You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Introduction
Dental hygienists have been administering local anesthesia (LA) dating back to 1971 when legislation was enacted to expand the scope of practice in the state of Washington.1 Since then, 44 of the 50 states include the administration of LA within the scope of practice for dental hygienists.1 Due to restrictions and limitations within individual dental practice acts, most states require the presence of a dentist for the administration of LA; however research has demonstrated that dental hygienists can administer LA safely.2 Scofield et al. surveyed state boards and found that there were no reports of disciplinary actions against dental hygienists related to the administration of LA among the respondents.2
Of the 44 states allowing for the administration of LA by dental hygienists, 35 require direct supervision by a licensed dentist, seven require general supervision, one allows for indirect supervision, and 2 are a mix of general and direct supervision, depending on the geographical location of the practice setting.1 Direct supervision is defined as requiring the dentist to be physically present while the procedure is performed while indirect supervision means that a dentist must authorize the procedure and be in the practice setting while the procedure is performed.3 General supervision is defined as authorizing the procedure to be performed but not required to be physically present in the practice setting. In addition to supervision requirements, there are limitations on the types of LA that dental hygienists are allowed to administer; some states allow both block and infiltration while others allow infiltrations only.1 The state of Virginia limits the administration of block and infiltration LA to patients over the age of 18.1
Dental hygienists have been administering LA under direct supervision in the state of California since 1976.1 Additionally, dental hygienists are allowed to provide other aspects of oral hygiene assessments including the preliminary examination, non-surgical periodontal therapy (NSPT), and subgingival irrigation with liquid anti-microbial agents under general supervision as defined by California code.4 Limitations to the pain management options provided during NSPT due to supervision requirements can impact the quality of care for patients during NSPT, however research is limited regarding supervision requirements and their impact on quality pain control. A study conducted by Rich et al. examined whether or not the expansion of the scope of practice of California dental hygienists had led to greater utilization of the administration of LA, nitrous oxide and oxygen analgesia and the provision of soft-tissue curettage, over the first four years after the implementation of the law.5 Results from the study demonstrated that the majority (90%) of the recent dental hygiene graduates were utilizing at least one of the expanded duties and that 86% of the general dentist and 100% of the periodontist respondents were delegating at least one of these duties, thus demonstrating highly favorable acceptance of these expanded duties in California.5
Education standards for the didactic and clinical content for LA curricula in both dental and dental hygiene education programs are established by the Commission on Dental Education.6,7 While didactic content for LA is the same for both dental and dental hygiene students, attitudinal differences regarding whether dental hygienists are qualified to administer LA vary. Gutmann et al. studied dental and dental hygiene students following a didactic LA course and found that while these students were educated together in the same class, the dental students felt the dental hygiene students were not adequately prepared to administer LA.8 Other concerns related to the administration of LA identified in this study were in regard to causing patient discomfort, which was similar in both groups. In regard to concerns related to causing patient harm or having an LA related medical emergency, the dental hygiene students reported having less anxiety than their dental student cohorts.8
Medical emergencies and complications related to the administration of LA were the focus of an observational study by Brand et al.9 A total of 103 patients received a mandibular block injection by either an oral/maxillofacial surgeon, an oral/maxillofacial resident, or a dental student. No differences were identified in the frequency of LA reactions and/or complications across the three groups. The most common observed reactions among patients was feeling tense (41.7%), clenching fists (14.5%), moaning (12.6%), turning pale (7.8%), and reacting to needle contact with a nerve (3.8%).9 Brand et al. concluded that the administration of LA resulted in a limited number of side effects and that a thorough health history is the most effective way to identify individuals at increased risk for LA complications.9
A variety of training models are used to teach the administration of LA. Simulation models may be used prior to the first live patient, often student to student, injection. Results from a second study by Brand et al. demonstrated that students who had their initial experience administering LA on a training model did not differ in their self-opinions regarding their ability to administer LA over the control group. However, the student partner recipients of the injection reported that the experimental group appeared to be significantly calmer than the control group and that the injection was less painful.10 Chandrasekaran et al. examined pre-clinical dental student anxiety levels towards administering and receiving an LA injection. Participants had neither administered nor received an LA injection from a student. Study results demonstrated that 40% of the student operators felt they could not make the patient comfortable and approximately 43% were unable to locate the insertion point and felt the need for additional supervision. Anxiety was common for both operators (46%) and recipients (51%) and nearly half of the students indicated a preference for some type of pre-clinical training model prior to the first student to student injection.11
The CODA authorizes the individual state regulatory bodies to determine the requirements for licensure in LA.6,7 In the state of California, the Dental Board of California (DBC) sets the requirements for dentistry while the Dental Hygiene Committee of California (DHCC) regulates dental hygiene programs. Standards set by these regulatory bodies for dentistry and dental hygiene vary greatly. DBC mandates only that competency in LA be demonstrated for dental licentiates; alternately, the DHCC has specific regulations for LA in place in regard to the educational requirements.12
These requirements include:
• Thirty hours of instruction (15 didactic/preclinical and 15 clinical)
• Injection types: anterior nerve block, middle superior alveolar nerve block, anterior middle superior nerve block, posterior superior alveolar nerve block, greater palatine nerve block, nasopalatine nerve block, supraperiosteal, inferior alveolar nerve block (including Gow-Gates didactically only), lingual nerve block, buccal nerve block, mental nerve block, incisive nerve block, intraseptal
• Two injections of each type on another student during pre-clinical instruction
• Four clinical experiences per injection on four different patients (one of which may be another student)
• Competency evaluation of 75% or greater.
