ip et al to measure medical students' attitudes and beliefs regarding obese patients.32 The NEW Attitudes scale had a test-retest reliability of 0.89 with moderate correlation to two previously validated measures of obesity bias.32 Curran et al developed a survey to explore the dentists' role in addressing obesity in adults and was modified to fit the topic of childhood obesity.30 The NEW survey was used in its entirety along with the modified survey from Curran et al; both surveys were used with permission from the authors.
The final survey instrument contained 7 sections: knowledge (9 items); attitudes and beliefs (34 items); practices (9 items); barriers (9 items); resources needed (1 item); practice information (2 items); and demographics (7 items). A 3-point Likert Scale was used to assess level of agreement to the questions.
Content validity was established with a panel of five nutrition and oral health experts.33 A validation form was used to rate each survey question for the content validity index (CVI) on a 4-point scale.33 The percentage of agreement about the relevance of each item was computed for the item CVI (I-CVI) and the scale CVI (S-CVI) was computed by the total of I-CVI's divided by the number of survey questions.33 An acceptable I-CVI rating among the panel of experts must result in 0.78 or higher, and the S-CVI must result in 0.90 or higher in order to determine adequate content validity of the questionnaire.33 The individual survey questions each received an adequate I-CVI score ranging from 0.8-1. The overall S-CVI score was .93, suggesting the survey was an adequate representation of this study's research questions. The survey was then pilot tested by a group of 10 DHs for feedback on clarity of questions with no revisions recommended. The final survey was entered into Survey Monkey®.
Survey participants
Participants were recruited through the American Dental Hygienists' Association (ADHA) database of members. ADHA chose a random sample of 13,492 DHs with a 99% delivery rate resulting in a final sample size of 13,357. Of these, 1,046 individuals accessed the survey. Post stratification was used to weight the data by gender and race in order to match U.S. population percentages34 and account for non-response bias.35
Survey Procedures
An email invitation containing a link to the survey was sent by ADHA to the selected sample. Participants were given 2 weeks to complete the survey. A second email reminder was sent by ADHA at the end of the second week and participants were given 2 more weeks to complete the survey. Investigators did not have access to the email list.
Data analysis
Weighted data were used for all analysis and were examined using statistical software (IBM,SPSS 24®). Demographics and participants' responses were calculated using summary statistics. Participant responses to "attitude" questions were appropriately weighted and summed, providing a summary "attitudes", anti-fat, self-efficacy, and patient knowledge score for each participant, as in the previously validated survey instrument.32
The χ2 test of independence was employed to examine responses on knowledge, attitude, practice and barrier items by level of DH education and source of nutrition education. The Fisher's exact test was applied whenever there were inadequate cases within the cells. A Bonferroni correction was used on all tables larger than 2x2 to correct for omnibus familywise error.
Clinical research often reports p-values alone, however, this study also used an effect size to calculate the strength of the association. Effect sizes calculate the strength or magnitude of an effect and are key in interpreting clinical research. While a significant p-value can be found, the effect size may be small and thus not relevant to clinical practice.36 In this study the phi coefficient (Φ) is reported to indicate the degree of association between variables in the χ2 test. Values of .10 are considered small, .30 medium, and .50 large effect sizes.37
A Spearman's rank order correlation was used to assess the relationship between age and all response items. Univariate multiple linear regression analyses were conducted to assess the association between participants "attitudes" scores and responses to practices items and all statistical tests were performed at an alpha threshold of 0.05.
Results
Participation Rate
Following dissemination of the survey link to the sample population, one individual emailed to indicate they were no longer practicing and was removed from future sample calculations. Therefore, 1046 independent attempts were recorded with 919 completed surveys and the overall participation rate for this survey was 89.1%. The participation rate (PR) was reported as recommended by the American Association for Public Opinion Research.38 PR is the number of people completing the survey divided by the number of people who started the survey, as the sources of non-response are unknown.38
Demographics
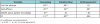
The majority of the participants were white females (91%) with an average age of 28 years (SD=12.22) (Table I). Less than half held a certificate or Associate's degree in Dental Hygiene (AS) with 40% holding a Bachelor's degree (BS), and 15% a Master's degree (MS). Over half reported having some nutrition content in their entry-level DH educational program while 31% indicated receiving obesity education through continuing education; including self-study and workshops. Over 67% of the participants were employed in a general practice, with 71% seeing fewer than 10 pediatric patients per week.
