You must be signed in to read the rest of this article.
Registration on CDEWorld is free. Sign up today!
Forgot your password? Click Here!
Tooth loss is a result of a multifactorial and often complex interaction of multiple comorbidities that, without sufficient intervention, may progress to complete edentulism.1 Traditionally, edentulism has been treated by fabricating removable, tissue-supported complete dentures.2 Optimal denture treatment involves three main factors: retention, stability, and support.3-5 Retention is related to a prosthesis's ability to resist the forces of dislodgment along its path of insertion or placement, whereas stability refers to a prosthesis's resistance to horizontal displacement.3,4,6 Support is the characteristic provided by the tissue surface of the mandibular edentulous ridge, and it is an important property that is related to the amount of surface area of the tissue that is in contact with the underlying structure of the prosthesis.5 Although it is difficult to measure the overall contribution of comfort and patient acceptance to optimal denture and overdenture function, when choosing between treatment approaches, patients often choose the treatment that best increases stability—even when cost is a major factor.7
Ensuring that a complete denture (or overdenture) achieves full adaptation to the edentulous ridge is an important technical characteristic of fabricating the prosthesis. The amount of surface area contact affects the viscosity and film thickness of the saliva, which also plays an important role in retention and stability of the prosthesis.8 Typically, as the surface area contact between the denture base and the soft tissue increases, the stability of the prosthesis on the edentulous ridge increases. When a prosthesis has areas of misfit, the chances of instability increase, and ulceration and sore spots may develop, potentially leaving patients with an increasingly difficult accommodation period.9
In addition to confirmation of surface area contact, the overall amount of edentulous ridge available has been correlated with the retention and stability of the denture. A combination of these factors has been implicated in patient satisfaction with a removable prosthesis.3,4,10 Common long-term maintenance of a removable prosthesis involves routine denture base adjustments.11,12 Because resorption of the residual ridge continues over time, it is important to ensure that a prosthesis has been fully adapted at the time of delivery to give the patient the best chance of having a successful outcome.13
Implant-Retained vs. -Supported
The delivery of implant-retained overdentures has long been regarded as a safe and highly effective long-term treatment option for edentulous patients.14-16 The placement of two to four dental implants for the purposes of retaining or supporting a removable prosthesis has been shown to be favorable for patients and has a long history of clinical use.17 Implants can be placed in either the anterior or posterior portions of the maxillary or mandibular arches; however, implants placed with a wider distribution and/or interimplant distance can result in improved retention and stability of the prosthesis.18,19 An implant overdenture prosthesis with stud-style abutments is referred to as an implant-retained overdenture because the attachment system imparts resiliency but permits slight movements with regard to the edentulous ridge. Overdenture prostheses utilizing these attachment systems rely heavily upon the soft tissue of the underlying edentulous ridge to provide support while the attachment system provides retention. This functionality is contrasted by that of implant-supported bar overdentures, which derive both their support and retention from the bar and attachment system. As a result, bar-retained overdenture solutions often have minimal tissue contact when compared with implant-retained overdentures.
Ensuring that an implant-retained prosthesis is fully adapted to the edentulous ridge is accomplished during clinical placement of the prosthesis at the delivery appointment. Regarding attachment processing, some clinicians advocate for a chairside approach as opposed to a laboratory approach in order to enhance the tissue contact of the prosthesis.20 Due to acrylic resin shrinkage that occurs at the time of processing, which can be significant, laboratory processed overdentures may present a higher risk of prosthetic misfit when compared with those that are processed chairside. In addition, clinicians can adjust the amount of prosthesis-tissue contact and the resulting tissue pressure during chairside processing of the housings/attachments. By holding the prosthesis in place with the desired amount of pressure or ensuring that the patient only closes lightly into centric relation, clinicians can ensure that processing procedures do not result in a prosthesis that overcompresses the tissues.
Before processing the housings/attachments utilizing a chairside approach, it is important to ensure that the prosthesis is fully adapted to the edentulous ridge. The following case report presents techniques that can be used to assess the adaptation of overdentures as well as protocols that can be used to adjust them prior to processing the housings/attachments in a clinical environment.