With respect to the variations in requirements for dental students versus dental hygiene students by state regulatory bodies in the state of California and the limited research regarding standard clinical teaching methods for LA, the purpose of this study was to determine if there was a difference in educational preparation and practical experiences between dental students and dental hygiene students in the administration of LA and management related complications.
Methods
This study was approved by the Human Subjects Committee, Institutional Review Board of Idaho State University (IRB- FY2017-101). A mixed methods approach consisting of a computer-based descriptive survey, a telephone interview and a comparative checklist was used to address the research questions. The checklist allowed for a comparison of LA course syllabi to the regulatory requirements, while the survey provided a means to gather more in-depth information about LA course content. The interview explored faculty perceptions regarding differences between dental and dental hygiene programs regarding LA didactic and clinical education.
The key study variables included LA course competencies, clinical administration requirements, didactic hour requirements, instructional experiences, practical experiences, and required competency-based performance evaluations for graduation. Additional variables included instructors' attitudes related to the instruction in dental and dental hygiene schools and the administration of LA by dental hygienists in clinical practice settings.
Program directors from the 6 dental schools and 29 dental hygiene programs in California received an email describing the study. Course instructors responsible for teaching LA were identified by the program director and invited to participate in the study. In the event the LA course instructor was unable to participate, the program director was invited to participate. Three reminders were sent to encourage participation and two $50 Amazon gift cards served as incentives for completion of the survey. Access to the Qualtrics® (Provo, UT) online survey was given after informed consent was received.
The self-designed survey was evaluated for validity and reliability prior to data collection. Validity was established using a 4-point Content Validity Index (CVI).13 Five dental hygiene instructors with LA teaching experience were asked to rate each item for relevance using the CVI. Reliability was obtained using a test/retest method with a different group of dental hygiene instructors; 100% agreement was obtained. Modifications to the survey were made based on CVI and reliability scores, and feedback received from the content experts.
Individuals completing the survey were given the option of participating in a follow-up, phone interview scheduled at a mutually convenient time. Semi-structured interviews lasting approximately fifteen minutes were conducted and notes transcribed. The third phase of the study involved a review of the LA course syllabus. A separate email was sent to program directors and LA course instructors requesting a copy of the course syllabus. Syllabi were analyzed for similarities and differences and compared to a checklist based on the literature and regulations governing the administration of LA in the state of California.7,14,15
Results
Eighteen course instructors or program directors participated in the study for a response rate of 51%. One respondent was from a dental school while 17 were from dental hygiene programs. The original intent of this study was to make comparisons between dental and dental hygiene programs regarding LA didactic and clinical teaching methods. However, given the low dental school response (n=1), inferential statistics were not calculated and results are limited to descriptive statistics.
Local Anesthesia Survey
Survey respondents from the dental hygiene programs were primarily female (82%) program directors (65%) ranging in age from 35-54 years (71%), and a little less than half (47%) had been teaching for less than ten years. In comparison, the dental school respondent had taught LA for over 20 years.