Early Versus Late Respondents
The non-response adjustment method was used to address the non-response bias in the study sample.38 Comparing respondents to non-respondents presents challenges in survey research and several methods have been developed to estimate the potential differences between people who respond and non-responders. This includes treating "late" responders as non-responders and using those late responders to compare to early participants. For this study, individuals who responded before the reminder email was sent were considered early responders and all others were considered late. Independent sample t-tests were performed on continuous variables and a χ2 test of independence was used to examine the relationship across the all categorical variables. Early responders were not different than late responders on any of the variables (p>.05).39
Knowledge
Table II illustrates DHs' knowledge about obesity, and relationships with oral and systemic health. Most respondents understood the risk of obesity and other health issues (99%) and a majority understood the role of SSBs in contributing to the added sugar content in diets (76%), and the quantities of SSBs consumed by youth (91%). Although the respondents (28%) did not feel overweight children were more likely to become overweight adults, they felt parental obesity was a strong risk factor for childhood and adolescent obesity, with maternal obesity having the greatest effect (76%). Dental hygienists felt unsure regarding their knowledge about the association between obesity and dental caries (56%), although they felt current research demonstrates an association between obesity and periodontal disease with an increased BMI (62%).
Attitudes and Beliefs
Participants' attitudes and beliefs about obese patients are illustrated in Table III. These questions explored the understanding of the risk factors of obesity and DHs' attitudes and beliefs towards educating and discussing weight related issues.30 Results showed DHs had a slightly more positive attitude (4.11) about obese patients, compared to Kading et al and Magliocca et al respondents, who had a negative attitude in that patients lacked will power (17%). One-third of respondents reported a negative stereotype of obese patients.
Significantly more respondents in the MS group (76%) agreed it would be rewarding to provide nutritional counseling versus 60% of the BS group (χ2(4, 907)=13.32, p=.01, Φ=.12). Master's level hygienists (45%) also indicated patients are likely to follow an agreed upon plan to increase their physical activity as compared to 34% of BS respondents. The AS group (41%) had the lowest number of individuals who were neutral on the same statement.
The NEW scale contains several items indicating the perceived self-efficacy of a hygienist for helping obese patients. Seventy-three percent of DHs with obesity education as continuing education (COE) agreed it would be rewarding to talk to someone about nutrition when compared to 61% of those with obesity education in an entry-level DH program (ELOE) (χ2(4, 907)=13.73, p=.01, Φ=.12). Additionally, 62% of the COE group agreed that they had a personal desire to counsel patients about nutrition with only 42% of ELOE respondents indicating the same desire (χ2(4, 907)=30.29, p<.001, Φ=.18). On a related item, 36% of the COE group agreed that they had a personal desire to counsel patients about physical activity with 20% of the same group disagreeing. Only 26% of those with ELOE reported a desire to provide physical activity counseling with 32% the ELOE group in disagreement (χ2(4, 907)=17.92, p=.001, Φ=.14). Significantly more of the COE group (28%) versus 18% of those with ELOEs agreed in having a personal desire to counsel patients about weight management (χ2(4, 907)=21.85, p<.001, Φ=.16). In contrast, 22% of those with COE indicated feeling awkward discussing weight when a patient is overweight/obese, versus only 15% of those with ELOE regarding the same response (χ2(4, 907)=10.08, p=.04, Φ=.11).
The NEW scale also contains several items indicating a person's anti-fat attitude. Among respondents, 56% of the ELOEs were in disagreement with the statement that people can eat a healthy diet if they choose to do so compared to 47% of those with COE (χ2(4, 907)=10.08, p=.04, Φ=.11). All other tests of independence between attitude items and obesity education source were not significant.
Practices
The practices DHs currently incorporate into assessing and educating for obesity in the dental practice are illustrated in Table IV. Most participants reported never measuring height and weight and 95% have never plotted BMI in children. Over half always provide nutritional counseling to reduce consumption of SSB drinks, but only 65% reported that they sometimes provide nutritional counseling to encourage healthy eating.
Most respondents reported never collaborating with school officials or other health professionals to ensure healthy food choices are available in schools. In addition, 76% report never referring to a Primary Care Provider (PCP) or registered dietitian nutritionist (RDN).