Case Report
A patient was referred to the practice by another clinician for the fabrication of a functional, stable prosthesis. He presented with four existing implants in the anterior mandible that were fitted with stud-style attachments (LOCATOR®, Zest Dental Solutions [alternatively: Stern SNAP®, Sterngold; OT Equator, Rhein83]) (Figure 1). The implants, which had been placed approximately 6 months prior, appeared healthy and well-integrated. An earlier attempt to fabricate an overdenture had resulted in an overextended prosthesis that rocked significantly. After multiple attempts to adjust the prosthesis, it had become excessively thin and ultimately fractured during function.
A consultation with the clinician who fabricated the failed prosthesis revealed that during the chairside processing of the attachment housings, the patient was instructed to close heavily into centric relation. Although this method can be successfully employed for some patients, in patients with soft tissues that demonstrate mobility, the clinician may inadvertently compress them. As a result, the patient can overload the soft tissues during the processing steps, which may lead to pressure areas within the prosthesis.
During several recall appointments, the overextended prosthesis in this case had been heavily adjusted, including removal of the flanges. Adjustments such as these are often made to suit patients' preferences. Many complain about prostheses engaging undercuts and the resulting sore areas. To placate these patients, some clinicians may take a heavy-handed approach and excessively adjust a prosthesis. For this patient, such modifications ultimately resulted in the removal of much of the supporting area of the prosthesis, which lead to an excessive amount of movement and fracture.
Ensuring that an implant-retained overdenture is properly adapted to the edentulous ridge starts at the initial appointment. When a patient has four well-spaced implants in the anterior mandible, they often provide an excellent opportunity for prosthetic stability. A challenge exists, however, when clinical and laboratory techniques to fabricate the prosthesis do not take into consideration the effect of the processing techniques upon the resulting prosthesis. In this case, multiple treatment options were presented to the patient, but he elected to proceed with the treatment plan involving restoration with a mandibular implant-retained overdenture.
Impression and Laboratory Techniques
Fabrication of a properly and completely adapted overdenture prosthesis first begins with the clinician and technician working together to create an optimal base. Typically, this will have as much surface area and contact with the edentulous ridge as possible while still maintaining physiologically derived borders that do not impinge upon the peripheral soft tissues and musculature.
Capturing an ideal impression can improve the fit of the denture base and overall clinical outcome of the final prosthesis. In this case, scan bodies (LOCATOR® Scan Bodies, Zest Dental Solutions [alternatively: 3Shape Scan bodies, 3Shape; Inclusive® Titanium Scan Body, Glidewell]) were placed onto each abutment and a digital impression was captured using an intraoral optical scanner (TRIOS®, 3Shape [alternatively: Element®, iTero; Planmeca Emerald™, Planmeca]) (Figure 2). The digital impression was inspected on the screen to ensure that it completely captured the edentulous ridge and the scan bodies. Next, a digital impression was made of the maxillary arch, and a third scan was performed to capture the interocclusal relationship of the two arches. A second optical impression of the mandibular arch with the patient's existing prosthesis was also captured to serve as a reference for the laboratory technician during fabrication of the new prosthesis. Finally, photographs of the patient's face in a smiling and relaxed position were acquired to assist the laboratory technician in optimizing the esthetics, midline, and phonetics of the final prosthesis.
Optical impression technology allows the clinician to capture the edentulous ridge and the soft tissues in a potentially relaxed and less-compressed state. Although there are challenges associated with capturing edentulous ridges using intraoral scanners, such as the complexity of the technology, limitations associated with the optical tracking of the scanning, and the difficulty of user techniques, the potential benefits may outweigh them. Scan bodies have been developed by implant manufacturers to assist in optical scanning techniques and can be utilized to help overcome some of these challenges. In addition, the use of scan bodies may provide the dental technician with an easier pathway for fabricating the prosthesis. One feature of an overdenture scan body is that it provides the ideal shape for the recessed spaces of the prosthesis through the shape of its body. By capturing a digital impression of the intraoral position of the scan bodies, the clinician greatly assists the technician in fabricating a digitally produced overdenture prosthesis because it automates the design of the recessed areas of the denture base within the prosthesis. This allows the clinician to simply place the prosthesis onto the edentulous ridge with minimal adjustments prior to placing housings and performing chairside processing techniques.