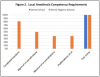
In addition to demographic questions, the survey consisted of items related to LA curriculum including competency evaluation. Test scores were utilized by all dental hygiene program respondents (n=17). Additional evaluations included observations of the administration LA injection types (n=13, 77%). The dental school respondent reported using both didactic and clinical examination scores. In regard to types of educational experiences provided during LA instruction, 88% of the dental hygiene respondents (n=15) reported using visual or audiovisual aids and 77% (n=13) reported using inanimate object (fruit) injection experiences prior to the first live patient injection. The dental school respondent reported using visual or audiovisual aids in LA instruction. Simulation models were used by several participants (n=2), with 12% indicating using a simulator model when teaching all types of injections. LA instructional experiences are shown in Figure 1. Required elements for student competencies are shown in Figure 2.
Participants were surveyed regarding the particular types of intraoral injections taught in the LA course. Sixteen of the 17 dental hygiene respondents reported teaching 12 types of intraoral injections; one participant noted that the Gow-Gates and the anterior middle superior alveolar nerve block injections were not taught in their curriculum. The dental school participant indicated teaching seven types of intraoral injections. In addition, the dental school required fewer student-to-student injections per type (n=7) than the dental hygiene schools (n=12). Results of the numbers of student-to-student injections administered as part of the dental and dental hygiene program educational experience are shown in Table I. Respondents were asked how many student-to-patient experiences were required prior to graduation. The majority of dental hygiene programs required three or more injections (student to patient) of each type. The dental school respondent reported there were no set number of student-to-patient injections required for graduation.
In regard to the types of procedural safety measures for LA taught, all participants (both dental and dental hygiene) indicated students performed a complete review of the patient's medical, dental, and drug history, determined any premedication needs, selected the appropriate type of LA, determined specific injection(s) and insertions site(s), prepared the injection site with topical anesthetic, aspirated prior to depositing the anesthetic, aspirated on more than one plane, deposited the anesthetic solution slowly, and evaluated the adequacy of the anesthesia.
A little more than half of all respondents (dental school n=1; dental hygiene program n=9) indicated students received between 1 to 5 hours of didactic instruction in the management of local or systemic complications and a little more than a quarter (29%) of the dental hygiene program respondents (n=5) reported their students received 16 or more hours of instruction. In addition, the majority of the respondents from the dental hygiene and the dental school indicated that management of systemic and local complications of LA were also covered in other courses including pharmacology, dental emergencies, advanced clinical dental hygiene, periodontics, and pain control.
Respondents were asked questions pertaining to management of local and systemic complications. A local complication was defined as being localized to the region where the anesthetic was administered and included facial nerve paralysis, hematoma, needle breakage, paresthesia, pain on injection, post-anesthetic intraoral lesion, sloughing of tissues, soft tissue injury, or trismus. A systemic complication was defined as a reaction following the administration of LA and included allergic responses or overdoses. When presented with a complication (systemic or local) the students' roles in management were to alert the instructor, observe and stay with the patient, explain the situation to the patient, provide post-op instruction, and monitor vital signs.
Regarding the frequency of systemic complications associated with LA in their respective programs, 53% of dental hygiene respondents (n=9) reported no systemic complications occurring per semester while 35% (n=6) reported 1-5 complications. In terms of local complications, 35% of the respondents indicated no local complications occurred per semester, 47% (n=8) reported 1-5 complications and 6% (n=1) indicated 11 or more local complications. Two dental hygiene participants and the dental school participant gave no response to the questions regarding complications.
Participants were asked whether students were allowed to administer LA unobserved after a specific number of injections had been demonstrated. Thirty-five percent (n=6) of the dental hygiene program respondents indicated that students could deliver LA independently after a specific number of successful injections had been observed while 53% (n=9) did not allow students to provide LA unobserved. Two dental hygiene participants and the dental school participant gave no response to the questions regarding unsupervised administration of LA.
Semi-structured Interview
Five individuals associated with dental hygiene programs agreed to participate in the qualitative portion of the study. Participants had been at their respective institutions between 2 to 23 years; one participant was a program director who was not currently teaching LA. Two participants had experience teaching in both dental and dental hygiene education programs and one was a former dental hygienist who is currently a dentist.
Participants' interpretation of the definition of direct supervision ranged from "the dentist is in the facility, but not in the operatory" to "the dentist is present from the beginning to the end of the procedure." When discussing the topic of direct supervision of LA for practicing dental hygienists, four of five participants indicated feeling it was not essential for a dentist to directly observe the administration of LA. Four of five individuals responded that they believed licensed dental hygienists are able to safely administer LA under general supervision. One participant indicated having concerns regarding patient safety and stated, "although the hygienist is prepared to administer LA, they are not prepared to treat the complications that result."