Tests of independence demonstrated significant relationships between source of obesity education and three practice items. First, more of the COE participants (23%) indicated they always provide nutritional counseling to encourage healthy eating, while only 15% of the ELOEs endorsed the same frequency (χ2(4, 919)=17.10, p=.002, Φ=.14). Second, participants in the COE group reported they either never (70%), sometimes (22%), or always (8%) advocate with school officials or leaders to ensure school food services, including vending services and school stores, provide nutritious food selections as compared to the ELOEs group (never=81%, sometimes=15%, and always=4%), (χ2(4, 919)=16.92, p=.002, Φ=.14). Finally, COEs are more likely to always (9%) or sometimes (24%) collaborate to increase awareness of the importance of maintaining healthy vending choices in schools, and to encourage the promotion of beverages of high nutritional value than those with ELOE (always=4%, sometimes=14%), (χ2(4, 919)=28.83, p<.001, Φ=.17).
Barriers
The major barriers to educating patients about childhood obesity were limited time, cited by 63% of the respondents. Minor barriers included insufficient knowledge about the guidelines for prevention and management of childhood obesity (52%), lack of confidence in addressing obesity issue (51%), lack of training to counsel on healthy eating for weight management (45%), lack of patient acceptance from a dental professional (51%), and lack of knowledge about making the appropriate referral (53%).
Dental Hygienists in the BS group (69%) said finding enough time in their schedule was a major barrier, compared to 63% of MS and 59% of AS level DHs (χ2(4, 919)=10.80, p=.03, Φ=.11). One-quarter of the Master's level DHs did not feel that lack of confidence in addressing the obesity issue with patients was a barrier as compared to 10% of the BS group and 17% of the AS group. (χ2(4, 919)=19.48, p=.001, Φ=.15). Lack of training about counseling for healthy eating patterns for weight management showed the largest difference between the MS group (26%), who were more likely not to see training as a barrier, in contrast to only 13% of the BS group. (χ2(4, 919)=12.37, p=.02, Φ=.12). In regards to lack of knowledge about making appropriate referrals, 22% of the MS group versus 12% of the BS group saw this as a barrier. (χ2(4, 919)=10.26, p=.04, Φ=.11).
Fear of offending a parent or patient was seen by 62% of the ELOEs as being a major barrier versus 38% of the COEs (χ2(4, 919)=25.80, p<.001, Φ=.17). Thirty-percent of the COE group viewed lack of training about counseling for healthy eating patterns for weight management a barrier as compared to 41% of the ELOEs (χ2(4, 919)=18.69, p<.001, Φ=.14). The COE group was less likely (29%) to see patient resistance to healthy eating advice as a major barrier as compared to 42% of the ELOEs (χ2(4, 919)=25.44, p<.001, Φ=.17). Only 28% of COEs thought lack of knowledge in making appropriate referrals for care was a major barrier as compared to 34% of the ELOEs. (χ2(4, 919)=24.12, p<.001, Φ=.16). The perceived barriers to educating about childhood obesity are illustrated in Table V.
Attitude Associations
Associations between attitude and practice was examined using multiple regression with the anti-fat, self-efficacy, and patient belief scales predicting each of the practice scales are displayed in Table VI. Practice scales were created by combining all items related to nutrition counseling (counseling), collaboration with other professionals (collaboration), and collecting/plotting anthropometric data and conducting a factor analysis.
Anti-fat, self-efficacy and patient beliefs were all significant positive predictors of the frequency that DHs provide obesity related counseling in practice. Anti-fat attitudes and self-efficacy scales were significant predictors of the frequency of collaboration and referral by hygienists. The model of attitude subscales predicting anthropometric frequency was not significant (p=.08) however the self-efficacy scale was a significant predictor within the model (p=.03). Overall, self-efficacy was the most robust predictor of practice frequency.
Discussion
Childhood obesity prevalence is a major public health concern.1,3 Risk factors such as Type 2 diabetes mellitus and cardiovascular disease, once considered adult-onset diseases, have increased dramatically among youth.40,41 Many respondents reported understanding the risk factors for systemic diseases and the majority understood the role SSBs play in the high sugar content in the child's diet. However, only about half reported consistently counseling patients on SSB consumption, and just over half (65%) reported sometimes counseling patients on healthy eating. Nutrition counseling on healthy eating to reduce caries risk and improve overall health is supported by the policies of the major professional dental organizations including the AAPD, ADA, and AHDA as an area that should be addressed as part of the preventative dental appointment.9-11
Since there is conflicting information regarding obesity and dental caries16,19 respondents were unsure of the relationship. Goodson et al and Mojarad et al evaluated the association between childhood obesity and dental caries and concluded that although dental caries increases with sugar consumption, obesity may not be a primary cause of caries,16,20 which may be the source of uncertainty in the respondents.