For this case, the digital impressions were imported into the laboratory's design software (Dental System, 3Shape [alternatively: DentalCAD, exocad; Planmeca PlanCAD®, Planmeca]), and the technician used them along with the photographs provided to design the prosthesis. The prosthesis was then fabricated from a PMMA disc (Ivotion™, Ivoclar Vivadent [alternatively: XCL™ Monolithic Puck, Avadent; BD Load®, Merz Dental]) using a subtractive manufacturing method in a milling machine (R5, VHF [alternatively: PrograMill PM7, Ivoclar Vivadent; Ceramill Motion 2, AmannGirrbach]). It was fabricated with ideally prepared recesses within the denture base simply by following the shape of the scan bodies on the optical impression. Because the patient had fractured his previous prosthesis, a cobalt-chrome metal framework was placed within the new overdenture.
Chairside Adjustments
The patient returned to the practice for chairside adjustments and delivery of the digitally produced overdenture. Prior to placing the attachment housings and performing any adjustments, the prosthesis was seated onto the patient's edentulous ridge to evaluate its general fit (Figure 3).
The prosthesis was then removed and air-dried, and denture disclosing media (Pressure Indicating Paste, Mizzy [alternatively: Pressure Disclosing Paste, Leemark Dental; Pressure Indicator Paste, Mark3]) was placed onto the entire intaglio surface using a brush (Figure 4). The paste was thoughtfully applied to the surface with emphasis on creating a linear streaked pattern (Figure 5). After the prosthesis is placed onto the edentulous ridge, any areas of contact between it and the denture-bearing surface can be rapidly visualized as disruptions in the streaked pattern.
Once the disclosing media was applied, the prosthesis was placed onto the patient's edentulous ridge using very light pressure. The clinician then placed three fingers on the occlusal surface of the prosthesis in the general area of the first molar regions and the central incisor positions. By placing fingers in these approximate positions, the clinician can evenly control the amount of simulated intraoral forces. Using moderate finger pressure, the clinician then pressed downward on the prosthesis in several motions: first, in an occlusal direction; second, in an anterior-posterior direction; and third, in an oblique direction (Figure 6). The temptation is to have the patient bite into centric relation or maximum intercuspation; however, doing so before making adjustments may result in a false assessment of the true pressure on the edentulous ridge.
Next, two fingers were used to evaluate the anteroposterior forces with one finger being placed on the anterior portion of the prosthesis in approximately the central incisor position and a second finger (on the opposite hand) placed in the molar region. Alternating finger pressure with moderate force will help identify areas where excessive tissue contact can cause a rocking sensation. The anteroposterior pressure simulates the dislodging force from the tongue pushing on the prosthesis during speaking and when it is protruded.18,19
Finally, one finger from each hand was placed onto the occlusal surface of the prosthesis in approximately the premolar position on each side. The clinician then pressed using alternating moderate finger pressure. This alternating molar pressure simulates the effect of the patient chewing a bolus of food, squeezing the lips, or pressing the tongue into the cheek during function.
After the simulation of intraoral forces, the prosthesis was carefully removed to prevent further displacement of the disclosing media. It was then inspected to visualize any areas of pressure contact (Figure 7). Excessive pressure due to occlusal forces results in a wide saucer-like displacement of the disclosing media (white arrows), and this is typically found in the areas of the retromolar pad, alveolar ridge crest, and immediately surrounding the implant attachment housings. Areas of excessive movement due to anteroposterior forces are often found in the peripheral areas surrounding the facial and lingual border portions of the anterior region of the prosthesis (green arrow). Excessive pressure areas caused by oblique dislodging forces are visualized by a lack of paste at the periphery of the prosthesis in the areas of the residual canine or premolar regions (blue arrow). Any areas where the streaked pattern is undisrupted on the intaglio surface of the prosthesis indicate an absence of tissue contact and the presence of space between the tissues and the denture base (yellow arrows).
