You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Since the introduction of implant osseointegration by Brånemark in the 1960s, the use of implant-supported restorations as a treatment option as opposed to conventional prosthodontic restorations has increased, especially in completely edentulous arches.1 While long-term clinical studies have been published that demonstrate the success of dental implant-supported restorations,1-3 most studies document implant-supported prostheses' survival and success rates on a relatively short- or medium-term basis. Patients may have concerns about the risks and successful long-term outcomes of implant-supported prostheses when presented with a choice between them versus conventional restorative options.4,5
In full-arch edentulous patients, treatment options for provisional restorations include extraction of hopeless teeth followed by use of a complete removable denture; sequential extraction of hopeless teeth and retention of questionable teeth to use as abutments for fixed prostheses; or extraction of hopeless teeth and use of transitional implants (TIs) as abutments for fixed provisional prostheses. TIs are narrow-diameter implants (1.8 mm to 2.4 mm)6 that can be used as abutments, allowing patients undergoing bone/soft-tissue augmentation procedures to function with fixed provisional restorations rather than removable complete dentures. Clinically, this enables non-loaded healing of augmented soft and hard tissues following implant placement. Moreover, with the use of a fixed temporary restoration, the clinician and patient can assess function and esthetics prior to the fabrication of the final fixed restoration.7,8
Fixed hybrid screw-retained restorations supported by implants have been shown to be a highly predictable treatment option for restoration of an edentulous arch, offering simplicity of use, reduced cost, and ease in reparability.9 The purpose of this long-term clinical case report is to describe the steps involved in transitioning from an edentulous maxilla with hopeless teeth to a full-arch implant-supported denture using TIs to support the provisional prosthesis. It presents the diagnosis, treatment planning, and sequence of therapy of a fully edentulous maxilla and partially edentulous mandible with implant-supported prostheses. An assessment of the 20-year follow-up, implant survival rates, and marginal bone loss is also provided.
Case Report
Diagnosis and Treatment Plan
In 1998, a 57-year-old female patient presented to the Ashman Department of Periodontology and Implant Dentistry at New York University College of Dentistry (NYUCD) with the chief complaint of, "My teeth are mobile, and I don't want to wear anything removable in my mouth." Her medical history was unremarkable. She was a nonsmoker and nondrinker. Her past dental history included loss of several teeth due to periodontal disease and caries.
Clinical and radiographic examinations were carried out and revealed multiple missing teeth, nonrestorable teeth, periodontal disease, and bone loss (Figure 1 and Figure 2). The final treatment plan that was then proposed to and accepted and signed by the patient included extraction of all remaining teeth in the maxilla, delivery of a provisional fixed restoration supported by six transitional implants, bilateral sinus augmentation, placement of eight to 10 conventional implants, and an implant-supported porcelain-fused-to-metal or hybrid (screw-retained) restoration. For the mandible, the plan included extraction of teeth Nos. 29 and 32 and placement of implants in sites Nos. 18, 19, 20, 29, 30, and 31, with three splinted implant-supported fixed crowns on each side. The patient, however, decided to proceed only with the maxillary restoration and have the mandibular implants and restorations done in private practice.
Provisionalization
Preliminary impressions of both arches with alginate and a bite registration were taken. A wax-up was made to fabricate first a chairside maxillary fixed provisional using the remaining maxillary teeth as abutments, and subsequently a laboratory-processed maxillary fixed provisional using TIs in sites Nos. 3, 5, 8, 9, 12, and 14, and using hopeless teeth Nos. 6, 11, and 16 as abutments. This wax-up was also used to fabricate maxillary radiographic and surgical stents. The patient was referred for a computerized axial tomographic (CAT) scan.
Placement of Transitional Implants
Teeth Nos. 10, 14, and 15 were extracted after achieving local anesthesia (2% lidocaine with 1:100,000 epinephrine, Henry Schein Dental). Teeth Nos. 6, 11, and 16 were retained as temporary abutments for the provisional. A midcrestal incision was made with a 15C blade, and a full-thickness flap was reflected with a periosteal elevator. Osteotomies were created with a 1.3-mm pilot drill at sites Nos. 3, 5, 8, 9, 12, and 14 using a surgical stent. Six TIs (Dentatus MTI™, Dentatus) were placed using a right-angle handpiece driver and then tightened manually with the winged socket key (Figure 3).
Gingival protective plastic spacers were placed over the squared TI heads to prevent flowing acrylic or composite from interlocking into the wider implant heads (onto the assembly). A titanium connective bar was inserted through the TI grooves facing upward, passing palatally to remaining tooth No. 6, through the palatal cusp of tooth No. 11 and through the central fossa of tooth No. 16, and aligned to follow the contour of the edentulous ridge (Figure 4). Modular copings were placed over the TIs/TI bar in a clamp-like approach, engaging the gingival protective spacers (Figure 5).