Study participants, particularly those who had engaged with obesity education in a continuing education format (COE), found it rewarding to discuss nutrition with patients and noted a personal desire to do so, but felt awkward discussing weight with someone who is overweight/obese. Participants in this study stated they would be uncomfortable discussing weight related issues unless the patient had an identifiable systemic/oral link, which was similar to the findings in previous studies.20,28,29 Interestingly, a study by Tavares and Chomitz on healthy weight interventions in the dental office found 95% caregivers of children felt the dental office is an appropriate place to get information on healthy eating and exercise, and 95% of caregivers felt the DH was a good person to discuss height and weight goals with the child and parent.42 These findings suggest an inconsistency between DHs perceptions regarding the response of caregivers/parents/patients to education about obesity intervention in the dental setting and their actual response.29,42
Findings in this study are similar to Kading et al in that a little over half (58%) of DHs lack the confidence to provide obesity education for prevention and management.29 Further investigation into the relationship between childhood obesity and caries may provide DHs with more confidence to discuss obesity, support healthy eating and provide referrals to PHPs for further evaluation when indicated.
Results from this study regarding attitudes and beliefs about obese patients were similar of Ip et al findings in medical students.32 Medical students in the Ip et al study had a mildly positive attitude (24.4) and DHs in this study had slightly positive attitude (4.15).32 The anti-fat and self-efficacy subscales of the attitudes scale in this study predicted the frequency of practice. Respondents with a more positive attitude about obese patients were more likely to provide counseling on a lower intake of SSBs, encourage healthy eating along with referral to a primary care provider, advocate/collaborate with schools to change policy, and refer to a PCP or RDN. This finding suggests the importance of further education at the graduate level or continuing education on obesity to dispel stereotypes and social stigmas. Further education on obesity intervention and management may enhance practice behaviors to address obesity in the dental setting and encourage inter-professional collaboration to benefit the patient's oral and overall health.
The barriers reported in this study were similar to those reported in the literature.28-31 Barriers included time constraints, fear of offending the parent/child, and a lack of knowledge on the guidelines for management of childhood obesity to be successful.
Only about half of participants in this study reported having received nutrition education which was unexpected given it is required as part of the Commission on Dental Accreditation Standards for Dental Hygiene Education Programs.43 Lack of obesity education in entry-level DH program curricula, may deter DHs' ability to gain the knowledge needed to be confident in assessing and educating for childhood obesity. Multiple studies report that DHs feel their education in assessing and educating for childhood obesity is limited, and that fear of offending the parent/child is a major barrier for implementation.28-31,44 Results from this study suggest higher levels of self-efficacy were a predictor of practice behaviors. Education in entry-level programs as well as continuing education opportunities may influence self-efficacy so DHs will be confident in providing education without fear of offending the parent or child.
A limitation to this study was the participation rate from the ADHA mailing list. Efforts were made during analysis to correct for bias by weighting the data and compare early respondents vs. late respondents. In addition, self-report surveys are susceptible to report bias such as responding in a socially desirable way to questions about attitudes, beliefs, and current practices.
Conclusion
Dental hygienists understand the increased risk factors with obesity and systemic health. While confident in providing nutritional counseling for caries prevention and management, only a little more than half address healthy eating and the intake of sugar-sweetened beverages. Brief nutrition interventions, along with referral to a health care provider by the dental hygienist, can assist overweight and obese patients in making incremental changes in weight management without the risk of offending the patient or parent. Contrary to the commonly held belief by dental hygienists regarding the openness of patients and caregivers to obesity education, research indicates that the vast majority of caregivers of children are open to nutritional education in the dental office setting.42
Basic nutritional counseling for a healthy lifestyle and obesity education needs to be incorporated into entry-level DH education and made available to practicing DHs to increase their knowledge and confidence in their role as members of interprofessional healthcare teams to manage the obesity epidemic.
Acknowledgements
The authors extend their thanks to the panel of experts for agreeing to share their expertise on this topic: Cyndee Stegeman, EdD, RDH, RD, LD, CDE, FAND; Lori Rainchuso, RDH, DHSc; Lisa Mallonee, MPH, RDH, RD, LD; Carole Palmer, EdD, RD, LDN; as well as to the dental hygienists who participated in making this research study possible.