Prosthetic adjustments to the areas of excessive pressure were made using acrylic burs to relieve the areas of paste displacement. First, any pressure areas caused by occlusal forces were adjusted by relieving the areas where heavy pressure was noted with a medium- to large-sized round bur using moderate speed and light force (Figure 8). The anteroposterior pressure areas were adjusted next, and the oblique pressure areas were adjusted last. Both of these pressure areas, which are typically visualized with longer, narrower areas of paste displacement, were adjusted with a tapering acrylic bur using low speed and moderate force. A highspeed handpiece with a large football-shaped carbide bur can assist in adjusting any areas where a metal framework is in excessive contact with the soft tissues.
After the initial adjustments were made, the brush used previously to initially place the disclosing media was utilized to return the streaked appearance to the existing paste within the intaglio surface of the prosthesis. Little to no additional disclosing media was introduced during subsequent brushstrokes and adjustments to keep the paste within the intaglio surface of the prosthesis thin. Excessive bulk of the disclosing media can result in false negative readings and lead to an insufficiently adjusted overdenture.
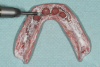
After subsequent adjustments to ensure complete adaptation of the prosthesis, the disclosing media exhibited a "splotchy" appearance similar to that of an orange peel (Figure 9). In addition, the streaked pattern was significantly minimized or eliminated, indicating that the prosthesis was intimately contacting the entire denture-bearing soft-tissue surface of the patient's edentulous ridge. The disclosing media was removed from the prosthesis using an alcohol-soaked gauze pad.
Once the abutment housings and block-out spacers for the attachment system were placed onto each abutment, the prosthesis was placed onto the edentulous ridge, and a passive fit over the housings was confirmed. The prosthesis was then removed from the mouth, and a vent hole was prepared into each recess using a bur. To process the attachments, a tissue-colored, dual-cure composite resin (CHAIRSIDE® Attachment Processing Material, Zest Dental Solutions [alternatively: Quick Up®, VOCO; Chairside Pick Up Material, Darby Dental Supply]) was placed into the prepared recesses, and the prosthesis was seated onto the edentulous ridge using light finger pressure. Similar to the simulated forces previously used to evaluate the adaptation of the prosthesis, the use of light pressure was to ensure that the prosthesis was passively seated onto the edentulous ridge without overcompressing the soft tissues.
After complete polymerization, the prosthesis was removed from the mouth and evaluated. Acrylic resin burs were used to trim up any areas of excess resin, and the prosthesis was polished. With the existing processing inserts still in place within the housings, additional disclosing media was placed onto the intaglio surface of the prosthesis in the same fashion employed earlier. Occlusal, anteroposterior, and oblique dislodging forces were again simulated using finger pressure, and the prosthesis was removed and inspected. Typically, no additional adjustments are needed if the prosthesis is processed using passive forces; however, in this case, any minor areas of excessive pressure were noted and adjusted prior to placing definitive inserts. In addition, articulating paper was used to confirm centric and occlusal contacts while the processing inserts were still in place.
The prosthesis was given a final polish using water and pumice, the processing inserts were removed, and the definitive inserts were placed (Figure 10). The prosthesis was placed onto the edentulous ridge and the retentive elements were engaged in order to confirm complete adaptation. Anteroposterior and oblique stability of the prosthesis was verified using finger pressure, and the patient was asked to stick out his tongue to verify that the prosthesis didn't excessively move or rotate. The patient was also instructed to close into centric occlusion to confirm occlusal stability of the prosthesis.
Prior to dismissal, the patient was provided with instructions regarding handling of the prosthesis, including insertion, removal, chewing, and maintenance. He stated that he was very satisfied with its final form and appearance.