When questioned whether they perceived major differences between LA education and preparation in dental versus dental hygiene educational settings, four of the five individuals indicated that more time was spent on student to student injections in laboratory settings in dental hygiene programs. One participant stated, "many of the dental schools have moved away from partner practice. They watch a video, go over landmarks, but they never actually practice on a partner. Alternately, most dental hygiene programs are required to administer injections repeatedly. After teaching in a hygiene school, dentists share their kudos for the hygiene programs and if they had that same training, they would have felt much more confident." Conversely, one participant felt that "dental students have a stronger understanding of reactions and receive more training in how to handle emergencies and emergency procedures than in hygiene school."
Participants were asked if direct supervision of dental hygienists should continue to be a requirement even if dental and dental hygiene students are taught LA theory and practice a comparable level. Four of five participants did not believe direct supervision of the licensed dental hygienist was necessary. They stated that in the event of a medical emergency, both dentists and dental hygienists would follow the same protocol and initiate the EMS system. One participant was concerned that "dental hygienists may not be trained in how to handle the emergencies that can result" while another individual stated, "the dentist and hygienist are trained in all aspects of LA including not only technique, but also in emergency response."
Syllabus Checklist
Four participants provided syllabi for their program's LA course. The course syllabi were compared using a checklist to identify additional information about learning outcomes, methods of instruction, and evaluation not revealed in the survey. Each of the syllabi included learning outcomes pertaining to preventing, recognizing, and managing medical emergencies related to LA administration; identifying the need for and correct type of anesthetic based on medical history and the procedure; identifying the injection type for the specific procedure; and, performing injections to a minimum competency of 75% or higher. Instructional methods varied and included lecture, discussion, case studies, online and laboratory exercises, peer learning exercises, journal articles and a research project on one injection. Evaluations consisted of examinations, laboratory and homework assignments, and online modules.
Discussion
Results of this study demonstrated dental hygiene students within California were educationally prepared to select the appropriate injection sites, employ the correct techniques, and manage complications and safety issues for the administration of LA. Competencies in these areas were reflected in the course syllabi provided and noted on the LA checklist. Course requirements also reflected and, in some areas, surpassed CODA Standards.6,7 Dental hygiene students in California had more institutional requirements related to student-to-student and student-to-patient LA experiences and there were few local and systemic complications noted, which was similar to findings reported in previous studies.2,9,16
Considering the LA education requirements of dental hygiene students in California, most dental hygiene faculty members were in favor of general supervision for LA administration for licensed dental hygienists. While reporting of adverse LA events is rare, dental hygienists have the same requirements for cardiopulmonary resuscitation as their dentist counterparts and would have the same responsibilities for activating the emergency medical system. There are no reports in the literature of dental hygienists being unsafe while administering LA, and the evidence does not support the subjective concerns expressed in the interviews in this study.2,8,9,16
The overall level of the educational experience dental hygiene students receive in California prepares them to work in a general supervision environment in private practice. The delivery of LA, the use of nitrous oxide oxygen analgesia and soft tissue curettage are the only designated duties requiring direct supervision for dental hygienists in California.15 General supervision would permit dental hygienists to provide comprehensive preventive and therapeutic care for patients without the limiting requirement of the prescribing dentist's physical presence in the practice setting.
Results of this study are limited to dental hygiene programs in California and cannot be generalized to other states. The low response rate from the 6 dental schools, in spite of multiple contacts, limited the ability to make any significant comparisons between dental and dental hygiene programs. The use of a self-designed survey is an additional limitation. In general surveys are limited as they may lack depth and securing a high response rate may be difficult to control.17 In order to balance these limitations, a CVI and reliability testing were used, and sections of the survey were available for open ended comments. Semi-structured interviews and syllabi checklists were also incorporated research protocol.
Additional studies focused on dental hygienists and LA should be considered. Broadening this study would provide a greater understanding on the depth and breadth of LA education and experiences dental hygiene students are required prior to licensure for clinical practice. It would also be valuable to include more dental schools in the study perhaps with a dentist educator as a co-investigator to achieve a higher response rate. Further research should continue to explore the use of simulation models in reducing student anxiety and increasing confidence levels and qualitative studies should be conducted among dental hygienists administering LA to understand their experiences working within various supervision levels.