About the Authors
Doreen Dawn M. Cole, RDH, MS is a territory sales manager with Hoya Corp, Dallas, TX; Linda D. Boyd, RDH, RD, EdD is dean and professor, and Lori J. Giblin-Scanlan, RDH, MS, is an associate professor and associate dean of clinical sciences; all are at the Forsyth School of Dental Hygiene, MCPHS University, Boston, MA.
Jared Vineyard, PhD is a postdoctoral fellow in the Idaho Center for Health Research at Idaho State University, Meridian, ID.
Corresponding Author: Linda D. Boyd, RDH, RD, EdD; linda.boyd@mcphs.edu
References
1. World Health Organization. Report of the Commission on Ending Childhood Obesity (ECHO). [Internet]. Geneva, Switzerland: WHO; 2016. [cited 2017 Jan 31]/ Available from: pps.who.int/iris/bitstream/10665/204176/1/9789241510066_eng.pdf
2. World Health Organization. Obesity and overweight. Fact sheet. [Internet]. Geneva, Switzerland: WHO; 2016 [cited 2017 June 26]. Available from: http://www.who.int/mediacentre/factsheets/fs311/en/
3. United States Public Health Service. Office of the Surgeon General. The surgeon general's vision for a healthy and fit nation. [Internet]. Rockville, MD: Office of the Surgeon General; 2010. [cited 2017 Jan 31]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK44660
4. Ogden CL, Carroll MD, Lawman HG, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. J Am Med Assoc. 2016;315(21):2292-9.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. J Am Med Assoc. 2012;307(5):483-90.
6. Dattilo AM, Birch L, Krebs NF, et al. Need for early interventions in the prevention of pediatric overweight: a review and upcoming directions. J Obes. 2012;2012:123023.
7. Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2012;346:e7492.
8. Moynihan P. Sugars and dental caries: Evidence for setting a recommended threshold for intake. Adv Nutr. 2016;7(1):149-56.
9. American Academy of Pediatric Dentistry. Policy on dietary recommendations for infants, children, and adolescents. Pediatr Dent. 2016;38(6):57-9.
10. American Dental Hygienists' Association. Policy manual. [Internet]. Chicago, IL: ADHA; 2016 [cited 2017 June 25]. Available from: https://www.adha.org/resources-docs/7614_Policy_Manual.pdf
11. American Dental Association. Current policies and historical publications. [Internet]. Chicago, IL: ADA; 2016 [cited 2017 June 25]. Available from: http://www.ada.org/en/member-center/leadership-governance/historical-publications-policies
12. Tseng R, Vann WF, Jr., Perrin EM. Addressing childhood overweight and obesity in the dental office: rationale and practical guidelines. Pediatr Dent. 2010;32(5):417-23.
13. Marcovecchio ML, Mohn A, Chiarelli F. Obesity and insulin resistance in children. J Pediatr Gastroenterol Nutr. 2010;51 Suppl 3:S149-50.
14. Herder C, Schneitler S, Rathmann W, et al. Low-grade inflammation, obesity, and insulin resistance in adolescents. J Clin Endocrinol Metab. 2007;92(12):4569-74.
15. Hayden C, Bowler JO, Chambers S, et al. Obesity and dental caries in children: a systematic review and meta-analysis. Community Dent Oral Epidemiol. 2013;41(4):289-308.
16. Goodson JM, Tavares M, Wang X, et al. Obesity and dental decay: inference on the role of dietary sugar. PLoS One. 2013;8(10):e74461.
17. Gunjalli G, Kumar KN, Jain SK, et al. Total salivary anti-oxidant levels, dental development and oral health status in childhood obesity. J Int Oral Health. 2014;6(4):63-7.
18. dos Santos Junior VE, de Sousa RM, et al. Early childhood caries and its relationship with perinatal, socioeconomic and nutritional risks: a cross-sectional study. BMC Oral Health. 2014;14:47.
19. Elangovan A, Mungara J, Joseph E. Exploring the relation between body mass index, diet, and dental caries among 6-12-year-old children. J Indian Soc Pedod Prev Dent. 2012;30(4):293- 300.