Conclusion
The proper adjustment of implant-retained overdentures is a very important yet often underemphasized task that involves careful attention. A properly fitting restoration begins with an ideal impression, and the use of an intraoral scanner can help to improve accuracy for patients with soft tissues that demonstrate mobility. Ensuring that the base has been completely adapted prior to placing the retentive elements and housings is essential to eliminate the possibility of excessive movement under intraoral forces and will minimize the need for long-term maintenance of the prosthesis and maximize the intervals at which the retentive inserts are replaced.
Queries regarding this course may be submitted to authorqueries@aegiscomm.com
About the Author
Michael D. Scherer, DMD, MS
Fellow
American College of Prosthodontists
Assistant Clinical Professor
Loma Linda University School of Dentistry
Loma Linda, California
Private Practice
Sonora, California
References
1. Felton DA. Edentulism and comorbid factors. J Prosthodont. 2009;18(2):88-96.
2. Lang BR. A review of traditional therapies in complete dentures. J Prosthet Dent. 1994;72(5):538-542.
3. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete denture retention, stability, and support. Part I: retention. J Prosthet Dent. 1983;49(1):5-15.
4. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete dentures. Part II: stability. J Prosthet Dent. 1983;49(2):165-172.
5. Jacobson TE, Krol AJ. A contemporary review of the factors involved in complete dentures. Part III: support. J Prosthet Dent. 1983;49(3):306-313.
6. The glossary of prosthodontic terms. J Prosthet Dent. 2005;94(1):10-92.
7. Mericske-Stern R, Probst D, Fahrländer F, Schellenberg M. Within-subject comparison of two rigid bar designs connecting two interforaminal implants: patients' satisfaction and prosthetic results. Clin Implant Dent Relat Res. 2009;11(3):228-237.
8. Darvell BW, Clark RK. The physical mechanisms of complete denture retention. Br Dent J. 2000;189(5):248-252.
9. Kivovics P, Jáhn M, Borbély J, Márton K. Frequency and location of traumatic ulcerations following placement of complete dentures. Int J Prosthodont. 2007;20(4):397-401.
10. Critchlow SB, Ellis JS. Prognostic indicators for conventional complete denture therapy: a review of the literature. J Dent. 2010;38(1):2-9.
11. Ettinger RL, Qian F. Longitudinal assessment of denture maintenance needs in an overdenture population. J Prosthodont. 2019;28(1):22-29.
12. Kaufmann R, Friedli M, Hug S, Mericske-Stern R. Removable dentures with implant support in strategic positions followed for up to 8 years. Int J Prosthodont. 2009;22(3):233-241.
13. Tallgren A. The continuing reduction of the residual alveolar ridges in complete denture wearers: a mixed-longitudinal study covering 25 years. J Prosthet Dent. 1972;27(2):120-132.
14. Naert I, Alsaadi G, Quirynen M. Prosthetic aspects and patient satisfaction with two-implant-retained mandibular overdentures: a 10-year randomized clinical study. Int J Prosthodont. 2004;17(4):401-410.
15. Sadowsky SJ. Mandibular implant-retained overdentures: a literature review. J Prosthet Dent. 2001;86(5):468-473.
16. Scherer MD. Overdenture implants: a simplified and contemporary approach to planning and placement. Dent Today. 2015;34(8):54,56-58,60.
17. Reissmann DR, Enkling N, Moazzin R, et al. Long-term changes in oral health-related quality of life over a period of 5 years in patients treated with narrow diameter implants: a prospective clinical study. J Dent. 2018;75:84-90.
18. Scherer MD, McGlumphy EA, Seghi RR, Campagni WV. Comparison of retention and stability of implant-retained overdentures based upon implant number and distribution. Int J Oral Maxillofac Implants. 2013;28(6):1619-1628.
19. Scherer MD, McGlumphy EA, Seghi RR, Campagni WV. Comparison of retention and stability of two implant-retained overdentures based upon implant location. J Prosthet Dent. 2014;112(3):515-521.
20. Scherer MD. When to use laboratory vs. chairside processing of overdentures. Inside Dental Technology. 2021;12(5):16-23.