Conclusion
This study examined the LA educational experiences of dental and dental hygiene students in California using surveys, interviews and a course syllabus checklist. Dental hygiene students in California appear to have comparable or enhanced LA education experiences as compared to the dental school surveyed in this study. Dental hygiene students in California programs appear to be well prepared through their education experiences to administer and manage complications related to local anesthesia and evidence suggests dental hygienists may be prepared to safely administer LA under general supervision. Consideration should be given to supporting changing the supervision requirements for the administration of local anesthesia by dental hygienists licensed in the state of California.
About the Authors
Anna N. Teeters, RDH, MS is an instructor in the Department of Dental Hygiene, Taft College, Taft, CA.
JoAnn R. Gurenlian, RDH, MS, PhD is a professor and graduate program director; Jacqueline Freudenthal, RDH, MHE is an associate professor and chair; both are in the Department of Dental Hygiene, Idaho State University, Pocatello, ID.
Corresponding author: Anna N. Teeters, RDH, MS; ateeters@taftcollege.edu
References
1. American Dental Hygienists' Association. Local anesthesia administration by dental hygienists' state chart. [Internet]. Chicago: American Dental Hygienists' Association; 2016 Dec [cited 2017 Oct 14]. Available from http://www.adha.org/sites/default/files/7514_Local_ Anesthesia_Requirements_by_State_0.pdf
2. Scofield JC, Gutmann ME, DeWald JP, Campbell PR. Disciplinary actions associated with the administration of LA against dentists and dental hygienists. J Dent Hyg. 2005 Winter;79(1):1-9.
3. American Dental Hygienists' Association. Dental hygiene practice act overview: Permitted functions and supervision levels by state [Internet]. Chicago: American Dental Hygienists' Association; 2017 Jun [cited 2017 Oct 14]. Available from https://www.adha.org/resources-docs/7511_Permitted_Services_Supervision_Levels_by_State.pdf
4. California Code of Regulations. Definitions, Title 16 C.C.R., Div. 10, Stat. 1067 (2017).
5. Rich SK, Smorang J. Survey of 1980 California dental hygiene graduates to determine expanded-function utilization. J Public Health Dent. 1984 Winter;44(1): 22-7.
6. Commission on Dental Accreditation. Accreditation standards for dental education programs [Internet]. Chicago: American Dental Association; 2017 Aug [cited 2017 Oct 14]. Available from http://www.ada.org/~/media/CODA/Files/2016_predoc.ashx
7. Commission on Dental Accreditation. Accreditation standards for dental hygiene education programs [Internet]. Chicago; American Dental Association; 2017 Aug [cited 2017 Oct 14]. Available from http://www. ada.org/~/media/CODA/Files/2016_dh.ashx
8. Gutmann ME, DeWald JP, Solomon, E, McCann, AL. Dental and dental hygiene students' attitudes in a joint local anesthesia course. Probe 1997 Sep- Oct;31(5):165-70.
9. Brand HS, Bekker W, Baart JA. Complications of local anesthesia. An observational study. Int J Dent Hyg. 2009 Nov;7(4):270-2.
10. Brand HS, Baart JA, Maas NE, Bachet I. Effect of a training model in local anesthesia teaching. J Dent Edu. 2010 Aug;74(8):876-9.
11. Chandrasekaran B, Cugati, N Kumaresan, R. Dental students' perception and anxiety levels during their first local anesthetic injection. Malays J Med Sci. 2014 Nov- Dec;21(6):45-51.
12. California Code of Regulations. RDH course in local anesthesia, nitrous oxide/oxygen analgesia and periodontal soft tissue curettage. Title 16 C.C.R., Div. 11, Stat. 1107 (2017).
13. Wynd CA, Schmidt B, Schaefer MA. Two quantitative approaches for estimating content validity. West J Nurs Res. 2003 Aug;25(2):508-18.
14. Sisty-LePeau, N, Henderson, WG, Martin, JF. The administration of local anesthesia by dental hygiene students. J Dent Hyg. 1986 Oct;60(1):28-32.
15. RDH duties and settings. Title 16 C.C.R., Div. 10, Stat. 1088 (2017).
16. Anderson JM. Use of local anesthesia by dental hygienists who completed a Minnesota CE course. J Dent Hyg. 2002 Winter;76(I):35-46.
17. Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003 Jun;15(3):261-6.