20. Mojarad F, Maybodi MH. Association between dental caries and body mass index among hamedan elementary school children in 2009. J Dent. 2011;8(4):170-7.
21. 2Martens L, De Smet S, Yusof MY, Rajasekharan S. Association between overweight/obesity and periodontal disease in children and adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent. 2017;18(2):69-82.
22. Li LW, Wong HM, Sun L, et al. Anthropometric measurements and periodontal diseases in children and adolescents: a systematic review and meta-analysis. Adv Nutr. 2015;6(6):828-41.
23. Gerards SM, Dagnelie PC, Jansen MW, et al. Barriers to successful recruitment of parents of overweight children for an obesity prevention intervention: a qualitative study among youth health care professionals. BMC Fam Pract. 2012;13:37.
24. Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110(1 Pt 2):210-4.
25. Sivertsen LM, Woolfenden SR, Woodhead HJ, Lewis D. Diagnosis and management of childhood obesity: a survey of general practitioners in South West Sydney. J Paediatr Child Health. 2008;44(11):622-9.
26. Redsell SA, Atkinson PJ, Nathan D, et, al. Preventing childhood obesity during infancy in UK primary care: a mixed-methods study of HCPs' knowledge, beliefs and practice. BMC Fam Pract. 2011;12:54.
27. Walker O, Strong M, Atchinson R, et,al. A qualitative study of primary care clinicians' views of treating childhood obesity. BMC Fam Pract. 2007;8:50.
28. Lee JY, Caplan DJ, Gizlice Z, et al. US pediatric dentists' counseling practices in addressing childhood obesity. Pediatr Dent. 2012;34(3):245-50.
29. Kading CL, Wilder RS, Vann WF, Jr., Curran AE. Factors affecting North Carolina dental hygienists' confidence in providing obesity education and counseling. J Dent Hyg. 2010;84(2):94-102.
30. Curran AE, Caplan DJ, Lee JY, et al. Dentists' attitudes about their role in addressing obesity in patients: a national survey. J Am Dent Assoc. 2010;141(11):1307-16.
31. Magliocca KR, Jabero MF, Alto DL, Magliocca JF. Knowledge, beliefs, and attitudes of dental and dental hygiene students toward obesity. J Dent Educ. 2005;69(12):1332-9.
32. Ip EH, Marshall S, Vitolins M, et al. Measuring medical student attitudes and beliefs regarding patients who are obese. Academic Med. 2013;88(2):282-9.
33. Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459-67.
34. American Community Survey (ACS), One-Year Public Use Microdata Sample (PUMS), 2015-16. [Internet]. Suitland, MD: US Census Bureau; 2016 [cited 2017 Aug 1]. Available from: https://www.census.gov/programs-surveys/acs/
35. Holt D, Smith TMF. Post stratification. J Royal Statistical Society. 1979;142(1):p33-46.
36. Cummings G. Understanding the New Statistics: Effect sizes, confidence intervals, and meta- analysis. New York, NY.: Routledge; 2012. 536 p.
37. Guilford JP. Psychometric Methods. 2nd ed. New York, NY.: McGraw-Hill; 1954. 597 p.
38. Baker R, Brick, JM, Bates, NA, et al. Summary report of the AAPOR task force on non-probability sampling. J Survey Statistics and Methodology. 2013;1(2):90-143.
39. Lindner J, Murphy TH, Briers, G.E. Handling nonresponse in social science research. J Agricultural Education. 2001;42(4):43-53.
40. Sanders RH, Han A, Baker JS, Cobley S. Childhood obesity and its physical and psychological comorbidities: a systematic review of Australian children and adolescents. Eur J Pediatr. 2015;174(6):715-46.
41. l'Allemand-Jander D. Clinical diagnosis of meta- bolic and cardiovascular risks in overweight children: early development of chronic diseases in the obese child. Int J Obes. 2010;34 Suppl 2:S32-6.
42. Tavares M, Chomitz V. A healthy weight intervention for children in a dental setting: a pilot study. J Am Dent Assoc. 2009;140(3):313-6.
43. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs. [Internet]. Chicago: Commission on Dental Accreditation; 2016 [cited 2017 Jan 7]. Available from: http://www.ada.org/~/media/CODA/Files/ dh.pdf?la=en.
44. Hisaw T, Kerins C, McWhorter AG, Seale NS. Pediatric obesity curriculum in pediatric dental residency programs. Pediatr Dent. 2009;31(7):486-91.