Acrylic resin was then added to the metal bar. The bar was removed to verify a parallel path of insertion and then placed back into the proper position. The maxillary fixed provisional prosthesis was relined with acrylic over the metal bar, abutments, and TIs (Figure 6). The titanium bar was incorporated into the transitional provisional prosthesis. The patient was instructed to close into a previously determined vertical dimension of occlusion until polymerization of the reline material occurred.
Primary closure was achieved with silk sutures. Periapical radiographs were procured, and postoperative instructions were given to the patient, who was prescribed an antibiotic (amoxicillin 500 mg every 8 hours for 1 week), analgesic (ibuprofen 600 mg every 8 hours as needed), and mouthrinse (0.12% chlorhexidine for 10 days) (Peridex™, 3M Oral Care). The provisional prosthesis was adjusted and cemented with carboxylate cement (Durelon™, 3M Oral Care). The healing process was uneventful, with no infection, inflammation, or pain.
Sinus Augmentation
One month later, right and left sinus augmentation procedures were performed using a lateral window approach. The provisional prosthesis was removed prior to the surgical procedures. Midcrestal, mesial, and distal vertical incisions were made, and full-thickness flaps were elevated to expose the lateral wall of the maxillary sinuses. A surgical high-speed round bur with copious irrigation was used to create the lateral windows. The Schneiderian membranes were elevated, and the maxillary sinuses were filled with bone-graft material (Bio-Oss® large particles, Geistlich Pharma North America) and a collagen membrane (Bio-Gide®, Geistlich Pharma North America) was contoured and placed over the windows. Primary closure was achieved with silk sutures.
Postoperative instructions were given to the patient, and the same medications as previously described were prescribed again. A panoramic radiograph was taken (Figure 7). The provisional prosthesis was adjusted and recemented. The healing process was uneventful, with no infection, inflammation, or pain.
Implant Surgeries
Nine months after bilateral sinus augmentation, the TI at site No. 3 was removed and three implants (Straumann® ITI SLA®, 4.1 mm x 12 mm, Straumann) were placed in sites Nos. 2, 3, and 4. Following extraction of tooth No. 6, one additional implant (Biomet 3i™, 3.25 mm x 13 mm, Zimmer Biomet) was placed with an immediate placement protocol using a surgical guide and a torque of 35 Ncm. A cover screw was placed on implant No. 6, and healing abutments were placed on the other three implants. Two weeks later, the TI on site No. 14 was removed and one implant (Biomet 3i, 5 mm x 15 mm) was placed in site No. 11 with an immediate placement protocol, and two implants (Straumann ITI SLA, 4.1 mm x 12 mm) were placed in sites Nos. 13 and 14 using a surgical guide with a torque of 35 Ncm. A cover screw was placed on implant No. 11 and healing abutments were placed on implants Nos. 13 and 14. Tooth No. 16 was then extracted under the same local anesthesia used previously.
Three weeks later (Figure 8), an impression was taken (Figure 9) for a laboratory-processed, screw-retained, implant-supported provisional prosthesis. Six months later, the TIs on sites Nos. 5, 8, 9, and 12 were removed, and two implants (Biomet 3i, 3.25 mm x 13 mm) were placed in sites Nos. 8 and 10 using a surgical guide. Cover screws were then placed (Figure 10). The fixed laboratory-fabricated provisional prosthesis was screwed in on implants Nos. 2, 3, 4, 13, and 14 (Figure 11). After 4 months, the patient presented with uneventful healing, and second-stage surgery was performed on implants Nos. 6, 8, 10, and 11 (Figure 12).
Prosthetic Phase
A final impression was made (Figure 13). Interocclusal registration also was taken, and a facebow was recorded. A buccal matrix and teeth set-up were fabricated to evaluate the available space for the final prosthesis, as well as occlusion, esthetics, and phonetics. Custom abutments were screwed in on implants Nos. 6, 8, 10, and 11, and octa abutments were screwed in on implants Nos. 2, 3, 4, 13, and 14. The fit was verified by periapical radiographs. Metal frames (one anterior section and two posterior sections) were tried-in for passive fit, a bite registration was recorded, and a pick-up impression was performed. Two interlocks, one in each extremity of the anterior segment, were included (Figure 14).
The implant-supported, screw-retained, hybrid acrylic complete denture in the maxilla and the mandibular implant fixed prostheses were delivered after torquing the custom abutments to 32 Ncm and the octa abutments to 35 Ncm, and metal frames, including the interlocks, were tried-in. After consensus was obtained on the phonetics, occlusion, and esthetics (Figure 15), the fit was verified by periapical radiographs. The patient, who was very satisfied with the result, was instructed in proper oral hygiene.
Follow-up
Follow-up appointments were scheduled at 1 week, 2 weeks, 4 weeks, 6 months, and 1 year post insertion. Radiographs and clinical examinations showed peri-implant soft tissue and marginal bone levels, and the prostheses were stable (Figure 16). Oral hygiene instructions were reinforced, and maintenance was scheduled every 3 to 6 months. At the 5-year follow-up visit, the patient exhibited excellent peri-implant soft-tissue health, stable marginal bone levels, and good stability of prostheses (Figure 17).
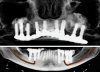
In 2020, the patient presented to the NYUCD Periodontology and Implant Dentistry Clinic. A clinical examination and radiographic evaluation showed that the patient's maxillary arch still exhibited good peri-implant soft-tissue health and stable marginal bone level with slight bone loss on implants Nos. 2, 6, 8, and 11 (Figure 18 through Figure 20). The maxillary prosthesis showed adequate stability with a slight chipped suprastructure on the porcelain on the right side. The patient was advised to substitute the implant-supported, screw-retained hybrid acrylic complete denture in the maxilla with a fixed, implant-supported, screw-retained prosthesis, which she declined due to financial considerations.
Discussion
Rehabilitation of patients who refuse to wear an immediate/interim complete removable denture during the healing process is a challenge. Correct diagnosis, accurate implant planning, and multidisciplinary teamwork are keys to ensuring successful results. The psychosocial impact of having to use a removable denture has been well-documented to have a strong effect on these patients, their oral condition, and their choice of dental interventions that comprise fixed prostheses rather than removable ones.9,10
According to histological studies, TIs can achieve successful osseointegration even when immediately loaded.11,12 Moreover, one study reported that 55% of TIs had torque values over 20 Ncm, which is considered a successful osseointegration.13 In the present case, TIs provided long-term stability, function, and esthetics while other treatment procedures were being carried out and osseointegration of the permanent implants was taking place.
The advantages of using TIs for screw-retained provisional restorations include: an improved healing of extraction sites or alveolar ridge augmentation by preventing premature functional and nonpremature loading; the avoidance of transmucosal loading during the sinus augmentation healing period; and support of the fixed provisional restorations as well as maintenance of the vertical dimension of occlusion. This may solve the problem of loosening of fixed provisional restorations caused by cement washout. The TI-supported provisionals are retrievable without damaging the prostheses. Technical and biological complications can be treated easily compared to cement-retained provisionals, which is why screw-retained provisionals are preferable.6,8,14 Provisional restorations based on ideal prosthetic wax-ups allow for esthetic modifications of teeth and tissue during the healing period. The patient can participate in selecting the color and size of their teeth, which in turn can be easily modified during the temporary restorative phase. This allows the patient to envision the final esthetic result. TIs also allow fixation of the surgical template during implant placement.4,5,7,8
Several disadvantages of using TIs should be noted, however. Excessive forces on TIs in poor bone quality may result in fracture or interfere with the osseointegration of the TIs. A minimum of 7 mm of bone and 6 mm to 7 mm of occlusal space (4 mm abutment component and 2 mm coping and restoration material) are required. Also, proximity of the TIs to the permanent implants may interfere with osseointegration of those implants. Increased cost and chairtime as well as the possibility of fracture during removal are also potential factors.4,5,7,8
Overall, TIs can be a valuable adjunct to implant treatment. They enable successful osseointegration while patients remain in a fixed functional provisional restoration throughout the treatment period. Although TIs were designed to be used on a short-term basis, they have been shown to remain in function for rather long periods of time.15,16 In the presented case report, the TIs lasted in function for up to 18 months.
Implant-supported acrylic hybrid prostheses for full-arch reconstruction have been used for a long time with high survival and success rates of both implants and prostheses. The most common problem with this type of prosthesis is technical prosthetic complications, especially chipping of acrylic teeth or fracture in the posterior areas. These complications increase when the opposing arch comprises a natural dentition or implant-supported fixed prosthesis. This complication was experienced in the present case report, as the patient, being in function with the hybrid restoration for 20 years, showed areas of chipping of the acrylic. Acrylic hybrid prostheses, however, are less costly, can achieve the desired esthetics, and maintain function long-term.17-20
Dental implant follow-up/maintenance appointments are critical for the long-term success of implant treatment. Poor oral hygiene and lack of proper maintenance cause bacteria biofilm accumulation, which can lead to peri-mucositis (soft-tissue inflammation around dental implants) and, if not treated, progress to peri-implantitis (bone loss around dental implants). In addition, patients who previously had periodontal disease are more prone to peri-implant disease, which increases the importance of frequent recall visits. The patient must be highly motivated to maintain good oral hygiene and follow a strict maintenance appointment schedule.21-23
Conclusion
The clinical implication of the presented case report on maxillary full-arch rehabilitation and mandibular partial-arch reconstruction after being in function for 20 years is that dental implants can be successful over a long term when either an immediate or delayed protocol is used and whether or not bone augmentation is performed. Many patients present with high expectations for immediate and esthetic fixed restorations. However, such treatment is not always possible in situations where bone quantity and quality are poor and/or the number of existing abutments does not allow for immediate fixed temporization. In this case report, the incorporation of transitional implants was utilized to achieve immediate fixed temporization, satisfying the patient's needs as well as preventing transmucosal loading during the healing phases of sinus augmentation and implant placement.